-
Start Preamble
Start Printed Page 72760
AGENCY:
Centers for Medicare & Medicaid Services (CMS), HHS.
ACTION:
Proposed rule.
SUMMARY:
This proposed rule addresses changes to the Medicare Shared Savings Program (Shared Savings Program), including provisions relating to the payment of Accountable Care Organizations (ACOs) participating in the Shared Savings Program. Under the Shared Savings Program, providers of services and suppliers that participate in an ACO continue to receive traditional Medicare fee-for-service (FFS) payments under Parts A and B, but the ACO may be eligible to receive a shared savings payment if it meets specified quality and savings requirements.
DATES:
To be assured consideration, comments must be received at one of the addresses provided below, no later than 5 p.m. on February 6, 2015.
ADDRESSES:
In commenting, please refer to file code CMS-1461-P. Because of staff and resource limitations, we cannot accept comments by facsimile (FAX) transmission.
You may submit comments in one of four ways (please choose only one of the ways listed):
1. Electronically. You may submit electronic comments on this regulation to http://www.regulations.gov. Follow the “Submit a comment” instructions.
2. By regular mail. You may mail written comments to the following address ONLY: Centers for Medicare & Medicaid Services, Department of Health and Human Services, Attention: CMS-1461-P, P.O. Box 8013, Baltimore, MD 21244-8013.
Please allow sufficient time for mailed comments to be received before the close of the comment period.
3. By express or overnight mail. You may send written comments to the following address ONLY: Centers for Medicare & Medicaid Services, Department of Health and Human Services, Attention: CMS-1461-P, Mail Stop C4-26-05, 7500 Security Boulevard, Baltimore, MD 21244-1850.
4. By hand or courier. Alternatively, you may deliver (by hand or courier) your written comments ONLY to the following addresses prior to the close of the comment period:
a. For delivery in Washington, DC—Centers for Medicare & Medicaid Services, Department of Health and Human Services, Room 445-G, Hubert H. Humphrey Building, 200 Independence Avenue SW., Washington, DC 20201
(Because access to the interior of the Hubert H. Humphrey Building is not readily available to persons without Federal government identification, commenters are encouraged to leave their comments in the CMS drop slots located in the main lobby of the building. A stamp-in clock is available for persons wishing to retain a proof of filing by stamping in and retaining an extra copy of the comments being filed.)
b. For delivery in Baltimore, MD—Centers for Medicare & Medicaid Services, Department of Health and Human Services, 7500 Security Boulevard, Baltimore, MD 21244-1850.
If you intend to deliver your comments to the Baltimore address, call telephone number (410) 786-7195 in advance to schedule your arrival with one of our staff members.
Comments erroneously mailed to the addresses indicated as appropriate for hand or courier delivery may be delayed and received after the comment period.
For information on viewing public comments, see the beginning of the SUPPLEMENTARY INFORMATION section.
Start Further InfoFOR FURTHER INFORMATION CONTACT:
Dr. Terri Postma or Rick Ensor, 410-786-8084, Email address: aco@cms.hhs.gov.
End Further Info End Preamble Start Supplemental InformationSUPPLEMENTARY INFORMATION:
Inspection of Public Comments: All comments received before the close of the comment period are available for viewing by the public, including any personally identifiable or confidential business information that is included in a comment. We post all comments received before the close of the comment period on the following Web site as soon as possible after they have been received: http://www.regulations.gov. Follow the search instructions on that Web site to view public comments.
Comments received timely will also be available for public inspection as they are received, generally beginning approximately 3 weeks after publication of a document, at the headquarters of the Centers for Medicare & Medicaid Services, 7500 Security Boulevard, Baltimore, Maryland 21244, Monday through Friday of each week from 8:30 a.m. to 4 p.m. To schedule an appointment to view public comments, phone 1-800-743-3951.
Table of Contents
To assist readers in referencing sections contained in this preamble, we are providing a table of contents.
I. Executive Summary and Background
A. Executive Summary
1. Purpose
2. Summary of the Major Provisions
3. Summary of Costs and Benefits
B. Background
II. Provisions of This Proposed Rule
A. Definitions
1. Proposed Definitions
2. Proposed Revisions to Existing Definitions
a. Definition of ACO Participant
b. Definition of ACO Professional
c. Definition of ACO Provider/Supplier
d. Definition of Assignment
e. Definition of Hospital
f. Definition of Primary Care Services
g. Definitions of Continuously Assigned Beneficiary and Newly Assigned Beneficiary
h. Definition of Agreement Period
B. ACO Eligibility Requirements
1. Agreement Requirements
a. Overview
b. Proposed Revisions
2. Sufficient Number of Primary Care Providers and Beneficiaries
a. Overview
b. Proposed Revisions
3. Identification and Required Reporting of ACO Participants and ACO Providers/Suppliers
a. Overview
b. Proposed Revisions
(1) Certified List of ACO Participants and ACO Providers/Suppliers
(2) Managing Changes to ACO Participants
(3) Managing Changes to ACO Providers/Suppliers
(4) Update of Medicare Enrollment Information
4. Significant Changes to an ACO
a. Overview
b. Proposed Revisions
5. Consideration of Claims Billed by Merged/Acquired Medicare-Enrolled Entities
a. Overview
b. Proposal
6. Legal Structure and Governance
a. Legal Entity and Governing Body
(1) Overview
(2) Proposed Revisions
b. Fiduciary Duties of Governing Body Members
(1) Overview
(2) Proposed Revisions
c. Composition of the Governing Body
(1) Overview
(2) Proposed Revisions
7. Leadership and Management Structure
a. Overview
b. Proposed Revisions
8. Required Process To Coordinate Care
a. Overview
b. Accelerating Health Information Technology Start Printed Page 72761
c. Proposed Revisions
9. Transition of Pioneer ACOs Into the Shared Savings Program
a. Overview
b. Proposed Revisions
C. Establishing and Maintaining the Participation Agreement With the Secretary
1. Background
2. Application Deadlines
a. Overview
b. Proposed Revisions
3. Renewal of Participation Agreements
a. Overview
b. Proposed Revisions
4. Changes to Program Requirements During the 3-Year Agreement
a. Overview
b. Proposed Revisions
D. Provision of Aggregate and Beneficiary Identifiable Data
1. Background
2. Aggregate Data Reports and Limited Identifiable Data
a. Overview
b. Proposed Revisions
3. Claims Data Sharing and Beneficiary Opt-Out
a. Overview
b. Proposed Revisions
E. Assignment of Medicare FFS Beneficiaries
1. Background
2. Basic Criteria for a Beneficiary To Be Assigned to an ACO
3. Definition of Primary Care Services
a. Overview
b. Proposed Revisions
4. Consideration of Physician Specialties and Non-Physician Practitioners in the Assignment Process
a. Overview
b. Proposed Revisions
5. Assignment of Beneficiaries to ACOs That Include FQHCs, RHCs, CAHs, or ETA Hospitals
a. Assignment of Beneficiaries to ACOs That Include FQHCs and RHCs
(1) Overview
(2) Proposed Revisions
b. Assignment of Beneficiaries to ACOs That Include CAHs
c. Assignment of Beneficiaries to ACOs That Include ETA Hospitals
6. Effective Date for Finalization of Proposals Affecting Beneficiary Assignment
F. Shared Savings and Losses
1. Background
2. Modifications to the Existing Payment Tracks
a. Overview
b. Proposals Related to Transition From the One-Sided to Two-Sided Model
c. Proposals for Modifications to the Track 2 Financial Model
3. Creating Options for ACOs That Participate in Risk-Based Arrangements
a. Overview
b. Proposals for Assignment of Beneficiaries Under Track 3
(1) Background
(2) Proposal for Prospective Assignment Under Track 3
c. Proposed Exclusion Criteria for Prospectively Assigned Beneficiaries
d. Proposed Timing of Prospective Assignment
e. Proposals for Addressing Interactions Between Prospective and Retrospective Assignment Models
f. Proposals for Determining Benchmark and Performance Year Expenditures Under Track 3
g. Proposals for Risk Adjusting the Updated Benchmark for Track 3 ACOs
h. Proposals for Final Sharing/Loss Rate and Performance Payment/Loss Recoupment Limit Under Track 3
i. Proposals for Minimum Savings Rate and Minimum Loss Rate in Track 3
4. Seeking Comment on Ways To Encourage ACOs Participation in Performance-Based Risk Arrangements
a. Payment Requirements and Program Requirements That May Need To Be Waived in Order To Carry Out the Shared Savings Program
(1) SNF 3-Day Rule
(2) Billing and Payment for Telehealth Services
(3) Homebound Requirement Under the Home Health Benefit
(4) Waivers for Referrals to Postacute Care Settings
(5) Waiver of Other Payment Rules
b. Other Options for Improving the Transition to Two-Sided Performance-Based Risk Arrangements
(1) Beneficiary Attestation
(2) Seeking Comment on a Step-Wise Progression for ACOs To Take on Performance-Based Risk
5. Modifications to Repayment Mechanism Requirements
a. Overview
b. Proposals for Amount and Duration of the Repayment Mechanism
c. Proposals Regarding Permissible Repayment Mechanisms
6. Seeking Comment on Methodology for Establishing, Updating, and Resetting the Benchmark
a. Background on Establishing, Updating, and Resetting the Benchmark
(1) Background on Use of National Growth Rate as a Benchmark Trending Factor
(2) Background on Use of National FFS Growth Factors in Updating the Benchmark During the Agreement Period
(3) Background on Managing Changes to ACOs During the Agreement Period
(4) Background on Resetting the Benchmark
(5) Background on Stakeholders' Concerns About Benchmarking Methodology
b. Factors To Use in Resetting ACO Benchmarks and Alternative Benchmarking Methodologies
(1) Equally Weighting the Three Benchmark Years
(2) Accounting for Shared Savings Payments in Benchmarks
(3) Use of Regional Factors (as opposed to national factors) in Establishing and Updating Benchmarks
(4) Alternative Benchmark Resetting Methodology: Hold the ACO's Historical Costs Constant Relative to Its Region
(5) Alternative Benchmark Methodology: Transition ACOs to Benchmarks Based Only on Regional FFS Costs Over the Course of Multiple Agreement Periods
(6) Seeking Comment on the Benchmarking Alternatives Considered and the Applicability of These Approaches
7. Seeking Comment on Technical Adjustments to the Benchmark and Performance Year Expenditures
G. Additional Program Requirements and Beneficiary Protections
1. Background
2. Public Reporting and Transparency
a. Overview
b. Proposed Revisions
3. Terminating Program Participation
a. Overview
b. Proposed Revisions
(1) Grounds for Termination
(2) Close-Out Procedures and Payment Consequences of Early Termination
(3) Reconsideration Review Process
(A) Overview
(B) Proposed Changes
(4) Monitoring ACO Compliance With Quality Performance Standards
III. Collection of Information Requirements
IV. Response to Comments
V. Regulatory Impact Analysis
A. Statement of Need
B. Overall Impact
C. Anticipated Effects
1. Effects on the Medicare Program
a. Assumptions and Uncertainties
b. Detailed Stochastic Modeling Results
c. Further Considerations
2. Effects on Beneficiaries
3. Effect on Providers and Suppliers
4. Effect on Small Entities
5. Effect on Small Rural Hospitals
6. Unfunded Mandates
D. Alternatives Considered
E. Accounting Statement and Table
F. Conclusion
Regulations Text
Acronyms
ACO Accountable Care Organization
BIPA Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000 (Pub. L. 106-554)
CAHs Critical Access Hospitals
CCM Chronic Care Management
CEHRT Certified Electronic Health Record Technology
CG-CAHPS Clinician and Group Consumer Assessment of Health Providers and Systems
CHIP Children's Health Insurance Program
CMP Civil Monetary Penalties
CMS Centers for Medicare & Medicaid Services
CNM Certified Nurse Midwife
CMS-HCC CMS Hierarchal Condition Category
CPT [Physicians] Current Procedural Terminology (CPT codes, descriptions and other data only are copyright 2013 American Medical Association. All rights reserved.)
CWF Common Working File
DHHS Department of Health and Human Services
DOJ Department of Justice
DRA Deficit Reduction Act of 2005 (Pub. L. 109-171)
DSH Disproportionate Share Hospital
DUA Data Use Agreement Start Printed Page 72762
EHR Electronic Health Record
ESRD End Stage Renal Disease
ETA hospital Electing Teaching Amendment Hospital
FFS Fee-for-service
FQHCs Federally Qualified Health Centers
FTC Federal Trade Commission
GPCI Geographic Practice Cost Index
GPRO Group Practice Reporting Option
HCC Hierarchal Condition Category
HCPCS Healthcare Common Procedure Coding System
HICN Health Insurance Claim Number
HIPAA Health Insurance Portability and Accountability Act of 1996 (Pub. L. 104-191)
HVBP Hospital Value-based Purchasing
IPA Independent Practice Association
IPPS Inpatient Prospective Payment System
IRS Internal Revenue Service
MA Medicare Advantage
MedPAC Medicare Payment Advisory Commission
MLR Minimum Loss Rate
MSP Medicare Secondary Payer
MSR Minimum Savings Rate
MU Meaningful Use
NCQA National Committee for Quality Assurance
NP Nurse Practitioner
NPI National Provider Identifier
NQF National Quality Forum
OIG Office of Inspector General
PA Physician Assistant
PACE Program of All Inclusive Care for the Elderly
PECOS Provider Enrollment, Chain, and Ownership System
PFS Physician Fee Schedule
PGP Physician Group Practice
PHI Protected Health Information
PPS Prospective Payment System
PQRS Physician Quality Reporting System
PRA Paperwork Reduction Act
PSA Primary Service Areas
RHCs Rural Health Clinics
RIA Regulatory Impact Analysis
SNFs Skilled Nursing Facilities
SSA Social Security Act
SSN Social Security Number
TIN Taxpayer Identification Number
VM Value Modifier
CPT (Current Procedural Terminology) Copyright Notice
Throughout this proposed rule, we use CPT codes and descriptions to refer to a variety of services. We note that CPT codes and descriptions are copyright 2013 American Medical Association. All Rights Reserved. CPT is a registered trademark of the American Medical Association (AMA). Applicable Federal Acquisition Regulations (FARs) and Defense Federal Acquisition Regulations (DFARs) apply.
I. Executive Summary and Background
A. Executive Summary
1. Purpose
Section 1899 of the Social Security Act (the Act) established the Medicare Shared Savings Program, which promotes accountability for a patient population, fosters coordination of items and services under parts A and B, and encourages investment in infrastructure and redesigned care processes for high quality and efficient health care service delivery. This proposed rule would make changes to the regulations that were promulgated in November 2011 to implement the Shared Savings Program in order to make refinements based on our experience with the program and to respond to concerns raised by stakeholders. Unless otherwise noted, these changes would be effective 60 days after publication of the final rule. Application or implementation dates may vary, depending on the nature of the policy; however, we anticipate all of the final policies and methodological changes would be applied for the 2016 performance year for all participating organizations unless otherwise noted.
2. Summary of the Major Provisions
This proposed rule is designed to codify existing guidance, reduce administrative burden and improve program function and transparency in the following areas: (1) Data-sharing requirements; (2) requirements for ACO participant agreements, the ACO application process, and our review of applications; (3) identification and reporting of ACO participants and ACO providers/suppliers, including managing changes to the list of ACO participants and ACO providers/suppliers; (4) eligibility requirements related to the ACO's number of beneficiaries, required processes, the ACO's legal structure and governing body, and its leadership and management structure; (5) modification to assignment methodology; (6) repayment mechanisms for ACOs in two-sided performance-based risk tracks; (7) alternatives to encourage participation in risk-based models; (8) ACO public reporting and transparency; (9) the ACO termination process; and (10) the reconsideration review process. To achieve these goals, we make the following proposed modifications to our current program rules:
- Clarify existing and establish new definitions of terms including an ACO participant, ACO provider/supplier, and ACO participation agreement.
- Add a process for ACOs to renew the participation agreement for an additional agreement period.
- Add, clarify, and revise the beneficiary assignment algorithm, including the following—
++ Update the CPT codes that would be considered to be primary care services as well as changing the treatment of certain physician specialties in the assignment process;
++ Include the claims for primary care services furnished by NP, PAs, and CNSs in Step 1 of the assignment algorithm; and
++ Clarify how primary care services furnished in federally qualified health centers (FQHCs), rural health clinics (RHCs), and electing teaching amendment (ETA) hospitals will be considered in the assignment process.
- Expand the kinds of beneficiary-identifiable data that would be provided to ACOs in various reports under the Shared Savings Program as well as simplify the claims data sharing opt-out process to improve the timeliness of access to claims data.
- Add or change policies to encourage greater ACO participation in risk-based models by—
++ Offering the opportunity for ACOs to continue participating under a one-sided participation agreement after their first 3-year agreement;
++ Reducing risk under Track 2; and
++ Adopting an alternative risk-based model referred to as Track 3 which includes proposals for a higher sharing rate and prospective assignment of beneficiaries.
In addition, we seek comment on a number of options that we have been considering in order to encourage ACOs to take on two-sided performance-based risk under the Shared Savings Program. We also seek comment on issues related to resetting the benchmark in a subsequent performance year and the use of statutory waiver authority to improve participation in two-sided risk models.
3. Summary of Costs and Benefits
We assume that our proposals to ease the transition to risk, reduce risk under Track 2, and adopt an alternative risk-based model (Track 3) would result in increased participation in the Shared Savings Program. As shown in our impact analysis, we expect the proposed changes to result in a significant increase in total shared savings, while shared losses would decrease. Moreover, as participation in the Shared Savings Program continues to expand, we anticipate there would be a broader focus on care coordination and quality improvement among providers and suppliers within the Medicare program that would lead to both increased efficiency in the provision of care and improved quality of the care provided to beneficiaries.
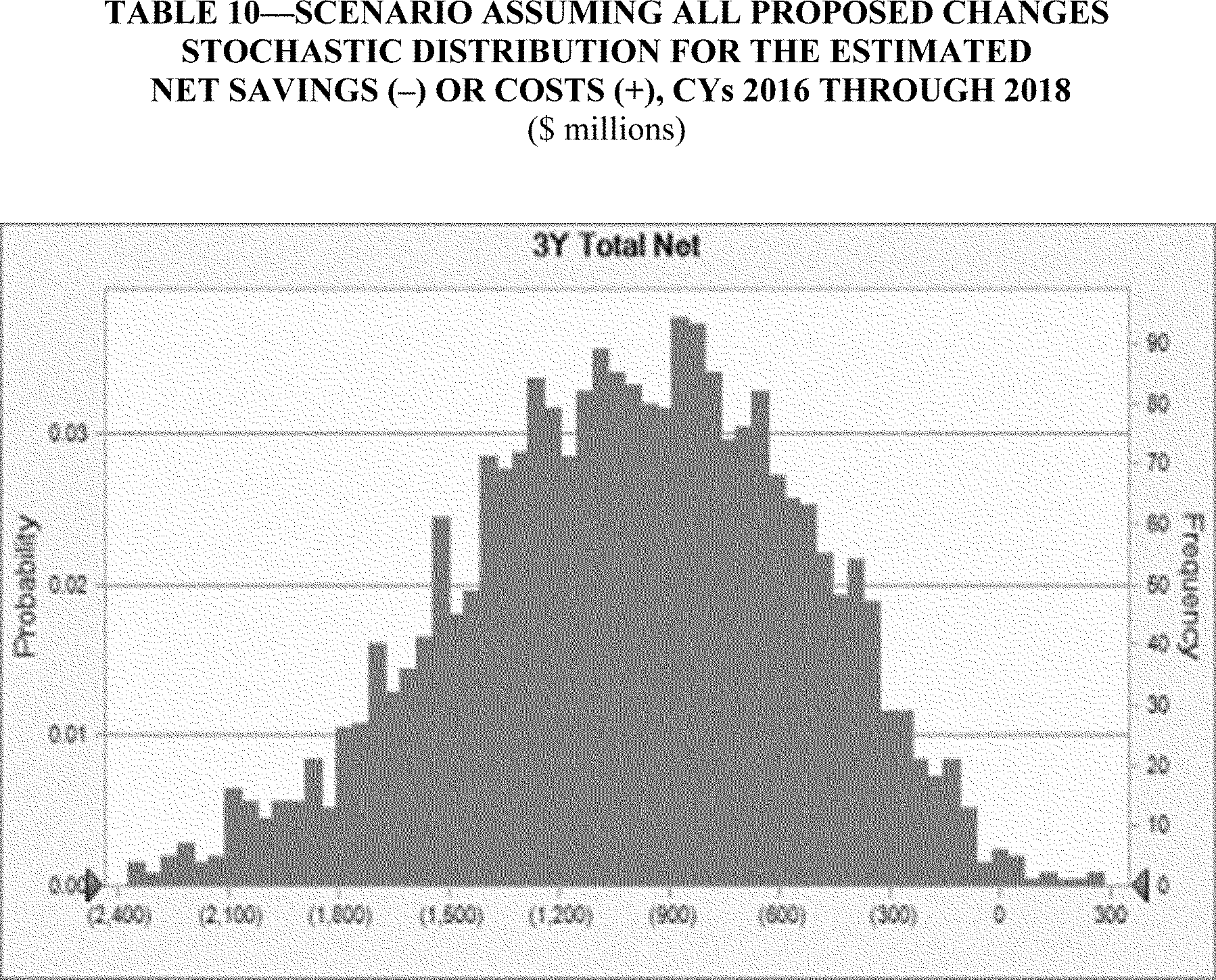
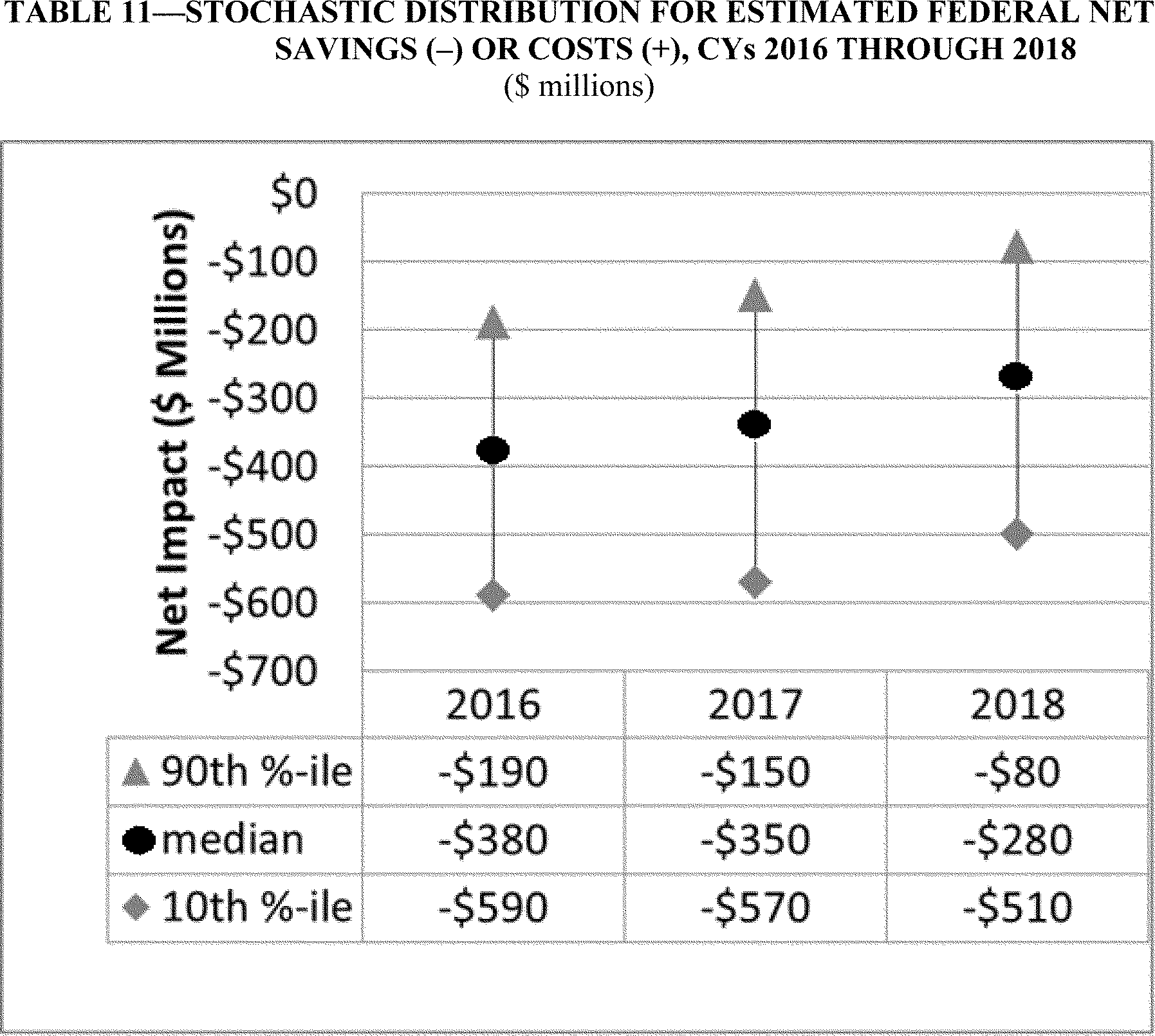
The proposed changes detailed in this rule would result in median estimated federal savings of $280 million greater than the $730 million median net Start Printed Page 72763savings estimated at baseline for calendar years (CYs) 2016 through 2018. We estimate that the provisions of this proposed rule would result in a reduction in the median shared loss dollars by $140 million and an increase in the median shared savings payments by $320 million dollars relative to the baseline for CYs 2016 through 2018. The estimated aggregate average start up investment and 3 year operating costs if all proposals are finalized is approximately $441 million.
B. Background
On March 23, 2010, the Patient Protection and Affordable Care Act (Pub. L. 111-148) was enacted, followed by enactment of the Health Care and Education Reconciliation Act of 2010 (Pub. L. 111-152) on March 30, 2010, which amended certain provisions of Public Law 111-148. Collectively known as the Affordable Care Act, these public laws include a number of provisions designed to improve the quality of Medicare services, support innovation and the establishment of new payment models, better align Medicare payments with provider costs, strengthen Medicare program integrity, and put Medicare on a firmer financial footing.
Section 3022 of the Affordable Care Act amended Title XVIII of the Act (42 U.S.C. 1395 et seq.) by adding new section 1899 to the Act to establish a Shared Savings Program. This program is a key component of the Medicare delivery system reform initiatives included in the Affordable Care Act and is a new approach to the delivery of health care. The purpose of the Shared Savings Program is to promote accountability for a population of Medicare beneficiaries, improve the coordination of FFS items and services, encourage investment in infrastructure and redesigned care processes for high quality and efficient service delivery, and promote higher value care. ACOs that successfully meet quality and savings requirements share a percentage of the achieved savings with Medicare. Under the Shared Savings Program, ACOs share in savings only if they meet both the quality performance standards and generate shareable savings. Consistent with the purpose of the Shared Savings Program, we focused on developing policies aimed at achieving the three-part aim consisting of: (1) Better care for individuals; (2) better health for populations; and (3) lower growth in expenditures.
In the November 2, 2011 Federal Register (76 FR 67802), we published the final rule entitled “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations” (November 2011 final rule). We viewed this final rule as a starting point for the program, and because of the scope and scale of the program and our limited experience with shared savings initiatives under FFS Medicare, we built a great deal of flexibility into the program rules. We anticipated that subsequent rulemaking for the Shared Savings Program would be informed by lessons learned from our experience with the program as well as from testing through the Pioneer ACO Model and other initiatives conducted by the Center for Medicare and Medicaid Innovation (Innovation Center) under section 1115A of the Act.
Over 330 organizations are now participating in the Shared Savings Program. We are gratified by stakeholder interest in this program. In the November 2011 final rule (76 FR 67805), we stated that we intended to assess the policies for the Shared Savings Program and models being tested by the Innovation Center to determine how well they were working and if there were any modifications that would enhance them. As evidenced by the high degree of interest in participation in the Shared Savings Program, we believe that the policies adopted in the November 2011 final rule are generally well-accepted. However, we have identified several policy areas we would like to revisit in light of the additional experience we have gained during the first 2 years of program implementation.
We note that in developing the Shared Savings Program, and in response to stakeholder suggestions, we worked very closely with agencies across the federal government to develop policies to encourage participation in the program and to ensure a coordinated inter- and intra-agency program implementation. The result of this effort was the release of several documents regarding the application of other relevant laws and regulations to ACOs. These documents are described in more detail in section II.C.5. of the November 2011 final rule (76 FR 67840) and include: (1) A joint CMS and DHHS OIG interim final rule with comment period establishing waivers of the application of the physician self-referral law, the Federal anti-kickback statute, and certain civil monetary penalties (CMP) law provisions for specified arrangements involving ACOs participating in the Shared Savings Program (76 FR 67992); (2) an Internal Revenue Service (IRS) notice (Notice 2011-20) and fact sheet (FS-2011-11) issued in response to comments regarding the need for additional tax guidance for tax-exempt organizations, including tax-exempt hospitals, that may participate in the Shared Savings Program (see Notice 2011-20 at www.irs.gov//pub/irs-drop/n-11-20.pdf and FS-2011-11 at www.irs.gov/pub/irs-news/fs-2011-11.pdf); and (3) a final Statement of Antitrust Enforcement Policy Regarding Accountable Care Organizations Participating in the Shared Savings Program issued jointly by the FTC and DOJ (collectively, the Antitrust Agencies) and published in the October 28, 2011 Federal Register (76 FR 67026). We have continued working with these agencies as we have implemented this program and believe that these materials continue to offer valuable information regarding a number of issues of great importance both to our implementation of the Shared Savings Program and to the entities that participate in the program. We encourage ACOs and other stakeholders to review and comply with the referenced documents. Documents can be accessed through the links on our Web site at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Statutes_Regulations_Guidance.html.
II. Provisions of This Proposed Rule
The purpose of this proposed rule is to propose revisions to some key policies adopted in the November 2011 final rule (76 FR 67802), to incorporate in our regulations certain guidance that we have issued since the Shared Savings Program was established, and to propose regulatory additions to support program compliance and growth. Our intent is to encourage continued and enhanced stakeholder participation, to reduce administrative burden for ACOs while facilitating their efforts to improve care outcomes, and to maintain excellence in program operations while bolstering program integrity.
A. Definitions
In the November 2011 final rule (76 FR 67802), we adopted definitions of key terms for purposes of the Shared Savings Program at § 425.20. These terms are used throughout this proposed rule. We encourage readers to review these definitions. Based on our experiences thus far with the Shared Savings Program and inquiries we received regarding the defined terms, we propose some additions to the definitions and a few revisions to the existing definitions.
1. Proposed Definitions
We propose to add several new terms to the definitions in § 425.20. First, we propose to add a definition of “participation agreement.” Specifically, Start Printed Page 72764we propose to define the term to mean the written agreement required under § 425.208(a) between the ACO and CMS that, along with the regulations at part 425, governs the ACO's participation in the Shared Savings Program. We further propose to make conforming changes throughout part 425, replacing references to an ACO's agreement with CMS with the defined term “participation agreement.” In addition, we propose to make a conforming change in § 425.204(c)(1)(i) to remove the incorrect reference to “participation agreements” and replace it with “ACO participant agreements.”
Second, we propose to add the related definition of “ACO participant agreement.” Specifically, we propose to define “ACO participant agreement” to mean the written agreement between an ACO and an ACO participant required at § 425.116 in which the ACO participant agrees to participate in, and comply with, the requirements of the Shared Savings Program.
Third, as discussed in greater detail in section II.F. of this proposed rule, we propose to add a definition for “assignment window,” to mean the 12-month period used to assign beneficiaries to an ACO.
2. Proposed Revisions to Existing Definitions
a. Definition of ACO Participant
The current definition of “ACO participant” states that an “ACO participant means an individual or group of ACO provider(s)/supplier(s), that is identified by a Medicare-enrolled TIN, that alone or together with one or more other ACO participants comprise(s) an ACO, and that is included on the list of ACO participants that is required under § 425.204(c)(5).” Based on inquiries we have received since the publication of November 2011 final rule, we believe that there has been some confusion as to the distinction between an ACO participant and an ACO provider/supplier. The key point is that an ACO participant is an entity, not a practitioner, identified by a Medicare-enrolled TIN (that is, a TIN that is used to bill Medicare for services furnished to Medicare fee-for-service beneficiaries). An ACO participant may be composed of one or more ACO providers/suppliers whose services are billed under a Medicare billing number assigned to the TIN of the ACO participant. Additionally, we emphasize that the ACO is responsible for ensuring that all individuals and entities that have reassigned the right to receive Medicare payment to the TIN of the ACO participant have also agreed to be ACO providers/suppliers.
We propose to revise the definition of “ACO participant” to clarify that an ACO participant is an entity identified by a Medicare-enrolled TIN. Additionally, we are correcting a grammatical error by revising the definition to indicate that one or more ACO participants “compose,” rather than “comprise” an ACO. We note that a related grammatical error is corrected at § 425.204(c)(iv). These proposed changes to the definition of “ACO participant” are not intended to alter the way the Shared Savings Program currently operates.
b. Definition of ACO Professional
Under the current definition at § 425.20, an “ACO professional” means an ACO provider/supplier who is either of the following:
- A physician legally authorized to practice medicine and surgery by the State in which he performs such function or action.
- A practitioner who is one of the following:
++ A physician assistant (as defined at § 410.74(a)(2)).
++ A nurse practitioner (as defined at § 410.75(b)).
++ A clinical nurse specialist (as defined at § 410.76(b)).
We propose to revise the definition of ACO professional to remove the requirement that an ACO professional be an ACO provider/supplier. We also propose to revise the definition of ACO professional to indicate that an ACO professional is an individual who bills for items or services he or she furnishes to Medicare fee-for-service beneficiaries under a Medicare billing number assigned to the TIN of an ACO participant in accordance with Medicare regulations. We are proposing these modifications because there may be ACO professionals who furnished services billed through an ACO participant's TIN in the benchmarking years but are no longer affiliated with the ACO participant and therefore are not furnishing services billed through the TIN of the ACO participant during the performance years. These proposed changes to the definition of “ACO professional” are not intended to alter the way the Shared Savings Program currently operates.
c. Definition of ACO Provider/Supplier
Under the current definition at § 425.20, an “ACO provider/supplier” means an individual or entity that—(1) is a provider (as defined at § 400.202) or a supplier (as defined at § 400.202); (2) is enrolled in Medicare; (3) bills for items and services it furnishes to Medicare fee-for-service beneficiaries under a Medicare billing number assigned to the TIN of an ACO participant in accordance with applicable Medicare regulations; and (4) is included on the certified list of ACO providers/suppliers that is submitted by the ACO. We propose to modify the definition to clarify that an individual or entity is an ACO provider/supplier only when it bills for items and services furnished to Medicare FFS beneficiaries during the agreement period under a Medicare billing number assigned to the TIN of an ACO participant and is included on the list of ACO providers/suppliers that is required under the proposed regulation at § 425.118. We do not believe that an individual or entity that may previously have reassigned the right to receive Medicare payment to an ACO participant, but that is not participating in the activities of the ACO by furnishing care to Medicare FFS beneficiaries that is billed through the TIN of an ACO participant during the ACO's agreement period, should be considered to be an ACO provider/supplier. Thus, this modification is intended to clarify that a provider or supplier must bill for items or services furnished to Medicare FFS beneficiaries through the TIN of an ACO participant during the ACO's agreement period in order to be an ACO provider/supplier.
d. Definition of Assignment
Under the current definition at § 425.20, “assignment” means “the operational process by which CMS determines whether a beneficiary has chosen to receive a sufficient level of the requisite primary care services from a physician who is an ACO provider/supplier so that the ACO may be appropriately designated as exercising basic responsibility for that beneficiary's care.” As discussed previously in this section, we are proposing to modify the definition of “ACO professional” to remove the requirement that an ACO professional be an ACO provider/supplier. Similarly, we believe that for purposes of defining assignment, it is more appropriate to use the term “ACO professional,” as revised, than the term “ACO provider/supplier” because a physician or other practitioner can only be an ACO provider/supplier if he or she bills for items and services through the TIN of an ACO participant during the ACO's agreement period and is included on the list of ACO providers/suppliers required under our regulations. However, as we discussed previously, there may be an ACO professional who furnished services billed through an ACO participant's TIN Start Printed Page 72765in the benchmarking years but is no longer billing through the ACO participant's TIN during the performance years and therefore cannot be considered an ACO provider/supplier. For example, a practitioner that retired before the ACO entered into a participation agreement with CMS and is no longer billing through the TIN of an ACO participant, and therefore was not included on the ACO provider/supplier list is not an ACO provider/supplier. Nevertheless, the services furnished by this ACO professional and billed through the TIN of an ACO participant would be considered for purposes of determining beneficiary assignment to the ACO during the benchmarking period.
In the interests of clarity, we therefore propose to modify the definition of assignment to reflect that our assignment methodology takes into account claims for primary care services furnished by ACO professionals, not solely claims for primary care services furnished by physicians in the ACO. This revision will ensure consistency with program operations and alignment with the definition of “ACO professional” since it is the aggregation of the ACO professionals' claims that impacts assignment. Consistent with section 1899(c) of the Act, a beneficiary must have at least one primary care service furnished by a physician in the ACO in order to be eligible for assignment to the ACO, and this is reflected in the assignment methodology articulated under subpart E of the Shared Savings Program regulations. Once a beneficiary is determined to be eligible for assignment, the beneficiary is then assigned to the ACO if its ACO professionals have rendered the plurality of primary care services for the beneficiary as determined under the stepwise assignment methodology in § 425.402. Thus, we believe the proposed modification to the definition of “assignment” would more accurately reflect the use of claims for primary care services furnished by ACO professionals that are submitted through an ACO participant's TIN in determining beneficiary assignment in the ACO's benchmark and performance years.
Additionally, we propose to make conforming changes as necessary to the regulations governing the assignment methodology in subpart E of part 425, to revise the references to “ACO provider/supplier” to read “ACO professional.”
e. Definition of Hospital
We are proposing a technical revision to the definition of “hospital” for purposes of the Shared Savings Program. Section 1899(h)(2) of the Act provides that, for purposes of the Shared Savings Program, the term “hospital” means a subsection (d) hospital as defined in section 1886(d)(1)(B) of the Act. In the November 2011 final rule (76 FR 67812), we stated that this statutory definition of hospital thus limits: ”. . . the definition to include only acute care hospitals paid under the hospital inpatient prospective payment system (IPPS).” Consistent with this interpretation, we proposed and finalized the following definition of “hospital” for purposes of the Shared Savings Program at § 425.20: “Hospital means a hospital subject to the prospective payment system specified in § 412.1(a)(1) of this chapter.”
Under this regulatory definition, Maryland acute care hospitals would not be considered to be hospitals for purposes of the Shared Savings Program because hospitals in the state of Maryland are subject to a waiver from the Medicare payment methodologies under which they would otherwise be paid. However, we have taken the position in other contexts, for example, for purposes of electronic health record (EHR) incentive payments (75 FR 44448) and in the FY 2014 IPPS final rule (78 FR 50623), that Maryland acute care hospitals remain subsection (d) hospitals. This is because these hospitals are “located in one of the fifty states or the District of Columbia” (as provided in the definition of subsection (d) hospitals at section 1886(d)(1)(B) of the Act) and are not hospitals that are specifically excluded from that category, such as cancer hospitals and psychiatric hospitals.
Therefore, we propose to revise the definition of “hospital” for purposes of the Shared Savings Program to provide that a “hospital” means a hospital as defined in section 1886(d)(1)(B) of the Act. The proposed regulation text is consistent with both the statutory definition of “hospital” for purposes of the Shared Savings Program in section 1899(h)(2) of the Act and the position we have taken in other contexts in referring to subsection (d) hospitals. The effect of this change is to clarify that a Maryland acute care hospital is a “hospital” for purposes of the Shared Savings Program.
f. Definition of Primary Care Services
We propose to modify the definition of “primary care services.” We refer the reader to section II.E.3. of this proposed rule for a more detailed discussion of the proposed revision to this definition, which is relevant to the assignment of a Medicare beneficiary to an ACO.
g. Definitions of “Continuously Assigned Beneficiary” and “Newly Assigned Beneficiary”
As discussed in greater detail in section II.F.3.b. of this proposed rule, we propose revisions to the definitions of “continuously assigned beneficiary” and “newly assigned beneficiary.” These definitions relate to risk adjustment for the assigned population and require minor modification to accommodate the newly proposed Track 3.
h. Definition of Agreement Period
In connection with our discussion of the applicability of certain changes that are made to program requirements during the agreement period, we propose revisions to the definition of “agreement period.” Readers should refer to section II.C.4. of this proposed rule for a discussion of the proposed changes to the definition.
B. ACO Eligibility Requirements
1. Agreement Requirements
a. Overview
Section 1899(b)(2)(B) of the Act requires participating ACOs to “enter into an agreement with the Secretary to participate in the program for not less than a 3-year period.” If the ACO is approved for participation in the Shared Savings Program, an executive who has the ability to legally bind the ACO must sign and submit a participation agreement to CMS (§ 425.208(a)(1)). Under the participation agreement with CMS, the ACO agrees to comply with the regulations governing the Shared Savings Program (§ 425.208(a)(2)). In addition, the ACO must require its ACO participants, ACO providers/suppliers, and other individuals or entities performing functions or services related to the ACO's activities to agree to comply with the Shared Savings Program regulations and all other applicable laws and regulations (§ 425.208(b) and § 425.210(b)). The ACO must provide a copy of its participation agreement with CMS to all ACO participants, ACO providers/suppliers, and other individuals and entities involved in ACO governance (§ 425.210(a)). As part of its application, we currently require each ACO to submit a sample of the agreement it executes with each of its ACO participants (the “ACO participant agreement”). Also, as part of its application and when requesting the addition of new ACO participants, we require an ACO to submit evidence that it has a signed written agreement with each of its ACO participants. (See guidance on our Web site at http://Start Printed Page 72766www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/Memo_Additional_Guidance_on_ACO_Participants.pdf.) An ACO's application to participate in the Shared Savings Program and any subsequent request to add new ACO participants will not be approved if the ACO does not have an agreement in place with each of its ACO participants in which each ACO participant agrees to participate in the Shared Savings Program and to comply with the requirements of the Shared Savings Program.
In our review of applications to participate in the Shared Savings Program, we received many ACO participant agreements that were not properly executed, were not between the correct parties, lacked the required provisions, contained incorrect information, or failed to comply with § 425.304(c) relating to the prohibition on certain required referrals and cost shifting. When we identified such agreements, ACOs experienced processing delays, and in some cases, we were unable to approve the ACO applicant and/or its ACO participant to participate in the Shared Savings Program. Consequently, we issued guidance for ACO applicants in which we reiterated the required elements for ACO participant agreements and strongly recommended that ACOs employ good contracting practices to ensure that each of their ACO participant agreements met our requirements (see http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/Tips-ACO-Developing-Participant-Agreements.pdf).
The ACO participant agreements are necessary for purposes of program transparency and to ensure an ACO's compliance with program requirements. Moreover, many important program operations (including calculation of shared savings, assignment of beneficiaries, and financial benchmarking), use claims and other information that are submitted to CMS by the ACO participant. Our guidance clarified that ACO participant agreements and any agreements with ACO providers/suppliers must contain the following:
- An explicit requirement that the ACO participant or the ACO provider/supplier will comply with the requirements and conditions of the Shared Savings Program (part 425), including, but not limited to, those specified in the participation agreement with CMS.
- A description of the ACO participants' and ACO providers'/suppliers' rights and obligations in and representation by the ACO.
- A description of how the opportunity to get shared savings or other financial arrangements will encourage ACO participants and ACO providers/suppliers to follow the quality assurance and improvement program and evidence-based clinical guidelines.
- Remedial measures that will apply to ACO participants and ACO providers/suppliers who do not comply with the requirements of their agreements with the ACO.
Our guidance also requires that the ACO participant agreements be made directly between the ACO and the ACO participant. We believe it is important that the parties entering into the agreement have a direct legal relationship to ensure that the requirements of the agreement are fully and directly enforceable by the ACO, including the ability of the ACO to terminate an agreement with an ACO participant that is not complying with the requirements of the Shared Savings Program. Additionally, a direct legal relationship ensures that the ACO participant may, if necessary, terminate the agreement with the ACO according to the terms of the agreement without interrupting other contracts or agreements with third parties. Therefore, the ACO and the ACO participant must be the only parties to an ACO participant agreement; the agreements may not include a third party to the agreement. For example, the agreement may not be between the ACO and another entity, such as an independent practice association (IPA) or management company that in turn has an agreement with one or more ACO participants. Similarly, existing contracts between ACOs and ACO participants that include third parties should not be used.
We recognize that there are existing contractual agreements between entities (for example, contracts that permit organizations like IPAs to negotiate contracts with health care payers on behalf of individual practitioners). However, because it is important to ensure that there is a direct legal relationship between the ACO and the ACO participant evidenced by a written agreement, and because ACO participants continue to bill and receive payments as usual under the Medicare FFS rules (that is, there is no negotiation for payment under the program) we believe that typical IPA contracts are generally inappropriate and unnecessary for purposes of participation in the Shared Savings Program. An ACO and ACO participant may use a contract unrelated to the Shared Savings Program as an ACO participant agreement only when it is between the two parties and is amended to satisfy the requirements for ACO participant agreements under the Shared Savings Program.
It is the ACO's responsibility to make sure that each ACO participant agreement identifies the parties entering into the agreement using their correct legal names, specifies the term of the agreement, and is signed by both parties to the agreement. We validate the legal names of the parties based on information the ACO submitted in its application and the legal name of the entity associated with the ACO participant's TIN in the Provider Enrollment Chain & Ownership System (PECOS). We reject an ACO participant agreement if the party names do not match our records. It may be necessary for the ACO to execute a new or amended ACO participant agreement.
Although the ACO participant must ensure that each of its ACO providers/suppliers (as identified by a National Provider Identifier (NPI)) has agreed to participate in the ACO and will comply with program rules, the ACO has the ultimate responsibility for ensuring that all the ACO providers/suppliers that bill through the TIN of the ACO participant (that is, reassign their right to receive Medicare payment to the ACO participant) have also agreed to participate in the Shared Savings Program and comply with our program regulations. The ACO may ensure this by directly contracting with each ACO provider/supplier (NPI) or by contractually requiring the ACO participant to ensure that all ACO providers/suppliers that bill through its TIN have agreed to participate in, and comply with the requirements of, the Shared Saving Program. If the ACO chooses to contract directly with the ACO providers/suppliers, the agreements must meet the same requirements as the agreements with ACO participants. We emphasize that even if an ACO chooses to contract directly with the ACO providers/suppliers (NPIs), it must still have the required ACO participant agreement. In other words, the ACO must be able to produce valid written agreements for each ACO participant and each ACO provider/supplier. Furthermore, since we use TINs (and not merely some of the NPIs that make up the entity identified by a TIN) as the basis for identifying ACO participants, and we use all claims submitted under an ACO participant's TIN for financial calculations and beneficiary assignment, an ACO may not include an entity as an ACO participant unless all Medicare Start Printed Page 72767enrolled providers and suppliers billing under that entity's TIN have agreed to participate in the ACO as ACO providers/suppliers.
To illustrate the requirement that all ACO providers/suppliers must agree to participate in and comply with the terms of the Shared Savings Program before the ACO can include the ACO participant's TIN on its list of ACO participants, we offer the following scenarios that describe when an ACO participant's TIN may and may not be included on the applicant's ACO participant list:
Correct: A large group practice (Medicare-enrolled TIN) decides to participate in an ACO as an ACO participant. Its owner signs an agreement with the ACO on behalf of the practice to participate in the program and follow program regulations. Also, all practitioners that have reassigned their right to receive Medicare payments to the TIN of the large group practice have also agreed to participate and follow program regulations. Therefore, the ACO may include this group practice TIN on its list of ACO participants.
Incorrect: A large group practice (Medicare-enrolled TIN) decides to participate in an ACO as an ACO participant. Its owner signs an agreement to participate in the program and follow program regulations. However, not all practitioners that have reassigned their right to receive Medicare payment to the group practice TIN have agreed to participate in the ACO and follow Shared Savings Program regulations. Therefore, the ACO may not include this group practice TIN on its list of ACO participants.
Incorrect: Several practitioners in a large group practice (Medicare-enrolled TIN) decide to participate in an ACO. However, the group practice as a whole has not agreed to participate in the program. Therefore, the ACO may not include this group practice TIN on its list of ACO participants.
We propose to codify much of our guidance regarding the content of the ACO participant and ACO provider/supplier agreements.
b. Proposed Revisions
First, we propose to add new § 425.116 to set forth the requirements for agreements between an ACO and an ACO participant or ACO provider/supplier. We believe the new provision would promote a better general understanding of the Shared Savings Program and transparency for ACO participants and ACO providers/suppliers. It is our intent to provide requirements that would facilitate and enhance the relationships between ACOs and ACO participants, and reduce uncertainties and misunderstandings leading to rejection of ACO participant agreements during application review. Specifically, we propose to require that ACO participant agreements satisfy the following criteria:
- The ACO and the ACO participant are the only parties to the agreement.
- The agreement must be signed on behalf of the ACO and the ACO participant by individuals who are authorized to bind the ACO and the ACO participant, respectively.
- The agreement must expressly require the ACO participant to agree, and to ensure that each ACO provider/supplier billing through the TIN of the ACO participant agrees, to participate in the Shared Savings Program and to comply with the requirements of the Shared Savings Program and all other applicable laws and regulations (including, but not limited to, those specified at § 425.208(b)).
- The agreement must set forth the ACO participant's rights and obligations in, and representation by, the ACO, including without limitation, the quality reporting requirements set forth in Subpart F, the beneficiary notification requirements set forth at § 425.312, and how participation in the Shared Savings Program affects the ability of the ACO participant and its ACO providers/suppliers to participate in other Medicare demonstration projects or programs that involve shared savings.
- The agreement must describe how the opportunity to receive shared savings or other financial arrangements will encourage the ACO participant to adhere to the quality assurance and improvement program and evidence-based medicine guidelines established by the ACO.
- The agreement must require the ACO participant to update enrollment information with its Medicare contractor using the PECOS, including the addition and deletion of ACO professionals billing through the TIN of the ACO participant, on a timely basis in accordance with Medicare program requirements. The Agreement must also require ACO participants to notify the ACO within 30 days after any addition or deletion of an ACO provider/supplier.
- The agreement must permit the ACO to take remedial action against the ACO participant, and must require the ACO participant to take remedial action against its ACO providers/suppliers, including imposition of a corrective action plan, denial of shared savings payments (that is, the ability of the ACO participant or ACO provider/supplier to receive a distribution of the ACO's shared savings) and termination of the ACO participant agreement, to address noncompliance with the requirements of the Shared Savings Program and other program integrity issues, including those identified by CMS.
- The term of the agreement must be for at least 1 performance year and must articulate potential consequences for early termination from the ACO.
- The agreement must require completion of a close-out process upon the termination or expiration of the ACO's participation agreement that requires the ACO participant to furnish data necessary to complete the annual assessment of the ACO's quality of care and addresses other relevant matters.
Although we propose that the term of an ACO participant agreement be for at least 1 performance year, we do not intend to prohibit early termination of the agreement. We recognize that there may be legitimate reasons to terminate an ACO participant agreement. However, because care coordination and quality improvement requires commitment from ACO participants, we believe this requirement would improve the likelihood of success in the Shared Savings Program. We are also considering whether and how ACO participant agreements should encourage participation to continue for subsequent performance years. We seek comment on this issue.
In the case of an ACO that chooses to contract directly with its ACO providers/suppliers, we propose virtually identical requirements for its agreements with ACO providers/suppliers. We note that agreements with ACO providers/suppliers would not be required to be for a term of 1 year, because we do not want to impede individual practitioners from activities such as retirement, reassignment of billing rights, or changing employers. In the case of ACO providers/suppliers that do not have a contract directly with the ACO, we are considering requiring each ACO to ensure that its ACO participants contract with or otherwise arrange for the services of its ACO providers/suppliers on the same or similar terms as those required for contracts made directly between the ACO and ACO providers/suppliers.
In addition, we propose to add at § 425.204(c)(6) a requirement that, as part of the application process and upon request thereafter, the ACO must submit documents demonstrating that its ACO participants, ACO providers/suppliers, and other individuals or entities performing functions or services related to ACO activities are required to comply Start Printed Page 72768with the requirements of the Shared Savings Program. In the case of ACO participants, the evidence to be submitted must, consistent with our past guidance, include executed agreements or sample form agreements together with the first and last (signature) page of each form agreement that has been fully executed by the parties to the agreement. However, we reserve the right, to request all pages of an executed ACO participant agreement to confirm that it conforms to the sample form agreement submitted by the ACO. We further propose at § 425.116(c) that executed ACO participant agreements must also be submitted when an ACO seeks approval to add new ACO participants. The agreements may be submitted in the same form and manner as set forth in § 425.204(c)(6). Finally, although we would not routinely request an ACO to submit copies of executed agreements with its ACO providers/suppliers or other individuals or entities performing functions or services related to ACO activities as part of the ACO's application or continued participation in each performance year, we reserve our right to request this information during the application or renewal process and at any other time for audit or monitoring purposes in accordance with § 425.314 and § 425.316.
We believe that the proposed requirements regarding agreements between ACOs and ACO participants, together with our earlier guidance regarding good contracting practices, would enhance transparency between the ACO, ACO participants, and ACO professionals, reduce turnover among ACO participants, prevent misunderstandings related to participation in the Shared Savings Program, and assist prospective ACOs in submitting complete applications and requests for adding ACO participants. We believe that codifying these requirements would assist the ACO, ACO participants, and ACO providers/suppliers in better understanding the program and their rights and responsibilities while participating in the program. We solicit comment on the proposed new requirements and on whether there are additional elements that should be considered for inclusion in the agreements the ACO has with its ACO participants and ACO providers/suppliers.
2. Sufficient Number of Primary Care Providers and Beneficiaries
a. Overview
Section 1899(b)(2)(D) of the Act requires participating ACOs to “include primary care ACO professionals that are sufficient for the number of Medicare fee-for-service beneficiaries assigned to the ACO . . .” and that at a minimum, “the ACO must have at least 5,000 such beneficiaries assigned to it. . . .” Under § 425.110(a)(2) of the regulations, an ACO is deemed to have initially satisfied the requirement to have at least 5,000 assigned beneficiaries if the number of Medicare beneficiaries historically assigned to the ACO participants in each of the 3 years before the start of the agreement period is 5,000 or more.
Under the beneficiary assignment methodology set forth in the regulations at part 425, subpart E, the assignment of beneficiaries to a particular ACO for a calendar year is dependent upon a number of factors, including where the beneficiary elected to receive primary care services and whether the beneficiary received primary care services from ACO professionals participating in one or more Shared Savings Program ACOs. We note that to ensure no duplication in shared savings payments for care provided to the same beneficiaries, assignment of a beneficiary may also be dependent on whether the beneficiary has been assigned to another initiative involving shared savings, such as the Pioneer ACO Model (§ 425.114(c)). While a final assignment determination can be made for the first 2 benchmark years (BY1 and BY2, respectively) for an ACO applying to participate in the Shared Savings Program, it is not possible to determine the final assignment for the third benchmark year (BY3) (that is, the calendar year immediately prior to the start of the agreement period) because application review and determination of whether the ACO has met the required 5,000 assignment must take place during BY3 before all claims are submitted for the calendar year. Further, there is a lag period after the end of a calendar year during which additional claims for the year are billed and processed. Therefore, the final historical benchmark for the 3-year period and the preliminary prospective assignment for PY1 must be determined after the ACO's agreement period has already started. We note that we currently estimate the number of historically assigned beneficiaries for the third benchmark year for Tracks 1 and 2 by using claims with dates of service for the last 3 months of benchmark year 2 (October through December) and the first 9 months of benchmark year 3 (January through September, with up to 3 months claims run out, as available). We use this approach to calculate the number of assigned beneficiaries for BY3 in order to be as consistent as possible with the timeframes (that is, 12 month period) and claims run out used for the BY1 and BY2 calculations.
Section 425.110(b) provides that an ACO that falls below 5,000 assigned beneficiaries at any time during the agreement period will be allowed to continue in the program, but CMS must issue a warning letter and place the ACO on a CAP. The purpose of this provision is to ensure that the ACO is aware that its number of assigned beneficiaries is below 5,000, is notified of the consequences of remaining under 5,000, and that the ACO is taking appropriate steps to correct the deficiency.
Section 425.110(b)(1) provides that, while under the CAP, the ACO will remain eligible to share in savings for the performance year in which it fell below the 5,000, and the MSR will be adjusted according to the number of assigned beneficiaries determined at the time of reconciliation. For example, according to Table 6 in the November 2011 final rule (42 FR 67928), a Track 1 ACO with an assigned population of 5,000 would have an MSR of 3.9. If the ACO's number of assigned beneficiaries falls below 5,000, we would work with the CMS Office of the Actuary to determine the MSR for the number of beneficiaries below 5,000, set at the same 90 percent confidence interval that is used to determine an ACO's MSR when the ACO has a smaller assigned beneficiary population. If the number of beneficiaries assigned to the ACO remains less than 5,000 by the end of the next performance year, the ACO is terminated and is not be permitted to share in savings for that performance year (§ 425.110(b)(2)).
b. Proposed Revisions
First, we propose to revise § 425.110(a)(2) to clarify the data used during the application review process to estimate the number of beneficiaries historically assigned in each of the 3 years of the benchmarking period. Specifically, we propose that the number of assigned beneficiaries would be calculated for each benchmark year using the assignment methodology set forth in Subpart E of part 425, and in the case of BY3, we would use the most recent data available with up to a 3-month claims run out to estimate the number of assigned beneficiaries. This proposed revision would reflect current operational processes under which we assign beneficiaries to ACOs using complete claims data for BY1 and BY2 but must rely on incomplete claims data for BY3. We would likely continue to Start Printed Page 72769estimate the number of historically assigned beneficiaries for the third benchmark year by using claims with dates of service for the last 3 months of BY2 and the first 9 months of BY3, with up to 3 months claims run out. However, that could vary from year to year depending on data availability during the application review process. As discussed previously, we believe that using this approach to calculate the number of assigned beneficiaries for BY3 is consistent with the timeframes and claims run out used for BY1 and BY2 calculations because we would be using a full 12 months of claims, rather than the only available claims for the calendar year, which would be less than 12 months.
The estimates of the number of assigned beneficiaries would be used during the ACO application review process to determine whether the ACO exceeds the 5,000 assigned beneficiary threshold for each year of the historical benchmark period. If based upon these estimates, we determine that an ACO had at least 5,000 assigned beneficiaries in each of the benchmark years, it would be deemed to have initially satisfied the eligibility requirement that the ACO have at least 5,000 assigned beneficiaries. The specific data to be used for computing these initial estimates during the ACO application review process would be designated through program instructions and guidance. Although unlikely, it is possible that when final benchmark year assignment numbers are generated after the ACO has been accepted into the program, the number of assigned beneficiaries could be below 5,000. In this event, the ACO will be allowed to continue in the program, but may be subject to the actions set forth in § 425.110(b).
Second, given our experience with the program and the timing of performance year determinations regarding beneficiary assignment provided during reconciliation, we wish to modify our rules to provide greater flexibility to address situations in which an ACO's assigned beneficiary population falls below 5,000 assigned beneficiaries. Specifically, we have concerns that in some cases it may be very difficult for an ACO to increase its number of assigned beneficiaries by the end of the next performance year, as currently required by § 425.110(b)(2). For example, assume an ACO with a start date of January 2013 were to get its third quarterly report for PY1 in November or December 2013, and the report indicated that the ACO's preliminary prospectively assigned beneficiary population had fallen below 5,000. Under our current regulations, we would send the ACO a warning letter and place the ACO on a CAP. If the ACO were to fail to increase its assigned beneficiary population to at least 5,000 by the end of the next performance year (PY2), it would be terminated. We note that increasing the number of assigned beneficiaries generally involves adding new ACO participants and/or ACO providers/suppliers. However, in the previous example, by the time the ACO had been notified that its assigned beneficiary population had fallen below 5,000 beneficiaries, it would have been too late for the ACO to add new ACO participants for PY2, leaving the ACO with more limited options for timely correction of the deficit. We believe that § 425.110(b) should be modified to provide ACOs with adequate time to successfully complete a CAP. Therefore, we propose to revise § 425.110(b)(2) to state that CMS will specify in its request for a CAP the performance year during which the ACO's assigned population must meet or exceed 5,000 beneficiaries. This modification would permit some flexibility for ACOs whose assigned populations fall below 5,000 late in a performance year to take appropriate actions to address the deficit.
Additionally, we do not believe it is necessary to request a CAP from every ACO whose assigned beneficiary population falls below 5,000. For example, we should have the discretion not to impose a CAP when the ACO has already submitted a request to add ACO participants effective at the beginning of the next performance year and CMS has a reasonable expectation that the addition of these new ACO participants would increase the assigned beneficiary population above the 5,000 minimum beneficiary threshold. Therefore, we propose to revise § 425.110(b) to indicate that we have the discretion whether to impose any remedial measures or to terminate an ACO for failure to satisfy the minimum assigned beneficiary threshold. Specifically, we propose to revise § 425.110(b) to state that the ACO “may” be subject to any of the actions described in § 425.216 (actions prior to termination, including a warning letter or request for CAP) and § 425.218 (termination). However, we note that although we are proposing to retain discretion as to whether to impose remedial measures or terminate an ACO whose assigned beneficiary population falls below 5,000, we recognize that the requirement that an ACO have at least 5,000 assigned beneficiaries is a condition of eligibility to participate in the Shared Savings Program under § 1899(b)(2)(D), and would exercise our discretion accordingly and consistently.
3. Identification and Required Reporting of ACO Participants and ACO Providers/Suppliers
a. Overview
For purposes of the Shared Savings Program, an ACO is an entity that is identified by a TIN and comprised of one or more Medicare-enrolled TINs associated with ACO participants (see § 425.20). The Medicare-enrolled TINs of ACO participants, in turn, are associated with Medicare enrolled individuals and entities that bill through the TIN of the ACO participant. (For example, in the case of a physician, the physician has reassigned to the TIN of the ACO participant his or her right to receive Medicare payments, and their services to Medicare beneficiaries are billed by the ACO participant under a billing number assigned to the TIN of the ACO participant).
As part of the application process and annually thereafter, the ACO must submit a certified list identifying all of its ACO participants and their Medicare-enrolled TINs (the “ACO participant list”) (§ 425.204(c)(5)(i)). Additionally, for each ACO participant, the ACO must submit a list identifying all ACO providers/suppliers (including their NPIs or other provider identifiers) that bill Medicare during the agreement period under a billing number assigned to the TIN of an ACO participant (the “ACO provider/supplier list”) (§ 425.204(c)(5)(i)(A)). Our regulations require the ACO to indicate on the ACO provider/supplier list whether an individual is a primary care physician as defined at § 425.20. All Medicare enrolled individuals and entities that bill through an ACO participant's TIN during the agreement period must be on the certified ACO provider/supplier list and agree to participate in the ACO. ACOs are required to maintain, update, and annually furnish the ACO participant and ACO provider/supplier lists to CMS at the beginning of each performance year and at such other times as may be specified by CMS (§ 425.304(d)).
We use TINs identified on the ACO participant list to identify claims billed to Medicare in order to support the assignment of Medicare fee-for-service beneficiaries to the ACO, the implementation of quality and other reporting requirements, and the determination of shared savings and losses (see section 1899(b)(2)(E) of the Act). We also use the ACO's initial (and annually updated) ACO participant list to: Identify parties subject to the Start Printed Page 72770screenings under § 425.304(b); determine whether the ACO satisfies the requirement to have a minimum of 5,000 assigned beneficiaries; establish the historical benchmark; perform financial calculations associated with quarterly and annual reports; determine preliminary prospective assignment for and during the performance year; determine a sample of beneficiaries for quality reporting; and coordinate participation in the Physician Quality Reporting System (PQRS) under the Shared Savings Program. Both the ACO participant and ACO provider/supplier lists are used to ensure compliance with program requirements. We refer readers to our guidance at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Updating-ACO-Participant-List.html for more information.
In this section, we discuss current policy and procedures regarding the identification and required reporting of ACO participants and ACO providers/suppliers. In addition, we propose revisions to our regulations to improve program transparency by ensuring that all ACO participants and ACO providers/suppliers are accurately identified.
b. Proposed Revisions
In order to administer the Shared Savings Program, we need to identify accurately the ACO participants and ACO providers/suppliers associated with each ACO that participates in the program. An accurate understanding of the ACO participants is critical for assignment of beneficiaries to the ACO as well as assessing the quality of care provided by the ACO to its assigned beneficiaries. An accurate understanding of the ACO providers/suppliers is also critical for ensuring compliance with program rules. We believe that this information is equally critical to the ACO for its own operational and compliance purposes. Thus, both CMS and the ACO need to have a common understanding of the individuals and entities that comprise the ACO participants and ACO providers/suppliers in the ACO. We obtain this common understanding by requiring the ACO to certify the accuracy of its ACO participant and ACO provider/supplier lists prior to the start of each performance year and to update the lists as changes occur during the performance year. Because we rely on these lists for both operational and program integrity purposes, we must have a transparent process that results in the accurate identification of all ACO participants and ACO providers/suppliers that compose each ACO in the Shared Savings Program.
We propose to add a new § 425.118 to reflect with more specificity the requirements for submitting ACO participant and ACO provider/supplier lists and the reporting of changes to those lists. In addition, we propose to revise § 425.204(c)(5) and to remove § 425.214(a) and § 425.304(d) because these provisions are addressed in new § 425.118.
(1) Certified Lists of ACO Participants and ACO Providers/Suppliers
We intend to continue to require ACOs to maintain, update and submit to CMS accurate and complete ACO participant and ACO provider/supplier lists, but are proposing to establish new § 425.118 to set forth the requirements and processes for maintaining, updating, and submitting the required ACO participant and ACO provider/supplier lists. New § 425.118 would consolidate and revise provisions at § 425.204(c)(5), § 425.214(a) and § 425.304(d) regarding the ACO participant and ACO provider/supplier lists. Specifically, we propose at § 425.118(a) that prior to the start of the agreement period and before each performance year thereafter, the ACO must provide CMS with a complete and certified list of its ACO participants and their Medicare-enrolled TINs. We would use this ACO participant list to identify the Medicare-enrolled individuals and entities that are affiliated with the ACO participant's TIN in PECOS, the CMS enrollment system. Because these individuals and entities are currently billing through the Medicare enrolled TIN identified by the ACO as an ACO participant, they must be included on the ACO provider/supplier list. We would provide the ACO with a list of all ACO providers/suppliers (NPIs) that we have identified as billing through each ACO participant's Medicare-enrolled TIN. In accordance with § 425.118(a), the ACO would be required to review the list, make any necessary corrections, and certify the lists of all of its ACO participants and ACO providers/suppliers (including their TINs and NPIs) as true, accurate, and complete. In addition, we propose that an ACO must submit certified ACO participant and ACO provider/supplier lists at any time upon CMS request. We note that all NPIs that reassign their right to receive Medicare payment to an ACO participant must be on the certified list of ACO providers/suppliers and must agree to be ACO providers/suppliers. We propose to clarify this point in regulations text at § 425.118(a)(4).
Finally, in accordance with developing and certifying the ACO participant and provider/supplier lists, we propose at § 425.118(d) to require the ACO to report changes in ACO participant and ACO provider/supplier enrollment status in PECOS within 30 days after such changes have occurred (for example, to report changes in an ACO provider's/supplier's reassignment of the right to receive Medicare payment or revocation of billing rights). This requirement corresponds with our longstanding policy that requires enrolled providers and suppliers to notify their Medicare contractors through PECOS within specified timeframes for certain reportable events. We recognize that PECOS is generally not accessible to ACOs to make these changes directly because most ACOs are not enrolled in Medicare. Therefore, an ACO may satisfy the requirement to update PECOS throughout the performance year by requiring its ACO participants to submit the required information directly in PECOS within 30 days after the change, provided that the ACO participant actually submits the required information within 30 days. We propose to require ACOs to include language in their ACO participant agreements (discussed in section II.B.1. of this proposed rule) to ensure compliance with this requirement. We are not proposing to change the current 30-day timeframe required for such reporting in PECOS. These changes are consistent with the current requirements regarding ACO participant and ACO provider/supplier list updates under § 425.304(d) and we believe that they would enhance transparency and accuracy within the Shared Savings Program. We further propose to remove § 425.304(d) because the requirements, although not modified, would be incorporated into new § 425.118(d).
This revised process should afford the ACO the opportunity to work with its ACO participants to identify its ACO providers/suppliers and to ensure compliance with Shared Savings Program requirements. Currently, we also require the ACO to indicate whether the ACO provider/supplier is a primary care physician as defined in § 425.20. Because this information is derived from the claims submitted under the ACO participant's TINs (FQHCs and RHCs being the exception), we have found this unnecessary to implement the program, so we are proposing to remove this requirement, which currently appears in § 425.204(c)(5)(i)(A).Start Printed Page 72771
(2) Managing Changes to ACO Participants
Except for rare instances, such as the cessation of ACO participant operations or exclusion from the Medicare program, we expect ACO participants to remain in the ACO for the entire 3 year agreement period. This is due to our belief that care coordination and quality improvement require the commitment of ACO participants. Moreover, as noted previously, we utilize the ACO participant list, among other things, for assigning beneficiaries to the ACO, determining the ACO's benchmark and performance year expenditures, and drawing the sample for ACO quality reporting. Nevertheless, we understand that there are legitimate reasons why an ACO may need to update its list of ACO participants during the 3-year agreement period. Thus, under current § 425.214(a), an ACO may add or remove ACO participants (identified by TINs) throughout a performance year, provided that it notifies CMS within 30 days of such addition or removal.
If such changes occur, we may, at our discretion, adjust the ACO's benchmark, risk scores, and preliminary prospective assignment (§ 425.214(a)(3)). We articulated the timing of these changes in our guidance (http://cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Updating-ACO-Participant-List.html), which states that we adjust the ACO's historical benchmark at the start of a performance year if the ACO participant list that the ACO certified at the start of that performance year differs from the one it certified at the start of the prior performance year. We use the updated certified ACO participant list to assign beneficiaries to the ACO in the benchmark period (the 3 years prior to the start of the ACO's agreement period) in order to determine the ACO's adjusted historical benchmark. Our guidance provides that, as a result of changes to the ACO's certified ACO participant list, we may adjust the historical benchmark upward or downward. We use the new annually certified list of ACO participants and the adjusted benchmark for the following program operations: The new performance year's assignment; quality measurement and sampling; reports for the new performance year; and financial reconciliation. We provide ACOs with the adjusted Historical Benchmark Report reflecting these changes.
However, our guidance stated that absent unusual circumstances, changes in ACO participants that occur in the middle of a performance year will not result in midyear changes to assignment, sampling for quality reporting, financial reconciliation, or other matters. As indicated in our guidance, the midyear removal of an entity from the ACO participant list due to program integrity issues is one unusual circumstance that could result in midyear changes to assignment and other matters. Finally, our guidance states that we do not make adjustments upon Medicare payment changes such as wage-index adjustments, or the addition or deletion of ACO participants during the course of the performance year made by the ACO and ACO participants.
We propose to add new provisions at § 425.118(b) to address the procedures for adding and removing ACO participants during the agreement period. These proposals revise the regulations to incorporate some of the important policies that we have implemented through our operational guidance as well as some additional proposals to ease the administrative burden generated by the magnitude of changes made to ACO participant lists to date.
First, we propose under § 425.118(b)(1) that an ACO must submit a request to add a new entity to its ACO participant list in the form and manner specified by CMS and that CMS must approve additions to the ACO participant list before they can become effective. We do not believe ACO participants should be admitted into the program if, for example, the screening conducted under § 425.304(b) reveals that the entity has a history of program integrity issues, or if the ACO participant agreement with the entity does not comply with program requirements, or if the entity is participating in another Medicare shared savings initiative (§ 425.114). If CMS denies the request to add an entity to the ACO participant list, then the entity is not eligible to participate in the ACO for the upcoming performance year.
Second, we propose that, if CMS approves the request, the entity will be added to the ACO participant list at the beginning of the following performance year. That is, entities that are approved for addition to the ACO participant list will not become ACO participants, and their claims would not be considered for purposes of benchmarking, assignment and other operational purposes, until the beginning of the next performance year. For example, if an ACO notifies CMS of the addition of an entity in June of the second performance year (PY2), the entity would not become an ACO participant and its claims would not be included in program operations until January 1 of PY3 if CMS approves the entity's addition.
Third, we propose that an ACO must notify CMS no later than 30 days after the date of termination of the entity's ACO participant agreement. The ACO may notify CMS in advance of such termination. The ACO must submit the notice of removal, which must include the date of termination, in the form and manner specified by CMS. We propose that the removal of the ACO participant from the ACO participant list would be effective on the date of termination of the ACO participation agreement.
We propose at § 425.118(b)(3)(i) that changes made by an ACO to its annually certified ACO participant list would result in adjustments to its historical benchmark, assignment, quality reporting sample, and the obligation of the ACO to report on behalf of eligible professionals for certain CMS quality initiatives. We would annually adjust the ACO's benchmark calculations to include (or exclude) the claims submitted during the benchmark years by the newly added (or removed) ACO participants. In other words, the annually certified ACO participant list is used under Subparts E (assignment of beneficiaries), F (quality performance assessment), and G (calculation of shared savings/losses) for the performance year. For example, if an ACO began program participation in 2013, the PY1 certified list generates an historical benchmark calculated from claims submitted by the TINs on the PY1 certified list during CY 2010, 2011, and 2012. If the ACO adds ACO participants during 2013 and certifies an updated list for PY2 reflecting those additions, we would adjust the historical benchmark to accommodate those changes by recalculating the benchmark using the claims submitted by the PY2 list of certified ACO participants during the ACO's same benchmark years (CYs 2010, 2011, and 2012). In this way, the ACO's benchmark continues to be based on the same 3 years prior to the start of the ACO's agreement, but ensures that the changes in ACO composition and performance year calculations retain a consistent comparison between benchmark and performance during the agreement period.
As noted previously, adjustment to the ACO's historical benchmark as a result of changes to the ACO's certified ACO participant list may move the benchmark upward or downward. We would use the annual certified ACO participant list and the adjusted benchmark for the new performance year's beneficiary assignment, quality measurement and other operations that Start Printed Page 72772are dependent on the ACO participant list as outlined in our guidance. We would provide ACOs with an adjusted Historical Benchmark Report that reflects the new certified ACO participant list. We propose to add this requirement at § 425.118(b)(3).
We propose at § 425.118(b)(3)(ii) to codify the policy we established in guidance that, absent unusual circumstances, the removal of an ACO participant from the ACO participant list during the performance year must not affect certain program calculations for the remainder of the performance year in which the removal becomes effective. Namely, the removal of an entity from the ACO participant list during the performance year would not affect the ACO's beneficiary assignment or, by extension, such program operations as the calculation of the ACO's historical benchmark, financial calculations for quarterly and annual reporting, the sample of beneficiaries for quality reporting, or the obligation of the ACO to report on behalf of eligible professionals for certain quality initiatives. In other words, absent unusual circumstances, CMS uses only the ACO participant list that is certified at the beginning of a performance year to assign beneficiaries to the ACO under Subpart E and to determine the ACO's quality and financial performance for that performance year under Subparts F and G. Examples of unusual circumstances that might justify midyear changes include the midyear removal of an ACO participant due to avoidance of at-risk beneficiaries or another program integrity issue.
For example, if an ACO participant is on the ACO's certified list of ACO participants for the second performance year, and the ACO timely notifies CMS of the termination of the entity's ACO participant agreement effective June 30th of PY2, the ACO participant would be removed from the ACO participant list effective June 30th of PY2. However, the former ACO participant's TIN would still be used for purposes of calculating the quality reporting requirements, financial reports, benchmarking, assignment and reporting of PQRS, meaningful use of EHR, and the value-based modifier. The ACO participant list that was certified at the start of the performance year governs the assessment of the ACO's financial and quality performance for that year, regardless of changes to the list during the performance year. We believe this is necessary to help create some stability in the assessment of the ACO's quality and financial performance for each performance year. If CMS had to modify underlying program operations each time an ACO added or removed a TIN from its list of ACO participants, the ACO would not be able to rely on information (such as the calculation of the historical benchmark) that we provide before the beginning of the performance year. We would not make adjustments upon Medicare payment changes such as wage index adjustments.
We further believe it is important for ACOs to communicate effectively with ACO participants that seek to join an ACO so that they understand the potential impact to the ACO, the ACO participant, and the ACO providers/suppliers affiliated with the ACO participant when an ACO participant leaves during a performance year. For example, it is likely that the ACO would be required to report quality data for beneficiaries that were seen by the former ACO participant in the previous 12 months. The ACO must work with the former ACO participant to obtain the necessary quality reporting data. Additionally, the ACO participant would not be able to qualify for PQRS incentive payment or avoid the PQRS payment adjustment apart from the ACO for that performance year. Therefore, it is in the best interest of both parties to understand this in advance and to commit to working together to fulfill the obligations for the performance year. To assist ACO and ACO participants, we have proposed criteria for ACO participant agreements addressing this issue (see section II.B.1. of this proposed rule).
(3) Managing Changes to ACO Providers/Suppliers
We recognize that ACO providers/suppliers may terminate their affiliation with an ACO participant or affiliate with new or additional Medicare-enrolled TINs (which may or may not be ACO participants) on a frequent basis. Thus, the annual certified ACO provider/supplier list may quickly become outdated. In order to ensure that CMS and the ACO have a common understanding of which NPIs are part of the ACO at any particular point in time, our regulations at § 425.214 set forth requirements for managing changes to the ACO during the term of the participation agreement. Specifically, § 425.214(a)(2) and § 425.304(d)(2) require an ACO to notify CMS within 30 days of the addition or removal of an ACO provider/supplier from the ACO provider/supplier list.
We are proposing new § 425.118(c) on how to report changes to the ACO provider/supplier list that occur during the performance year. Under proposed § 425.118(c), ACOs will continue to be required to report these changes within 30 days. As discussed later in this section, we would require the ACO to ensure that changes in ACO participant and ACO provider/supplier enrollment status are reported in PECOS. However, because the lists of ACO providers/suppliers cannot be maintained in PECOS, we propose to require ACOs to notify CMS' Shared Savings Program separately, in the form and manner specified by CMS, of the addition or removal of an ACO provider/supplier. At this time, we anticipate that ACOs will be required to send such notifications via electronic mail; however, specific guidance regarding this notification process would be provided by the Secretary on the CMS Web site and/or through the ACO intranet portal.
We propose that an ACO may add an individual or entity to the ACO provider/supplier list if it notifies CMS within 30 days after the individual or entity became a Medicare-enrolled provider or supplier that bills for items and services it furnishes to Medicare fee-for-service beneficiaries under a billing number assigned to the TIN of an ACO participant. If the ACO provides such notice by the 30-day deadline, the addition of an ACO provider/supplier would be effective on the date specified in the notice furnished to CMS but no earlier than 30 days before the date of notice. If the ACO fails to provide timely notice to CMS regarding the addition of an individual or entity to the ACO provider/supplier list, then the addition becomes effective on the date CMS receives notice from the ACO. However, we note that when an individual has begun billing through the TIN of an ACO participant but is not on the ACO provider/supplier list, the individual satisfies the definition of an ACO professional, in which case his or her claims for services furnished to Medicare fee-for-service beneficiaries are considered for assignment and other operational purposes previously described.
Each potential ACO provider/supplier that reassigns his or her billing rights under the TIN of an ACO participant is screened by CMS through the enrollment process and PECOS system. Additionally, the Shared Savings Program conducts additional screening on a biannual basis for each ACO provider/supplier through the CMS Fraud Prevention System. In spite of this, we are concerned that our proposed effective date for the addition of an individual or entity to the ACO provider/supplier list will prevent us from conducting a robust program integrity screening of such individuals Start Printed Page 72773and entities. Therefore, we are considering whether to delay the effective date of any additions to the ACO provider/supplier list until after we have completed a program integrity screening of the individuals or entities that the ACO wishes to add to the list. For example, we are considering whether to delay the effective date of additions to the ACO provider/supplier list until the start of the next performance year, similar to the timing for adding TINs of ACO participants to the list of ACO participants. In this way, a complete yearly screening, including screening with the assistance of our law enforcement partners, could occur at one time for both the ACO participant list and the ACO provider/supplier list. As noted previously, until the individual or entity has been officially designated as an ACO provider/supplier, that individual or entity would be an ACO professional because of its billing relationship with the ACO participant. Thus, any claims billed by the ACO professional through the TIN of the ACO participant would be used for assignment and related activities during the performance year in which the change takes place, regardless of whether the individual or entity subsequently becomes an ACO provider/supplier. We seek comment on this proposal.
We propose that to remove an ACO provider/supplier from the ACO provider/supplier list, an ACO must notify CMS no later than 30 days after the individual or entity ceases to be a Medicare-enrolled provider or supplier that bills for items and services it furnishes to Medicare fee-for-service beneficiaries under a billing number assigned to the TIN of an ACO participant. The individual or entity would be removed from the ACO provider/supplier list effective as of the date the individual or entity terminates its affiliation with the ACO participant.
(4) Update of Medicare Enrollment Information
We propose at § 425.118(d) to require the ACO to ensure that changes in ACO participant and ACO provider/supplier enrollment status are reported in PECOS consistent with § 424.516 (for example, changes in an ACO provider's/supplier's reassignment of the right to receive Medicare payment or revocation of billing rights). As previously discussed in detail, this requirement corresponds with our longstanding policy that requires enrolled providers and suppliers to notify their Medicare contractors through PECOS within specified timeframes for certain reportable events.
4. Significant Changes to an ACO
a. Overview
Section 425.214(b) requires an ACO to notify CMS within 30 days of any significant change. A significant change occurs when an ACO is no longer able to meet the Shared Savings Program eligibility or program requirements (§ 425.214(b)). Upon receiving an ACO's notice of a significant change, CMS reviews the ACO's eligibility to continue participating in the Shared Savings Program and, if necessary, may terminate the ACO's participation agreement (§ 425.214 (c)). In addition, § 425.214(c)(2) provides that CMS may determine that a significant change has caused the ACO's structure to be so different from what was approved in the ACO's initial application that it is no longer able to meet the eligibility or program requirements. Under such circumstances, CMS would terminate the ACO's participation agreement, and permit the ACO to submit a new application for program participation. In the November 2011 final rule (76 FR 67840), we noted that changes to an ACO participant list could constitute a significant change to an ACO if, for example, the removal of a large primary care practice from the list of ACO participants caused the number of assigned beneficiaries to fall below 5,000.
b. Proposed Revisions
In light of changes proposed in the previous section of this preamble, we propose to redesignate § 425.214(b) and (c) as § 425.214(a) and (b). Second, we propose to describe when certain changes to the ACO constitute a significant change to the ACO. We believe that a change in ownership of an ACO or the addition or deletion of ACO participants could affect an ACO's compliance with the governance requirements in § 425.106 or other eligibility requirements. We note that some changes to the ACO participant list may be of such a magnitude that the ACO is no longer the entity that was originally approved for program participation. In addition, depending on the nature of the change in ownership, the ACO would need to execute a new participation agreement with CMS if the existing participation agreement is no longer with the correct legal entity. We believe that such changes constitute significant changes and should be subject to the actions outlined under § 425.214(b).
Therefore, we are proposing to specify at § 425.214(a) that a significant change occurs when the ACO is no longer able to meet the eligibility or other requirements of the Shared Savings Program, or when the number or identity of ACO participants included on the ACO participant list, as updated in accordance with § 425.118, changes by 50 percent or more during an agreement period. For example, in the case of an ACO whose initial certified ACO participant list contained ten ACO participants, five of which gradually left the ACO and either were not replaced or were replaced with five different ACO participants, the ACO would have undergone a significant change because the number or identity of its ACO participants changed by 50 percent. Similarly, if an ACO's initial certified ACO participant list contains 20 ACO participants, and the ACO incrementally adds 10 new ACO participants for a total of 30 ACO participants, it would have undergone a significant change with the addition of the 10th new ACO participant.
Upon notice that an ACO has experienced a significant change, we would evaluate the ACO's eligibility to continue participating in the Shared Savings Program and make one of the determinations listed in the provision we propose to redesignate as § 425.214(b). We may request additional information to determine whether and under what terms the ACO may continue in the program. We note that a determination that a significant change has occurred would not necessarily result in the termination of the ACO's participation agreement. We further propose to modify § 425.214 to provide that an ACO's failure to notify CMS of a significant change must not preclude CMS from determining that the ACO has experienced a significant change.
In addition, we are seeking comment on whether we should consider amending our regulations to clarify that the ACO's notice of a significant change must be furnished prior to the occurrence of the significant change. We believe some significant changes could benefit from a longer notice period, particularly in the case of a change of ownership that causes the ACO to be unable to comply with program requirements. Therefore, we seek comment on whether ACOs should be required to provide 45 or 60 days' advance notice of a significant change. We also seek comment on what changes in the ACO participant list should constitute a significant change.Start Printed Page 72774
5. Consideration of Claims Billed by Merged/Acquired Medicare-Enrolled Entities
a. Overview
As discussed in the November 2011 final rule (76 FR 67843), we do not believe that mergers and acquisitions by ACO providers and suppliers are the only way for an entity to become an ACO. The statute and our regulations permit ACO participants that form an ACO to use a variety of collaborative organizational structures, including collaborations other than merger. We reject the proposition that an entity under single control, that is, an entity formed through a merger, would be more likely to meet the goals of improved health at a lower cost. However, we have received questions from industry stakeholders regarding how previous mergers and acquisitions of entities with Medicare enrolled billing TINs will be treated for purposes of the Shared Savings Program. In particular, some applicants have inquired whether the claims billed to Medicare in previous years by an entity that has since been merged with, or acquired by, a different entity could be used to determine whether an applicant meets the requirement to have at least 5,000 beneficiaries assigned to it in each of the benchmark years (§ 425.110) and to establish the ACO's historical benchmark and preliminary prospective assignment. To illustrate, suppose a large group practice that is a prospective ACO participant recently purchased two small primary care practices, and the primary care practitioners from those small practices have reassigned the right to receive Medicare payment to the larger group practice Medicare-enrolled TIN. In this instance, it is likely that the primary care providers will continue to serve the same patient population they served before the practices were purchased, and that their patients may appear on the ACO's list of assigned beneficiaries at the end of the performance year. Therefore, applicants and established ACOs have inquired whether there is a way to take into account the claims billed by the Medicare-enrolled TINs of practices acquired by sale or merger for purposes of meeting the minimum assigned beneficiary threshold and creating a more accurate benchmark and preliminary prospective list of assigned beneficiaries for the upcoming performance year. Similarly, an established ACO may request consideration of the claims billed by the Medicare-enrolled TINs of entities acquired during the course of a performance year for the same purposes.
In response to questions from industry stakeholders, we provided additional guidance on our Web site to all Shared Savings Program applicants about the requirements related to mergers and acquisitions (see http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/Merger-Acquisitions-FAQ.pdf). In this guidance, we indicated that under the following circumstances, we may take the claims billed under TINs of entities acquired through purchase or merger into account for purposes of beneficiary assignment and the ACO's historical benchmark:
- The ACO participant must have subsumed the acquired entity's TIN in its entirety, including all the providers and suppliers that reassigned the right to receive Medicare payment to that acquired entity's TIN.
- All the providers and suppliers that previously reassigned the right to receive Medicare payment to the acquired entity's TIN must reassign that right to the TIN of the acquiring ACO participant.
- The acquired entity's TIN must no longer be used to bill Medicare.
In order to attribute the billings of merged or acquired TINs to the ACO's benchmark, the ACO applicant must—
- Submit the acquired entity's TIN on the ACO participant list, along with an attestation stating that all providers and/suppliers that previously billed under the acquired entity's TIN have reassigned their right to receive Medicare payment to an ACO participant's TIN;
- Indicate the acquired entity's TIN and which ACO participant acquired it; and
- Submit supporting documentation demonstrating that the entity's TIN was acquired by an ACO participant through a sale or merger and submit a letter attesting that the acquired entity's TIN will no longer be used to bill Medicare.
We note that we require an applicant's list of ACO providers/suppliers to include all individuals who previously billed under the acquired entity's TIN to have reassigned their right to receive Medicare payment to an ACO participant's TIN.
We believe that these requirements are necessary to ensure that these entities have actually been completely merged or acquired and that it would be likely that the primary care providers will continue to serve the same patient population. In this way, the beneficiary assignments and the benchmarks would be more accurate for ACOs that include merged or acquired Medicare-enrolled TINs under which their ACO professionals billed during application or updates to the ACO participant list.
b. Proposal
We believe the current criteria and processes have been working well and have benefited both CMS (for example, by providing assurance that an entity's Medicare-enrolled billing TIN have actually been acquired through sale or merger) and the affected ACOs (for example, by allowing for an increase in the ACO's number of appropriately assigned beneficiaries and providing for a more accurate financial benchmark). To avoid uncertainty and to establish a clear and consistent process for the recognition of the claims previously billed by the TINs of acquired entities, we propose to codify the current operational guidance on this topic at § 425.204(g) with some minor revisions to more precisely and accurately describe our proposed policy. Proposed § 425.204(g) would add the option for ACOs to request consideration of claims submitted by the Medicare-enrolled TINs of acquired entities as part of their application, and would address the documentation requirements for such requests. Although this provision is added in a section regarding the content of the initial application, we propose to permit ACOs to annually request consideration of claims submitted by the TINs of entities acquired through sale or merger upon submission of the ACO's updated list of ACO participants.
6. Legal Structure and Governance
Section 1899(b)(1) of the Act requires ACO participants to have established a “mechanism for shared governance” in order to be eligible to participate as ACOs in the Shared Savings Program. In addition, section 1899(b)(2)(C) of the Act requires the ACO to have a formal legal structure that allows the organization to receive and distribute shared savings payments to ACO participants and ACO providers/suppliers. We believe this requirement is important because a formal legal structure can ensure the ACO is protected against improper influence. In this section, we propose clarifications to our rules related to the ACO's legal entity and governing body. The purpose of these changes is to clarify our regulations and to ensure that ACO decision making is governed by individuals who have a fiduciary duty, including a duty of loyalty, to the ACO alone and not to any other individuals or entities. We believe these clarifications are relatively minor and would not significantly impact the program as currently implemented.Start Printed Page 72775
a. Legal Entity and Governing Body
(1) Overview
As specified in the November 2011 final rule (76 FR 67816) and at § 425.104(a), an ACO must be a legal entity, formed under applicable state, federal, or tribal law, and authorized to conduct business in each state in which it operates for purposes of the following:
- Receiving and distributing shared savings.
- Repaying shared losses or other monies determined to be owed to CMS.
- Establishing, reporting, and ensuring provider compliance with health care quality criteria, including quality performance standards.
- Fulfilling other ACO functions identified in this part.
Additionally, under § 425.104(b), an ACO formed by two or more “otherwise independent” ACO participants must be a legal entity separate from any of its ACO participants. Our regulations at § 425.106(b)(4) further specify that when an ACO comprises “multiple, otherwise independent ACO participants,” the governing body of the ACO must be “separate and unique to the ACO”. In contrast, if the ACO is an “existing legal entity,” the ACO governing body may be the same as the governing body of that existing legal entity, provided it satisfies all other requirements of § 425.106, including provisions regarding the fiduciary duties of governing body members, the composition of the governing body, and conflict of interest policies (§ 425.106(b)(5)).
Some applicants have questioned when an ACO needs to be formed as a separate legal entity, particularly the meaning in § 425.104(b) of “otherwise independent” ACO participants. Specifically, applicants have questioned whether multiple prospective ACO participants are “otherwise independent” when they have a prior relationship through, for example, an integrated health system. In addition, we received some questions regarding compliance with the governing body requirements set forth in § 425.106(b)(4) and (5). For example, we received questions from some IPAs, each of which wanted to apply to the Shared Savings Program as an ACO using its existing legal structure and governing body. In some cases, the IPA represented many group practices, but not every group practice represented by an IPA had agreed to be an ACO participant. We believe that such an IPA would need to organize its ACO as a separate legal entity with its own governing body to ensure that the governing body members would have a fiduciary duty to the ACO alone, as required by § 425.106(b)(3), and not to an entity comprised in part by entities that are not ACO participants.
(2) Proposed Revisions
We propose to clarify our regulation text regarding when an ACO must be formed as a separate legal entity. Specifically, we propose to remove the reference to “otherwise independent ACO participants” in § 425.104(b). The revised regulation would provide that an ACO formed by “two or more ACO participants, each of which is identified by a unique TIN,” must be a legal entity separate from any of its ACO participants. For example, if an ACO is composed of three ACO participants, each of which belongs to the same health system or IPA, the ACO must be a legal entity separate and distinct from any one of the three ACO participants.
In addition, we propose to clarify § 425.106(a), which sets forth the general requirement that an ACO have an identifiable governing body with the authority to execute the functions of an ACO. Specifically, we propose that the governing body must satisfy three criteria. First, the governing body of the ACO must be the same as the governing body of the legal entity that is the ACO. Second, in the case of an ACO that comprises multiple ACO participants the governing body must be separate and unique to the ACO and must not be the same as the governing body of any ACO participant. Third, the governing body must satisfy all other requirements set forth in § 425.106, including the fiduciary duty requirement. We note that the second criterion incorporates the requirement that currently appears at § 425.106(b)(4), which provides that the governing body of the ACO must be separate and unique to the ACO in cases where there are multiple ACO participants. Accordingly, we propose to remove § 425.106(b)(4). We further propose to remove § 425.106(b)(5), which provides that if an ACO is an existing legal entity, its governing body may be the same as the governing body of that existing entity, provided that it satisfies the other requirements of § 425.106. In light of our proposed revision to § 425.106(a), we believe this provision is unnecessary and should be removed to avoid confusion.
In proposing that the governing body be the same as the governing body of the legal entity that is the ACO, we intend to preclude delegation of all ACO decision-making authority to a committee of the governing body or retention of ACO decision-making authority by a parent company; ultimate authority for the ACO must still reside with the governing body. We recognize that the governing body of the legal entity that is the ACO may wish to organize committees that address certain matters pertaining to the ACO, but we do not believe that such committees can constitute the governing body of the ACO. We also recognize that a parent organization may wish to retain certain authorities to protect the parent company and ensure the subsidiary's success; however, the ACO's governing body must retain the ultimate authority to execute the functions of an ACO. As stated in the regulations, we believe such functions include such things as developing and implementing the required processes under § 425.112 and holding leadership and management accountable for the ACO's activities. We also believe this authority extends to such activities including the appointment and removal of members of the governing body, leadership, and management, and determining how shared savings are used and distributed among ACO participants and ACO providers/suppliers. We seek comments on this proposal that the ultimate authority for the ACO to carry out its activities must reside with the governing body of the ACO.
The purpose of the new provision precluding the governing body of the ACO from being the same as the governing body of an ACO participant is to ensure that decisions made on behalf of the ACO are not improperly influenced by the interests of individuals and entities other than the ACO. In order to comply with the requirement that the governing body be separate and unique to the ACO, it must not be responsible for representing the interests of any entity participating in the ACO or any entity that is not participating in the ACO. Thus, we propose the requirement that an ACO's governing body must not be the same as the governing body of any of the ACO participants.
b. Fiduciary Duties of Governing Body Members
(1) Overview
Our current regulations at § 425.106(b)(3) require that the governing body members have a fiduciary duty to the ACO and must act consistent with that fiduciary duty. We have clarified in guidance that the governing body members cannot meet the fiduciary duty requirement if the governing body is also responsible for governing the activities of individuals or entities that are not part of the ACO (See “Additional Guidance for Medicare Shared Savings Program Accountable Care Organization (ACO) Applicants” Start Printed Page 72776located online at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/Memo_Additional_Guidance_on_ACO_Participants.pdf). For example, in the case of an IPA that applies as an ACO to the Shared Savings Program, we believe it would be difficult for the members of the IPA's governing body to make decisions in the best interests of the ACO if only some of the group practices that compose the IPA are ACO participants; decisions affecting the ACO may be improperly influenced by the interests of group practices that are part of the IPA but are not ACO participants. For this reason, our regulations require the IPA to establish the ACO as a separate legal entity. This new legal entity must have a governing body whose members have a fiduciary responsibility to the ACO alone and not to any other individual or entity.
We wish to emphasize that the ACO's governing body decisions must be free from the influence of interests that may conflict with the ACO's interests.
(2) Proposed Revisions
We propose to clarify in § 425.106(b)(3) that the fiduciary duty owed to an ACO by its governing body members includes the duty of loyalty. This proposal does not represent a change in policy and is simply intended to emphasize that members of an ACO governing body must not have divided loyalties; they must act only in the best interests of the ACO and not another individual or entity, including the individual interests of ACO participants, ACO professionals, ACO providers/suppliers, or other individuals or entities.
c. Composition of the Governing Body
(1) Overview
Section 1899(b)(1) requires an ACO to have a “mechanism for shared governance” among ACO participants. Section 425.106(c)(1) of the regulations requires an ACO to provide for meaningful participation in the composition and control of the ACO's governing body for ACO participants or their designated representatives. As we explained in the November 2011 final rule (76 FR 67819), we believe that an ACO should be operated and directed by Medicare-enrolled entities that directly provide health care services to beneficiaries. However, we acknowledged, that small groups of providers often lack both the capital and infrastructure necessary to form an ACO and to administer the programmatic requirements of the Shared Savings Program and could benefit from partnerships with non-Medicare enrolled entities. For this reason, we proposed (76 FR 19541) that to be eligible for participation in the Shared Savings Program, the ACO participants must have at least 75 percent control of the ACO's governing body. In the November 2011 final rule, we explained that this requirement would ensure that ACOs remain provider-driven, but also leave room for nonproviders to participate in the program.
In addition, to provide for patient involvement in the ACO governing process, we specified at § 425.106(c)(2) that an ACO's governing body must include a Medicare beneficiary served by the ACO who does not have a conflict of interest with the ACO. We acknowledged that beneficiary representation on an ACO's governing body may not always be feasible. For example, commenters raised concerns that requiring a beneficiary on the governing body could conflict with State corporate practice of medicine laws or other local laws regarding governing body requirements for public health or higher education institutions (76 FR 67821). As a result, we believed it was appropriate to provide some flexibility for us to permit an ACO to adopt an alternative structure for its governing body, while still ensuring that ACO participants and Medicare FFS beneficiaries are involved in ACO governance.
Accordingly, the November 2011 final rule, offers some flexibility to permit an ACO to participate in the Shared Savings Program even if its governing body fails to include a beneficiary or satisfy the requirement that 75 percent of the governing body be controlled by ACO participants. Specifically, § 425.106(c)(5) provides that if an ACO's governing body does not meet either the 75 percent threshold or the requirement regarding beneficiary representation, it must describe in its application how the proposed structure of its governing body would involve ACO participants in innovative ways in ACO governance or provide a meaningful opportunity for beneficiaries to participate in the governance of the ACO. For example, under this provision, we anticipated that exceptions might be needed for ACOs that operate in states with Corporate Practice of Medicine restrictions to structure beneficiary representation accordingly. We contemplated that this provision could also be used by an existing entity to explain why it should not be required to reconfigure its board if it had other means of addressing the requirement to include a consumer perspective in governance (see 76 FR 67821).
(2) Proposed Revisions
We propose to revise § 425.106(c)(5) to remove the flexibility for ACOs to deviate from the requirement that at least 75 percent control of an ACO's governing body must be held by ACO participants. Based on our experience to date with implementing the program, we have learned that ACO applicants do not have difficulty meeting the requirement under § 425.106(c)(3) that ACO participants maintain 75 percent control of the governing body. We have not denied participation to any ACO applicants on the basis of failure to comply with this requirement, and it has not been necessary to grant any exceptions to this rule under § 425.106(c)(5). To the contrary, we have found the 75 percent control requirement to be necessary and protective of the ACO participant's interests. Accordingly, we believe there is no reason to continue to offer an exception to the rule.
We continue to believe it is important to maintain the flexibility for ACOs to request innovative ways to provide meaningful representation of Medicare beneficiaries on ACO governing bodies. Based on our experience, some ACOs have been unable to include a beneficiary on their governing body, and these entities have used the process under § 425.106(c)(5) to establish that they satisfy the requirement for meaningful beneficiary representation through the use of patient advisory bodies that report to the governing body of the ACO.
We also propose to revise § 425.106(c)(2) to explicitly prohibit an ACO provider/supplier from being the beneficiary representative on the governing body. Some ACO applicants have proposed that one of their ACO providers/suppliers would serve as the beneficiary representative on the governing body. We believe it would be very difficult for an ACO provider/supplier who is Medicare beneficiary to represent only the interests of beneficiaries, rather than his or her own interests as an ACO provider/supplier, the interests of other ACO providers/suppliers, or the interests of the ACO participant through which he or she bills Medicare. Finally, we are proposing to revise § 425.106(c)(1) to reiterate the statutory standard in section 1899(b)(1) of the Act requiring an ACO to have a “mechanism for shared governance” among ACO participants. Although we declined in the November 2011 final rule to promulgate a requirement that each Start Printed Page 72777ACO participant be a member of the ACO's governing body (76 FR 67818), the governing body must nevertheless represent a mechanism for shared governance among ACO participants. To that end, the governing body of an ACO that is composed of more than one ACO participant should not, for example, include representatives from only one ACO participant. For ACOs that have extensive ACO participant lists, we would expect to see representatives from many different ACO participants on the governing body. Our proposal to reiterate the statutory standard for shared governance in our regulations at § 425.106(c)(1) does not constitute a substantive change to the program.
7. Leadership and Management Structure
a. Overview
Section 1899(b)(2)(F) of the Act requires an eligible ACO to “have in place a leadership and management structure that includes clinical and administrative systems.” Under this authority, we incorporated certain leadership and management requirements into the Shared Savings Program, as part of the eligibility requirements for program participation. In the November 2011 final rule (76 FR 67822), we stated that we believed an ACO's leadership and management structure should align with and support the goals of the Shared Savings Program and the three-part aim of better care for individuals, better health for populations, and lower growth in expenditures.
In the November 2011 final rule (76 FR 67825), we established the requirement that the ACO's operations be managed by an executive, officer, manager, general partner, or similar party whose appointment and removal are under the control of the ACO's governing body and whose leadership team has demonstrated the ability to influence or direct clinical practice to improve efficiency, processes, and outcomes (see § 425.108(b)). In addition, under § 425.108(c), clinical management and oversight must be managed by a senior-level medical director who is one of the ACO providers/suppliers, who is physically present on a regular basis in an established ACO location (clinic, office or other location participating in the ACO), and who is a board-certified physician licensed in a State in which the ACO operates. In § 425.204(c)(1)(iii), we require ACO applicants to submit materials documenting the ACO's organization and management structure, including senior administrative and clinical leaders specified in § 425.108.
In the November 2011 final rule (76 FR 67825), we provided flexibility for ACOs to request an exception to the leadership and management requirements set forth under § 425.108(b) and (c). We believed that affording this flexibility was appropriate in order to encourage innovation in ACO leadership and management structures. In accordance with § 425.108(e), we reserve the right to give consideration to an innovative ACO leadership and management structure that does not comply with the requirements of § 425.108(b) and (c).
We continue to believe that having these key leaders (operational manager and clinical medical director) is necessary for a well-functioning and clinically integrated ACO. We have learned from our experience with the program, over four application cycles, that ACO applicants generally do not have difficulty in meeting the operational manager and clinical medical director requirements. Only one ACO has requested an exception to the medical director requirements. In that case, the ACO sought the exception in order to allow a physician, who had retired after a long tenure with the organization to serve as the medical director of the ACO. We approved this request because, although the retired physician was not an ACO provider/supplier because he was no longer billing for physician services furnished during the agreement period, he was closely associated with the clinical operations of the ACO, familiar with the ACO's organizational culture, and dedicated to this one ACO.
In addition, we have received a number of questions from ACO applicants regarding the other types of roles for which CMS requires documentation under § 425.204(c)(1)(iii) to evaluate whether an applicant has a “. . . leadership and management structure that includes clinical and administrative systems” that support the purposes of the Shared Savings Program and the aims of better care for individuals, better health for populations, and lower growth in expenditures, as articulated at § 425.108(a)). In response to such inquiries regard, we have indicated that we consider an ACO's “. . . leadership and management structure that includes clinical and administrative systems” to be comprised of the operational manager and clinical medical director (referenced under § 425.108(b) and (c)) as well as the qualified healthcare professional that is required under § 425.112(a) to be responsible for the ACO's quality assurance and improvement program.
b. Proposed Revisions
We propose to amend § 425.108 to provide some additional flexibility regarding the qualifications of the ACO medical director and to eliminate the provision permitting some ACOs to enter the program without satisfying the requirements at § 425.108(b) and (c) for operations and clinical management. In addition, we propose to amend § 425.204(c)(iii) to clarify that applicants must submit materials regarding the qualified health care professional responsible for the ACO's quality assurance and improvement program. We discuss each proposal later in this section.
We believe that it is appropriate to amend the medical director requirement at § 425.108(c) to allow some additional flexibility. Specifically, we propose to remove the requirement that the medical director be an ACO provider/supplier. This change would permit an ACO to have a medical director who was, for example, previously closely associated with an ACO participant but who is not an ACO provider/supplier because he or she does not bill through the TIN of an ACO participant and is not on the list of ACO providers/suppliers. Alternatively, we may retain the requirement that an ACO's medical director be an ACO provider/supplier, but permit ACOs to request CMS approval to designate as its medical director a physician who is not an ACO provider/supplier but who is closely associated with the ACO and satisfies all of the other medical director requirements. We seek comment on whether an ACO medical director who is not an ACO provider/supplier must have been closely associated with the ACO or an ACO participant in the recent past. In addition, we propose to clarify that the medical director must be physically present on a regular basis “at any clinic, office, or other location of the ACO, ACO participant or ACO provider/supplier.” Currently, the provision incorrectly refers only to locations “participating in the ACO.”
However, we continue to strongly believe that the medical director of the ACO should be directly associated with the ACO's clinical operations and familiar with the ACO's organizational culture. This is one purpose of the provision requiring medical directors to be physically present on a regular basis at any clinic, office, or other ACO location. A close working relationship with the ACO and its clinical operations is necessary in order for the medical director to lead the ACO's efforts to achieve quality improvement and cost efficiencies.Start Printed Page 72778
We propose to eliminate § 425.108(e), which permits us to approve applications from innovative ACOs that do not satisfy the leadership and management requirements related to operations management and clinical management and oversight set forth at § 425.108(b) and (c). Based on our experience with the program and the proposed change to the medical director requirement, we believe it is unnecessary to continue to allow ACOs the flexibility to request an exception to the leadership and management requirements related to operations management and clinical management and oversight (§ 425.108(b) and (c)). These requirements are broad and flexible and have not posed a barrier to participation in the Shared Savings Program; in fact, in only one instance has an ACO requested an exception to the operations management criterion (§ 425.108(b)). We are unaware of any alternative operations management structure that might be considered acceptable, and we have modified § 425.108(c) to accommodate the one exception we have granted to date. Accordingly, we propose to revise the regulations by striking § 425.108(e) to eliminate the flexibility for ACOs to request an exception to the leadership and management requirements at § 425.108(b) and (c).
Finally, to clarify questions that have been raised by ACO applicants and to reduce the need for application corrections, we propose to modify § 425.204(c)(1)(iii) to require a Shared Savings Program applicant to submit documentation regarding the qualified healthcare professional responsible for the ACO's quality assurance and improvement program (as required by § 425.112(a)).
We seek comment on these changes to the requirements for ACO leadership and management.
8. Required Process To Coordinate Care
a. Overview
Section 1899(b)(2)(G) of the Act requires an ACO to “define processes to . . . coordinate care, such as through the use of telehealth, remote patient monitoring, and other such enabling technologies.” In the November 2011 final rule (76 FR 67829 through 67830), we established requirements under § 425.112(b)(4) that ACOs define their care coordination processes across and among primary care physicians, specialists, and acute and postacute providers. As part of this requirement, an ACO must define its methods and processes to coordinate care throughout an episode of care and during its transitions. In its application to participate in the Shared Savings Program, the ACO must submit a description of its individualized care program, along with a sample care plan, and explain how this program is used to promote improved outcomes for, at a minimum, its high-risk and multiple chronic condition patients. In addition, an ACO's application must describe target populations that would benefit from individualized care plans.
In developing these policies for the November 2011 final rule (76 FR 67819), we received comments acknowledging that requiring ACOs to define processes to promote coordination of care is vital to the success of the Shared Savings Program. Commenters stressed the importance of health information exchanges in coordination of care activities and recommended that CMS allow ACOs the flexibility to use any standards-based electronic care coordination tools that meet their needs. Other commenters suggested that the proposed rule anticipated a level of functional health information exchange and technology adoption that may be too aggressive.
As stated in § 425.204(c)(1)(ii), applicants to the Shared Savings Program must provide a description, or documents sufficient to describe, how the ACO will implement the required processes and patient-centeredness criteria under § 425.112, including descriptions of the remedial processes and penalties (including the potential for expulsion) that will apply if an ACO participant or an ACO provider/supplier fails to comply with and implement these processes. Under § 425.112(b), an ACO must establish processes to accomplish the following: promote evidence-based medicine; Promote patient engagement; develop an infrastructure to internally report on quality and cost metrics required for monitoring and feedback; and coordinate care across and among primary care physicians, specialists and acute and postacute providers and suppliers.
In addition to the processes described previously, we believe it is important for applicants to explain how they will develop the health information technology tools and infrastructure to accomplish care coordination across and among physicians and providers Adoption of health information technology is important for supporting care coordination by ACO participants and other providers outside the ACO in the following ways: Secure, private sharing of patient information; reporting on quality data and aggregating data across providers and sites to track quality measures; and deploying clinical decision support tools that provide access to alerts and evidence based-guidelines. As ACOs establish more mature processes for risk management, information technology infrastructure allows ACOs and providers to conduct robust financial management of beneficiary populations, deliver cost and quality feedback reporting to individual providers, and streamline the administration of risk based contracts across multiple payers. We believe that requiring ACOs to address health information technology infrastructure in their application to the Shared Savings program would support more careful planning and increased focus on this issue.
b. Accelerating Health Information Technology
HHS believes all patients, their families, and their healthcare providers should have consistent and timely access to their health information in a standardized format that can be securely exchanged between the patient, providers, and others involved in the patient's care. (HHS August 2013 Statement, “Principles and Strategies for Accelerating Health Information Exchange”) HHS is committed to accelerating health information exchange (HIE) through the use of EHRs and other types of health information technology (HIT) across the broader care continuum through a number of initiatives including: (1) Alignment of incentives and payment adjustments to encourage provider adoption and optimization of HIT and HIE services through Medicare and Medicaid payment policies; (2) adoption of common standards and certification requirements for interoperable HIT; (3) support for privacy and security of patient information across all HIE-focused initiatives; and (4) governance of health information networks. These initiatives are designed to encourage HIE among health care providers, including professionals and hospitals eligible for the Medicare and Medicaid EHR Incentive Programs and those who are not eligible for the EHR Incentive programs as well as those providers that are participating in the Medicare Shared Savings Program as an ACO and those that are not, and are designed to improve care delivery and coordination across the entire care continuum. For example, the Transition of Care Measure #2 in Stage 2 of the Medicare and Medicaid EHR Incentive Programs requires HIE to share summary records for at least 10 percent of care transitions.
We believe that HIE and the use of certified EHRs can effectively and Start Printed Page 72779efficiently help ACOs and participating providers improve internal care delivery practices, support management of patient care across the continuum, and support the reporting of electronically specified clinical quality measures (eCQMs).
c. Proposed Revisions
We continue to believe that ACOs should coordinate care between all types of providers and across all services, and that the secure, electronic exchange of health information across all providers in a community is of the utmost importance for both effective care coordination activities and the success of the Shared Savings Program. We understand that ACOs will differ in their ability to adopt the appropriate health information exchange technologies, but we continue to underscore the importance of robust health information exchange tools in effective care coordination.
ACOs have reported how important access to real time data is for providers to improve care coordination across all sites of care, including outpatient, acute, and postacute sites of care. We believe that providers across the continuum of care are essential partners to physicians in the management of patient care. ACOs participating in the program indicate that they are actively developing the necessary infrastructure and have been encouraging the use of technologies that enable real time data sharing among and between sites of care. We believe having a process and plan in place to coordinate a beneficiary's care by electronically sharing health information improves care, and that this helps all clinicians involved in the care of a patient to securely access the necessary health information in a timely manner. It also can also be used to engage beneficiaries in their own care. We further believe that Shared Savings Program applicants should provide, as part of the application, their plans for improving care coordination by developing, encouraging, and using enabling technologies and electronic health records to make health information electronically available to all practitioners involved in a beneficiary's care.
Therefore, we propose to add a new requirement to the eligibility requirements under § 425.112(b)(4)(ii)(C) which would require an ACO to describe in its application how it will encourage and promote the use of enabling technologies for improving care coordination for beneficiaries. Such enabling technologies and services may include electronic health records and other health IT tools (such as population health management and data aggregation and analytic tools), telehealth services (including remote patient monitoring), health information exchange services, or other electronic tools to engage patients in their care. We also propose to add a new provision at § 425.112(b)(4)(ii)(D) to require the applicant to describe how the ACO intends to partner with long-term and postacute care providers to improve care coordination for the ACO's assigned beneficiaries. Finally, we propose to add a provision under § 425.112(b)(4)(ii)(E) to require that an ACO define and submit major milestones or performance targets it will use in each performance year to assess the progress of its ACO participants in implementing the elements required under § 425.112(b)(4). For instance, providers would be required to submit milestones and targets such as: Projected dates for implementation of an electronic quality reporting infrastructure for participants; the number of providers expected to be connected to health information exchange services by year; or the projected dates for implementing elements of their care coordination approach, such as alert notifications on emergency department and hospital visits or e-care plan tools for virtual care teams. We believe this information would allow us to better understand and support ACOs' plans to put into place the systems and processes needed to deliver high quality care to beneficiaries.
We also note that ACOs have flexibility to use telehealth services as they deem appropriate for their efforts to improve care and avoid unnecessary costs. Some ACOs have already reported that they are actively using telehealth services to improve care for their beneficiaries. We welcome information from ACOs and other stakeholders about the use of such technologies. We seek comment on the specific services and functions of this technology that might be appropriately adopted by ACOs. For example, does the use of telehealth services and other technologies necessitate any additional protections for beneficiaries? Are these technologies necessary for care coordination or could other methods be used for care coordination? If a particular technology is necessary, under what circumstances?
9. Transition of Pioneer ACOs Into the Shared Savings Program
a. Overview
The Center for Medicare and Medicaid Innovation (the Innovation Center) at CMS was established by section 1115A of the Act (as added by section 3021 of the Affordable Care Act) for the purpose of testing “innovative payment and service delivery models to reduce program expenditures . . . while preserving or enhancing the quality of care” for those individuals who receive Medicare, Medicaid, or Children's Health Insurance Program (CHIP) benefits. The Pioneer ACO Model is an Innovation Center initiative designed for organizations with experience operating as ACOs or in similar arrangements. The Pioneer ACO Model is testing the impact of using different payment arrangements in helping these experienced organizations achieve the goals of providing better care to patients, and reducing Medicare costs. Under section 1899(b)(4) of the Act, to be eligible to participate in the Shared Savings Program, a provider of services or supplier may not also be participating in a program or demonstration project that involves shared savings, such as the Pioneer ACO Model. Thus, Pioneer ACOs are not permitted to participate concurrently in the Shared Savings Program. As Pioneer ACOs complete the model test (the agreement is for a minimum of 3 years with an option to participate for an additional 2 years), they would have an opportunity to transition to the Shared Savings Program. We believe it would be appropriate to establish an efficient process to facilitate this transition in a way that minimizes any unnecessary burdens on these ACOs and on CMS.
b. Proposed Revisions
In order to do this, we propose to use a transition process that is similar to the transition process we established previously for Physician Group Practice (PGP) demonstration participants applying to participate in the Shared Savings Program. The PGP demonstration, authorized under section 1866A of the Act, was our first experience with a shared savings program in Medicare and served as a model for many aspects of the Shared Savings Program.
In the November 2011 final rule (76 FR 67834), we finalized § 425.202(b), which provides that PGP sites applying for participation in the Shared Savings Program will be given the opportunity to complete a condensed application form. This condensed application form requires a PGP site to provide the information that was required for the standard Shared Savings Program application but that was not already obtained through its application for or via its participation in the PGP demonstration. Also, a PGP participant Start Printed Page 72780would be required to update any information contained in its application for the PGP demonstration that was also required on the standard Shared Savings Program application. Former PGP participants qualified to use a condensed application form if their ACO legal entity and TINs of ACO participant were the same as those that participated under the PGP demonstration.
As we continue to implement the Shared Savings program, we will likely have a similar situation with regard to Pioneer ACOs that have completed their current agreement and wish to transition to the Shared Savings Program. Given that we have been working with and have a level of familiarity with these organizations similar to that with the PGP participants, we believe it is also appropriate to consider offering some latitude with regard to the process for applying to the Shared Savings Program for these ACOs.
Thus, we propose to revise § 425.202(b) to offer Pioneer ACOs the opportunity to apply to the Shared Savings Program using a condensed application if three criteria are satisfied. First, the applicant ACO must be the same legal entity as the Pioneer ACO. Second, all of the TINs on the applicant's ACO participant list must have appeared on the “Confirmed Annual TIN/NPI List” (as defined in the Pioneer ACO Model Innovation Agreement with CMS) for the applicant ACO's last full performance year in the Pioneer ACO Model. Third, the applicant must be applying to participate in a two-sided model. We note that, consistent with the statute and our regulation at § 425.114, any Pioneer ACO transitioning to the Shared Savings Program must apply to participate in the Shared Savings Program for an agreement period that would start after its participation in the Pioneer ACO Model has ceased. We further note that Pioneer ACOs transitioning to the Shared Savings Program would be subject to the standard program integrity screening and an evaluation of their history of compliance with the requirements of the Pioneer ACO Model.
Regarding the second criterion, we recognize there are differences between the Pioneer ACO Model and the Shared Savings Program, and that only some of the NPIs within a TIN might have participated in the Pioneer ACO. Therefore, for purposes of determining whether a condensed application will be appropriate under the Shared Savings Program, we will only compare the TINs and not NPIs. We also recognize that some TINs may not be able to obtain the consent of all NPIs billing through the TIN to participate in the Shared Savings Program, which disqualifies the TIN from participating in the program. Therefore, unlike with the PGP demonstration sites, we propose to allow the ACO applicant to complete a condensed application form even if it drops TINs that participated in its Pioneer ACO. However, if the applicant ACO includes TINs that were not on the Pioneer ACO's Confirmed Annual TIN/NPI List for its last full performance year in the Pioneer ACO Model, the applicant must use the standard application for the Shared Savings Program. A Pioneer ACO applying to the Shared Savings Program using a condensed application form will be required to include a narrative description of the modifications they need to make to fulfill our requirements (for example, making changes to the governing body and obtaining or revising agreements with ACO participants and ACO providers/suppliers).
Because the Pioneer ACO Model is a risk-bearing model designed for more experienced organizations, the third proposed criterion would permit Pioneer ACOs to use the condensed application only if they apply to participate in the Shared Savings Program under a two-sided model. We established Track 1 of the Shared Savings Program as an on-ramp for ACOs while they gain experience and become ready to accept risk. In this case, the Pioneer ACOs are already experienced and will have already accepted significant financial risk. Therefore, under this proposal, former Pioneer ACOs would not be permitted to enter the Shared Savings Program under Track 1. We further note that the rules and methodologies used under the Pioneer ACO Model to assess performance-based risk are different than under the Shared Savings Program. Therefore, we encourage former Pioneer Model ACOs to carefully consider the risk-based track to which they apply under the Shared Savings Program, and to be cognizant of the differences in rules and methodologies.
We seek comments on this proposal to establish a condensed application process for Pioneer ACOs applying to participate in the Shared Savings Program and to require such Pioneer ACOs to participate under a track that includes performance-based risk. Pioneer ACOs that do not meet criteria for the condensed application would have to apply through the regular application process.
C. Establishing and Maintaining the Participation Agreement With the Secretary
1. Background
The November 2011 final rule established procedures for applying to participate in the Shared Savings Program, including the need to submit a complete application, the content of the application, and CMS's criteria for evaluating applications (see § 425.202 through § 425.206). In addition, § 425.212 specifies which changes to program requirements will apply during the term of an ACO's participation agreement. In this section we discuss our proposals to clarify and to supplement the rules related to these requirements.
In addition, while the current regulations address certain issues with respect to ACOs that wish to reapply after termination or experiencing a loss during their initial agreement period (§ 425.222 and § 425.600(c), respectively). The regulations are generally silent with respect to the procedures that apply to ACOs that successfully complete a 3-year agreement and would like to reapply for a subsequent agreement period in the Shared Savings Program. In this section, we discuss our proposal to establish the procedure for an ACO to renew its participation agreement for a subsequent agreement period.
2. Application Deadlines
a. Overview
To obtain a determination on whether a prospective ACO meets the requirements to participate in the Shared Savings Program, our rules at § 425.202(a) require that an ACO submit a complete application in the form and manner required by CMS by the deadline established by CMS. Information on the required content of applications can be found in § 425.204, as well as in guidance published at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Application.html. Among other requirements, applications must include certain information such as an ACO's prior participation in or termination from the program (§ 425.204(b)); documents such as participation agreements, employment contracts and operating policies (§ 425.204(c)(1)(i)); and a list of all ACO participants and their Medicare-enrolled TINs (§ 425.204(c)(5)(i)).
We determine and publish in advance on our Web site the relevant due dates for the initial submission of applications Start Printed Page 72781for each application cycle. While ACOs must submit a completed application by the initial application due date specified on our Web site, we recognize that there may be portions of the application where additional information is necessary for CMS to make a determination. Therefore, according to § 425.206(a)(2), we notify an applicant when its application is incomplete and provide an opportunity to submit information to complete the application by the deadline specified by CMS.
As stated in § 425.206(a), CMS evaluates an ACO's application on the basis of the information contained in and submitted with the application. Applications that remain incomplete after the deadline specified by CMS are denied. It is incumbent upon the ACO applicant to submit the information that is required for CMS to decide whether the applicant is eligible to participate in the program.
b. Proposed Revisions
In implementing the Shared Savings Program, we found that some applicants misunderstood our application process and the need to submit all required information by the specified deadline for submission of applications and supporting information. Thus, we propose to revise our application review process set forth at § 425.206(a) to better reflect our review procedures.
First, we propose to consolidate at § 425.206 two similar provisions regarding application review. Currently, § 425.202(c)(1) regarding application review provides that CMS determines whether an applicant satisfies the requirements of Part 425 and is qualified to participate in the Shared Savings Program, and § 425.202(c)(2) provides that CMS approves or denies applications accordingly. We propose to amend § 425.206(a)(1) to address the concept of application review currently set forth at § 425.202(c)(1), and we propose to amend § 425.202(c) by replacing the existing text with language clarifying that CMS reviews applications in accordance with § 425.206.
Second, we propose to revise § 425.206(a) to better reflect our application review process and the meaning of the reference to “application due date.” Specifically, we propose to revise § 425.206(a)(1) to clarify that CMS approves or denies an application on the basis of the following: Information contained in and submitted with the application by the deadline specified by CMS; any supplemental information submitted by a deadline specified by CMS in response to CMS' request for information; and other information available to CMS (including information on the ACO's program integrity history). In addition, we propose to amend § 425.206(a)(2) to clarify our process for requesting supplemental information and to add a new paragraph (a)(3) to specify that CMS may deny an application if an ACO applicant fails to submit information by the deadlines specified by CMS. We believe that additional clarity may result in more timely submission of the information necessary to evaluate applications. Moreover, it is critical that ACOs submit information on a timely basis so that we can perform other necessary operational processes before the start of the approved ACO's first performance year (for example, determining the number of beneficiaries assigned to the ACO, screening prospective ACO participants and ACO providers or suppliers, identifying the preliminary prospective list of assigned beneficiaries, and calculating the ACO's historical benchmark).
These proposed changes are consistent with our current regulations and practice. For example, as part of the application review process, CMS provides feedback to the ACO applicant regarding its list of ACO participants, and the number of assigned beneficiaries is determined using this list of ACO participants. If the number of assigned beneficiaries based on the list of ACO participants submitted with the application is under 5,000, which is the threshold for eligibility under § 425.110(a), we give the ACO applicant an opportunity to add ACO participant TINs. However, the ACO applicant must do so by the deadline indicated by CMS or the application is denied. Similarly, CMS denies an application if an ACO applicant fails to timely submit additional information that is required for CMS to determine whether the ACO applicant meets program requirements.
3. Renewal of Participation Agreements
a. Overview
For ACOs that would like to continue participating in the Shared Savings Program after the expiration of their current agreement period, we propose a process for renewing their existing participation agreements, rather than requiring submission of a new or condensed application for continued program participation. Therefore, we propose to add new § 425.224 to establish procedures for renewing the participation agreements of ACOs. In addition, we propose to modify the definition of “agreement period” at § 425.20 to clarify its meaning in the context of participation agreement renewals.
b. Proposed Revisions
Under proposed § 425.224(a), an ACO would be permitted to request renewal of its participation agreement prior to its expiration in a form and manner and by the deadline specified by CMS in guidance. An ACO executive who has the authority to legally bind the ACO must certify that the information contained in the renewal request is accurate, complete, and truthful. Further, an ACO that seeks renewal of its participation agreement and was newly formed after March 23, 2010, as defined in the Antitrust Policy Statement, must agree that CMS can share a copy of its renewal request with the Antitrust Agencies. We anticipate that our operational guidance will outline a process permitting renewal requests during the last performance year of an ACO's participation agreement. For example, an ACO with a participation agreement ending on December 31, 2015 would be offered the opportunity to renew its participation agreement sometime during the 2015 calendar year in preparation to begin a new 3-year agreement period on January 1, 2016. To streamline program operations, we anticipate specifying a timeframe for submission and supplementation of renewal requests that would generally coincide with the deadlines applicable to submission and supplementation of applications by new ACO applicants under § 425.202.
Under proposed § 425.224(b), we propose to determine whether to renew a participation agreement based on an evaluation of all of the following factors:
- Whether the ACO satisfies the criteria for operating under the selected risk model.
- The ACO's history of compliance with the requirements of the Shared Savings Program.
- Whether the ACO has established that it is in compliance with the eligibility and other requirements of the Shared Savings Program, including the ability to repay losses, if applicable.
- Whether the ACO met the quality performance standards during at least 1 of the first 2 years of the previous agreement period.
- Whether an ACO under a two-sided model has repaid losses owed to the program that it generated during the first 2 years of the previous agreement period.
- The results of a program integrity screening of the ACO, its ACO participants, and its ACO providers/suppliers (conducted in accordance with § 425.304(b)).Start Printed Page 72782
We solicit comments on these criteria and any additional criteria that would help ensure the success of the program.
We further propose to approve or deny a renewal request based on the information submitted in the request and other information available to CMS. We propose to notify the ACO when the request is incomplete or inadequate and to provide an opportunity for the ACO to submit supplemental information to correct the deficiency. The ACO must submit both the renewal request and any additional information needed to evaluate the request in the form and manner and by the deadlines specified by CMS.
Under § 425.224(c), we propose to notify each ACO in writing of our determination to approve or deny the ACO's renewal request. If we deny the renewal request, the notice would specify the reasons for the denial and inform the ACO of any rights to request reconsideration review in accordance with the procedures specified in part 425 subpart I.
We believe that a simple renewal process would reduce the burden for ACOs that wish to continue in the program and minimize the administrative burden on CMS, which would allow us to focus our attention on new applicants that have not yet established their eligibility to participate. We intend to establish the deadlines and other operational details for this renewal process through guidance and instructions. Finally, we note that under our proposal to modify the definition of the participation “agreement period” (section II.C.4 of this proposed rule), a new agreement period would begin upon the start of the first performance year of the renewed participation agreement.
4. Changes to Program Requirements During the 3-Year Agreement
a. Overview
In the November 2011 final rule (76 FR 67838), we recognized that we might promulgate changes to the Shared Savings Program regulations that would become effective while participating ACOs are in the middle of an agreement period. Therefore, we promulgated a rule to specify under what conditions an ACO would be subject to regulatory changes that become effective after the start of its agreement period. Specifically, we finalized § 425.212(a)(2), which provides that ACOs are subject to all regulatory changes with the exception of changes to the eligibility requirements concerning ACO structure and governance, the calculation of the sharing rate, and the assignment of beneficiaries (§ 425.212(a)(2)). We did not exempt ACOs from becoming immediately subject to other regulatory changes. For example, we did not exempt changes such as those related to quality measures because we believed that requiring ACOs to adhere to changes related to quality measures would ensure that they keep pace with changes in clinical practices and developments in evidence-based medicine.
The November 2011 final rule did not require ACOs to be subject to any regulatory changes regarding beneficiary assignment that become effective during an agreement period because we recognized that changes in the beneficiary assignment methodology could necessitate changes to ACOs' financial benchmarks. At the time we published the November 2011 final rule (76 FR 67838), we had not developed a methodology for adjusting an ACO's benchmark to reflect changes in the beneficiary assignment methodology during an agreement period. We anticipated that ACOs would complete their 3-year agreement period with a relatively stable set of ACO participants, and therefore they would all have stable benchmarks during the 3-year agreement period that would require updates only to reflect annual national FFS trends and changes in beneficiary characteristics, consistent with statutory requirements. Without a methodology for adjusting benchmarks to reflect changes in the beneficiary assignment methodology during the agreement period, we were reluctant to subject ACOs to immediate regulatory changes that could impact their benchmarks during the term of a participation agreement. However, in light of the extensive changes that ACOs have made to their lists of ACO participants during the first two performance years, the significant effect that these changes have had upon beneficiary assignment, and our subsequent development of additional policies regarding benchmark adjustment at the start of each performance year to reflect such changes (see http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Updating-ACO-Participant-List.html), we wish to revisit the types of regulatory changes an ACO would become subject to during its agreement period. We also propose to clarify § 425.212(a) regarding the applicability of certain regulatory changes and to clarify the definition of “agreement period” under § 425.20.
b. Proposed Revisions
First, we propose to modify § 425.212(a) to provide that ACOs are subject to all regulatory changes “that become effective during the agreement period,” except for regulations regarding certain specified program areas, “unless otherwise required by statute.” This proposed revision corrects the omission of temporal language in the requirement regarding regulatory changes. In addition, it clarifies that ACOs would be subject to regulatory changes regarding ACO structure and governance, and calculation of the sharing rate during an agreement period if CMS is mandated by statute to implement such changes by regulation in the middle of a performance year.
Second, we propose to modify the definition of “agreement period” at § 425.20. The term “agreement period” is currently defined at § 425.20 to mean “the term of the participation agreement which begins at the start of the first performance year and concludes at the end of the final performance year.” However, the reference to “final performance year” in the existing definition is ambiguous in light of our proposal to renew participation agreements (see section II.C.4. of this proposed rule). For example, if the “final performance year” of the agreement period includes the last performance year of a renewed participation agreement, an ACO would never be subject to regulatory changes regarding ACO structure and governance or calculation of the sharing rate. Therefore, we propose to amend the definition to provide that the agreement period would be 3 performance years, unless otherwise specified in the participation agreement. Thus, an ACO whose participation agreement is renewed for a second or subsequent agreement period would be subject, beginning at the start of that second or subsequent agreement period, to any regulatory changes regarding ACO structure and governance that became effective during the previous 3 years (that is, during the preceding agreement period).
Third, we propose to require ACOs to be subject to any regulatory changes regarding beneficiary assignment that become effective during an agreement period. Specifically, we propose to remove beneficiary assignment as an exception under § 425.212(a). Consistent with our authority under section 1899(d)(1)(B)(ii) of the Act to adjust the benchmark “for beneficiary characteristics and other factors as the Secretary determines appropriate,” we have now developed operational Start Printed Page 72783policies under which we are able to adjust the benchmark on a yearly basis to account for changes in beneficiary assignment resulting from changes in the ACO's list of ACO participants. For more detailed information on these policies see http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Updating-ACO-Participant-List.html. Given that these operational policies enable annual adjustments to ACO benchmarks to account for changes in beneficiary assignment resulting from changes in ACO participants, we believe we would also be able to adjust an ACO's benchmark to account for regulatory changes regarding beneficiary assignment methodology that become effective during an agreement period. Accordingly, we do not believe our proposal to make regulatory changes regarding beneficiary assignment applicable to ACOs during an agreement period would inappropriately affect the calculation of an ACO's benchmark or shared savings for a given performance year. Rather, our adjustment methodology would ensure continued and appropriate comparison between benchmark and performance year expenditures.
Under this proposal, regulatory changes regarding beneficiary assignment would apply to all ACOs, including those ACOs that are in the middle of an agreement period. However, as discussed in section II.E.6. of this proposed rule, we also propose that any final policies that affect beneficiary assignment would not be applicable until the start of the next performance year. We believe that implementing any revisions to the assignment methodology at the beginning of a performance year is reasonable and appropriate because it would permit time for us to make the necessary programming changes and would not disrupt the assessment of ACOs for the current performance year. Moreover, we would adjust all benchmarks at the start of the first performance year in which the new assignment rules are applied so that the benchmark for an ACO reflects the use of the same assignment rules that would apply in the performance year.
We also note that we carefully consider the timing and effect on both current and future ACOs of any new regulatory proposal, and when promulgating new regulatory changes, we intend to solicit comment on these matters. Additionally, when implementing a final rule that changes our processes and methodologies, we intend to alert current and prospective ACOs of such changes via CMS communications and updates to guidance. We request comment on this proposed change to § 425.212(a).
D. Provision of Aggregate and Beneficiary Identifiable Data
1. Background
Under section 1899(b)(2)(A) of the Act, an ACO must “be willing to become accountable for the quality, cost, and overall care of the Medicare fee-for-service beneficiaries assigned to it.” Further, in order to be eligible to participate in the Shared Savings Program, section 1899(b)(2)(G) of the Act states an “ACO shall define processes to . . . report on quality and cost measures, and coordinate care. . . .” However, section 1899 of the Act does not address what data, if any, we should make available to ACOs on their assigned beneficiary populations to support them in evaluating the performance of ACO participants and ACO providers/suppliers, conducting quality assessment and improvement activities, or conducting population-based activities relating to improved health.
As we explained in the November 2011 final rule (76 FR 67844), in agreeing to become accountable for a group of Medicare beneficiaries, and as a condition of participation in the Shared Savings Program, we expect that ACOs will have, or are working towards having, processes in place to independently identify and produce the data they believe are necessary to best evaluate the health needs of their patient population, improve health outcomes, monitor provider/supplier quality of care and patient experience of care, and produce efficiencies in utilization of services. Therefore, it is our expectation that ACOs are actively working on developing and refining these processes. Moreover, we continue to believe this ability to independently identify and produce data for evaluating, improving, and monitoring the health of their patient population is a critical skill for each ACO to develop, leading to an understanding of the patient population that it serves. Once the ACO achieves an understanding of its patient population, it can work toward redesigning appropriate care processes to address the specific needs of its patient population.
However, as we noted previously (76 FR 67844), while an ACO typically should have, or at least be moving towards having complete information for the services its ACO providers/suppliers furnish to Medicare FFS beneficiaries, we recognize that the ACO may not have access to information about services provided to its assigned beneficiaries by health care providers and suppliers outside the ACO—information that may be key to the ACO's coordination of care efforts. Therefore, during the original rulemaking process for the Shared Savings Program, we proposed and made final a policy: (1) To distribute aggregate-level data reports to ACOs; (2) upon request from the ACO, to share limited identifying information about beneficiaries who are preliminarily prospectively assigned to the ACO and whose information serves as the basis for the aggregate reports; and (3) upon request from the ACO, to share certain beneficiary identifiable claims data with the ACO to enable it to conduct quality assessment and improvement activities and/or conduct care coordination, on its own behalf as a covered entity, or on behalf of its ACO participants and ACO providers/suppliers that are covered entities, unless the beneficiary chooses to decline to share his or her claims data.
As we stated in the November 2011 final rule (76 FR 67844), we believe that access to beneficiary identifiable information would provide ACOs with a more complete picture about the care their assigned beneficiaries receive, both within and outside the ACO. Further, it is our view that this information would help ACOs evaluate providers'/suppliers' performance, conduct quality assessment and improvement activities, perform care coordination activities, and conduct population-based activities relating to improved health.
In the April 2011 proposed rule (76 FR 19558), we described the circumstances under which we believed that the HIPAA Privacy Rule would permit our disclosure of certain Medicare Part A and B data to ACOs participating in the Shared Savings Program. Specifically, under the Shared Savings Program statute and regulations, ACOs are tasked with working with their ACO participants and ACO providers/suppliers to evaluate their performance, conduct quality assessment and improvement activities, perform care coordination activities, and conduct population-based activities relating to improved health for their assigned beneficiary population. When done by or on behalf of a covered entity, these are functions and activities that would qualify as “health care operations” under the first and second paragraphs of the definition of health care operations at 45 CFR 164.501. As such, these activities can be done by an ACO either on its own behalf, if it is itself a covered entity, or on behalf of its covered entity ACO participants and Start Printed Page 72784ACO providers/suppliers, in which case the ACO would be acting as the business associate of its covered entity ACO participants and ACO providers/suppliers. Accordingly we concluded that the disclosure of Part A and B claims data would be permitted by the HIPAA Privacy Rule provisions governing disclosures for “health care operations,” provided certain conditions are met.
As we also discussed, upon receipt of a request for protected health information (PHI), a covered entity or its business associate is permitted to disclose PHI to another covered entity or its business associate for the requestor's health care operations if both entities have or had a relationship with the subject of the records to be disclosed (which is true in the Shared Savings Program), the records pertain to that relationship (which is also true in the Shared Savings Program), and the recipient asserts in its request for the data that it plans to use the records for a “health care operations” function that falls within the first two paragraphs of the definition of “health care operations” in the HIPAA Privacy Rule and that the data requested are the “minimum necessary” to carry out those health care operations. (See, the HIPAA Privacy Rule at 45 CFR 164.502(b) and 164.506(c)(4)). The first two paragraphs of the definition of health care operations under 45 CFR 164.501 include evaluating a provider's or supplier's performance, conducting quality assessment and improvement activities, care coordination activities, and conducting population-based activities relating to improved health.
With respect to the relationship requirements in 45 CFR 164.506(c)(4), we have a relationship with the individuals who are the subjects of the requested PHI because they are Medicare beneficiaries. The ACO has a relationship with such individuals, either as a covered entity itself or on behalf of its covered entity ACO participants and ACO providers/suppliers as a business associate, because the individuals are either preliminarily prospectively assigned to the ACO or have received a primary care service during the past 12 month period from an ACO participant upon whom assignment is based. In addition, the requested PHI pertains to the individuals' relationship with both CMS and the ACO, in that we provide health care coverage for Medicare FFS beneficiaries and have an interest in ensuring that they receive high quality and efficient care, and the ACO is responsible for managing and coordinating the care of these individuals, who are part of the ACO's assigned beneficiary population.
Beneficiary identifiable Medicare prescription drug information could also be used by ACOs to improve the care coordination of their patient populations. Accordingly, consistent with the regulations governing the release of Part D data, in the April 2011 proposed rule (76 FR 19559), we also proposed to make available the minimum Part D data necessary to allow for the evaluation of the performance of ACO participants and ACO providers/suppliers, to conduct quality assessment and improvement, to perform care coordination, and to conduct population-based activities relating to improved health.
In the November 2011 final rule (76 FR 67846 and 67851), we adopted a policy that defined when we would share beneficiary identifiable information (including Part A and B claims data and Part D prescription drug event data) for preliminarily prospectively assigned beneficiaries and those beneficiaries who have a primary care visit with an ACO participant that is used to assign beneficiaries to the ACO. As a basic requirement, in order to receive such data an ACO that chooses to access beneficiary identifiable data is required under 42 CFR 425.704 to request the minimum data necessary for the ACO to conduct health care operations work, either as a HIPAA-covered entity in its own right, or as the business associate of one or more HIPAA-covered entities (where such covered entities are the ACO participants and ACO providers/suppliers), for “health care operations” activities that fall within the first or second paragraph of the definition of health care operations at 45 CFR 164.501. We note that as part of their application to participate in the Shared Savings Program, ACOs certify whether they intend to request beneficiary identifiable information, and that the requested data reflects the minimum necessary for the ACO to conduct health care operations either on its own behalf or on behalf of its covered entity ACO participants and ACO provider/suppliers. Thus, the ACO's formal request to receive data is accomplished at the time of its application to the Shared Savings Program. The ACO must also enter into a data use agreement (DUA) with CMS. If all of these conditions are satisfied, CMS makes available certain limited PHI regarding the preliminarily prospectively assigned beneficiaries whose data were used to generate the aggregate data reports provided to the ACO under § 425.702(b) and other beneficiaries who have a primary care visit during the performance year with an ACO participant upon whom assignment is based. In order to enhance transparency and beneficiary engagement, we also finalized a policy that before ACOs may start receiving PHI in the form of beneficiary identifiable claims data, they must give beneficiaries the opportunity to decline sharing of their claims data as required under § 425.708.
Since the publication of the November 2011 final rule, we have gained further experience with sharing data with ACOs participating in the Shared Savings Program. We continue to believe that distributing aggregate reports, paired with making available certain beneficiary identifiable information related to preliminarily prospectively assigned beneficiaries, as well as making available the claims data for preliminarily prospectively assigned FFS beneficiaries and other FFS beneficiaries that have primary care service visits with ACO participants that submit claims for primary care services that are used to determine the ACO's assigned population, is worthwhile and consistent with the goals of the Shared Savings Program. The aggregate data reports and the beneficiary identifiable information related to preliminarily prospectively assigned beneficiaries give ACOs valuable information that can be used to better understand their patient population, redesign care processes, and better coordinate the care of their beneficiaries. ACOs participating in the Shared Savings Program have reported that the beneficiary identifiable claims data that they receive from us are being used effectively to better understand the FFS beneficiaries that are served by their ACO participants and ACO providers/suppliers. These data give ACOs valuable insight into patterns of care for their beneficiary population; enable them to improve care coordination among and across providers and suppliers and sites of care, including providers and suppliers and sites of care not affiliated with the ACO; and allow them to identify and address gaps in patient care.
However, based upon our experiences administering the Shared Savings Program and feedback from stakeholders, we believe that we can improve our data sharing policies and processes to streamline access to such data to better support program and ACO function and goals and better serve Medicare beneficiaries. It is with this in mind that we propose the following modifications to our data sharing policies and procedures under the Shared Savings Program.Start Printed Page 72785
2. Aggregate Data Reports and Limited Identifiable Data
a. Overview
Under § 425.702, we share aggregate reports with ACOs at the beginning of the agreement period based on beneficiary claims used to calculate the benchmark, at each quarter thereafter on a rolling 12-month basis, and in conjunction with the annual reconciliation. The aggregate reports provided under § 425.702(a) and (b) contain certain de-identified beneficiary information including all of the following:
- Aggregated metrics on the ACO's preliminarily prospectively assigned beneficiary population, including characteristics of the assigned beneficiary population, the number of primary care services provided to the assigned beneficiary population by the ACO, and the proportion of primary care services provided to the assigned beneficiary population by ACO participants upon whom assignment is based.
- Expenditure data for the ACO's assigned beneficiary population by Medicare enrollment type (ESRD, disabled, aged/dual eligible, aged/non-dual eligible) and type of service (for example, inpatient hospital, physician, etc.).
- Utilization data on select metrics for the assigned population, such as ambulatory care sensitive conditions discharge rates per 1,000 beneficiaries for conditions such as congestive heart failure (CHF) or uncontrolled diabetes, and utilization rates for imaging, emergency department visits, hospitalizations, and primary care services.
In addition, under § 425.702(c), we also provide a report that includes certain beneficiary identifiable information about the beneficiaries who are preliminarily prospectively assigned to the ACO and whose data were used to generate the de-identified aggregate data reports. The information currently contained in this assignment report includes the beneficiary name, date of birth, HICN, and sex. These beneficiary identifiable data are made available to an ACO that has met the conditions previously discussed in detail for purposes of carrying out population-based activities related to improving health or reducing growth in health care costs, process development (such as care coordination processes), case management, and care coordination for the beneficiary population assigned to the ACO. Under § 425.708(d) these data points are not subject to the requirement that an ACO give beneficiaries an opportunity to decline claims data sharing.
Feedback we have received since the November 2011 final rule was issued and during implementation of the Shared Savings Program, confirms there is a strong desire among ACOs and their ACO participants and ACO providers/suppliers to have as much information about their patients as is possible, in as timely a manner as possible, to better coordinate care and target care strategies toward individual beneficiaries. Moreover, ACOs are actively using the reports provided under § 425.702 to conduct their health care operations work with the expectation that it will result in higher quality and more efficient care for their assigned beneficiary populations. However, ACOs and their ACO participants and ACO providers/suppliers also report that the four data elements currently made available on the assignment reports under § 425.702(c)—that is, beneficiary name, date of birth, HICN, and sex—severely limit their care redesign efforts. They assert that additional data elements are necessary in order to conduct health care operations work under the first or second paragraph of the definition of health care operations at 45 CFR 164.501. For example, an ACO reported that having data not only on the frequency of hospitalizations but also on which specific beneficiaries were hospitalized and in which specific hospitals would better enable it to identify the effectiveness and outcomes of its post-hospitalization care coordination processes. Some stakeholders have made suggestions for beneficiary identifiable data that should be included in the quarterly reports in addition to the current four data elements, such as risk profiles or information on whether the beneficiary had a hospital visit in the past year. Some stakeholders suggested that the report be expanded to include information not only for the beneficiaries that received a plurality of their primary care services from ACO professionals, but also for all FFS beneficiaries that received a primary care service from an ACO participant in the past year. These stakeholders argue that understanding the entire FFS patient population served by the ACO and its ACO participants would improve their ability to redesign care, and reduce the uncertainty associated with a list of preliminarily prospectively assigned beneficiaries that fluctuates from quarter to quarter, based on the population's use of primary care services.
b. Proposed Revisions
We considered what additional beneficiary identifiable data might be the minimum necessary to support the ACOs' health care operations work. Based on our discussions with ACOs and ACO participants and ACO providers/suppliers, we believe that making additional information available to ACOs about the FFS beneficiaries they serve, including for example, on whether a beneficiary visited an emergency room or was hospitalized, would help support such efforts. Thus, we propose to expand the information made available to ACOs under § 425.702(c) to include certain additional beneficiary identifiable data subject to the existing requirements of § 425.702(c)(2), which incorporates the requirements under HIPAA governing the disclosure of PHI. Specifically, in addition to the four data elements (name, date of birth, HICN, and sex) which are currently made available for preliminarily prospectively assigned beneficiaries, we propose to expand the beneficiary identifiable information that is made available under § 425.702(c)(1) to include these data elements (name, date of birth, HICN, and sex) for each beneficiary that has a primary care service visit with an ACO participant that bills for primary care services that are considered in the assignment process in the most recent 12-month period.
Additionally, we propose to expand the beneficiary identifiable information made available for preliminarily prospectively assigned beneficiaries to include additional data points. The information would be derived from the same claims used to determine the preliminary prospective assigned beneficiary list. Specifically, we propose that we would make available the minimum data set necessary for purposes of the ACO's population-based activities related to improving health or reducing health care costs, required process development (under § 425.112), care management, and care coordination for its preliminarily prospectively assigned beneficiary population, at the following times: (1) At the beginning of the agreement period; (2) at the beginning of each performance year and quarterly thereafter; and (3) in conjunction with the annual reconciliation. We would articulate the data elements associated with the minimum data set in operational guidance, and update as needed to reflect changes in the minimum data necessary for ACOs to perform these activities. The information would fall under the following categories:Start Printed Page 72786
- Demographic data such as enrollment status.
- Health status information such as risk profile, and chronic condition subgroup.
- Utilization rates of Medicare services such as the use of evaluation and management, hospital, emergency, and post-acute services, including dates and place of service.
- Expenditure information related to utilization of services.
We believe that under this approach the data made available in the aggregate data reports under § 425.702(c) would generally constitute the minimum data necessary for covered entity ACOs or for ACOs serving as the business associate of their covered entity ACO participants and ACO providers/suppliers, to evaluate providers' and suppliers' performance, conduct quality assessment and improvement activities, and conduct population-based activities relating to improved health.
Finally, we note that these proposals for expansion of the data reports provided under § 425.702(c) to include each FFS beneficiary that has a primary care visit with an ACO participant that submits claims for primary care services that are considered in the assignment process, would apply only to ACOs participating in Tracks 1 and 2, where beneficiaries are assigned in a preliminarily prospective manner with retrospective reconciliation. This is because ACOs in Tracks 1 and 2 have an incentive to redesign care processes for all FFS beneficiaries that receive care from their ACO participants, due to the nature of the preliminarily prospective assignment methodology with retrospective reconciliation. Under our proposed Track 3, which is discussed in detail in section II.F.3.a. of this proposed rule, we believe that the minimum data necessary for ACOs to perform health care operations as defined under the first and second paragraphs of the definition of health care operations at 45 CFR 164.501, would not extend beyond data needed for health operations related to the prospective list of assigned beneficiaries. We believe a prospective assignment approach incentivizes targeting of the specific FFS beneficiaries on the list for care improvement, rather than redesigning care processes for all FFS beneficiaries seen by the ACO participants. As such, the minimum data necessary required for Track 3 ACOs to perform health care operations work would be limited to the data for beneficiaries that are prospectively assigned for a performance year. Thus, for Track 3, we propose to limit the beneficiary identifiable data included in the reports made available under § 425.702(c) to only those beneficiaries that appear on the ACO's prospective list of beneficiaries at the beginning of a performance year. Specifically, Track 3 ACOs would have access to beneficiary identifiable data elements associated with the list of categories under § 425.702(c) for beneficiaries prospectively assigned to the ACO but would not be able to request any information related to other Medicare FFS beneficiaries who receive primary care services that are considered in the assignment process from ACO participants. We believe this limitation is reasonable because, under Track 3, the prospectively assigned beneficiary list would encompass all beneficiaries for whom the ACO would be held accountable in a given performance year, in contrast to ACOs in Tracks 1 and 2 that would be held accountable for any FFS beneficiaries that choose to receive a plurality of their primary care services from ACO professionals billing through the TINs of ACO participants.
We seek comment on our proposal to expand the data set made available to ACOs under § 425.702(c). We seek comment on the categories of information that we have proposed to include and on any other beneficiary identifiable information that should be offered in the aggregate reports provided under § 425.702(c) in order to allow ACOs as covered entities or as the business associate of their covered entity ACO participants and ACO providers/suppliers to conduct health care operations work under paragraphs one or two of the definition of health care operations at 45 CFR 164.501. We also specifically seek comment on our proposal to expand the list of beneficiaries for which data are made available under § 425.702(c) to ACOs participating in Track 1 and Track 2 to include all beneficiaries that had a primary care service visit with an ACO participant that submits claims for primary care services that are considered in the assignment process.
3. Claims Data Sharing and Beneficiary Opt-Out
a. Overview
Because Medicare FFS beneficiaries have the freedom to choose their health care providers and suppliers, and are not required to receive services from providers and suppliers participating in the ACO, the patients of ACO participants and ACO providers/suppliers often receive care from other providers and suppliers that are not affiliated with the ACO. As a result, ACOs and their ACO participants and ACO providers/suppliers may not be aware of all of the services an assigned beneficiary is receiving. Furthermore, under Tracks 1 and 2, we perform a retrospective reconciliation at the end of each performance year to determine an ACO's assigned beneficiary population based on beneficiaries' use of primary care services using the assignment algorithm described at § 425.402 of the regulations. Therefore, under Tracks 1 and 2, it is possible that an ACO's preliminary prospective assigned beneficiary list would not be complete and would not include all the beneficiaries that would ultimately be assigned to the ACO at the end of the performance year—that is, all of the beneficiaries for which the ACO ultimately would be held accountable. As we discussed in the April 2011 proposed rule (76 FR 19558) and in the November 2011 final rule (76 FR 67844), we were concerned about ACOs' ability to do their work in the absence of information about services delivered outside of the ACO. As we stated at that time, we believed that it would be important to give ACOs appropriate access to a beneficiary's identifiable claims data when the beneficiary has received a primary care service billed through the TIN of an ACO participant, and is thus a candidate for assignment at the time of retrospective reconciliation for the performance year. We believed that sharing beneficiary identifiable claims data would enable ACOs to better coordinate and target care strategies towards the individual beneficiaries seen by ACO participants and ACO providers/suppliers.
We ultimately concluded that the bases for disclosure under the HIPAA Privacy Rule were broad enough to cover CMS's disclosure of Medicare Parts A and B claims data to ACOs for health care operations work when certain conditions are met. Similarly, we concluded that the Part D regulations governing the release of Part D data on prescription drug use would permit the release of Part D prescription drug event data to ACOs for purposes of supporting care coordination, quality improvement, and performance measurement activities. Thus, we concluded that we are permitted to disclose the minimum Medicare Parts A, B, and D data necessary to allow ACOs to conduct the health care operations activities that fall into the first or second paragraph of the definition of health care operations under the HIPAA Privacy Rule when such data is requested by the ACO as a covered entity or as the business Start Printed Page 72787associate of its covered entity ACO participants and ACO providers/suppliers. Accordingly, in the November 2011 final rule (76 FR 67851), we adopted a policy under which an ACO may request Part A and Part B claims data and Part D prescription drug event data for preliminarily prospectively assigned beneficiaries and other beneficiaries who receive primary care services from an ACO participant upon whom assignment is based. In accordance with the terms of the DUA that the ACO must enter into with CMS, data received from CMS under the data sharing provisions of the Shared Savings Program may only be used for the purposes of clinical treatment, care management and coordination, quality improvement activities, and provider incentive design and implementation. In providing the claims data subject to these limitations, we believed that we would ensure compliance with the requirements of the HIPAA Privacy Rule and the regulations governing the release of Part D data.
While the disclosure of claims data in this manner is within the bounds of the applicable laws, we also noted concerns about beneficiaries' interests in controlling access to their individually identifiable health information. Thus, even though we believed that we had legal authority to make the contemplated disclosures without the consent of beneficiaries, in the November 2011 final rule (76 FR 67849) we implemented the additional requirement at § 425.708 that ACOs offer beneficiaries an opportunity to decline to have their claims data shared with the ACO. As such, before requesting access to the beneficiary's data and as part of its broader activities to notify patients that their health care provider or supplier is participating in an ACO, the ACO is required to inform beneficiaries that the ACO may request access to their claims data, and give beneficiaries an opportunity to decline such claims data sharing.
Under the current opt-out system, once the ACO formally requests beneficiary identifiable claims data through the application process, enters into a DUA with CMS, and begins its first performance year, the ACO must supply beneficiaries with a written notification explaining their opportunity to decline claims data sharing. Offering beneficiaries the opportunity to decline claims data sharing may take two forms under current § 425.708. First, if the ACO has formally requested beneficiary identifiable claims data as part of the application process, the ACO must notify each FFS beneficiary of the opportunity to decline data sharing when the beneficiary has his or her first visit with an ACO participant upon whom assignment is based. During this visit, the beneficiary must be provided with written notification informing him or her of the ACO provider/supplier's participation in the ACO and that the ACO may request claims information from CMS in order to better coordinate the beneficiary's care and for other health operations activities. This written notification contains template language created by CMS with the assistance of the Medicare Ombudsman's office and with input from beneficiaries, and explains the beneficiary's option to decline claims data sharing. Once the beneficiary has expressed a preference at the point of care, the ACO may immediately inform CMS of the beneficiary's data sharing preference. If the beneficiary has not declined data sharing, CMS makes that beneficiary's data available to the ACO.
We recognized, however, that beneficiaries may not seek primary care services until later in the performance year. Because of this, we offered an alternative option to ACOs who met requirements for receiving beneficiary identifiable claims data. Under the alternative option, ACOs may contact beneficiaries via a mailed notification that is sent to all preliminarily prospectively assigned beneficiaries to notify them of their health care provider's participation in an ACO under the Shared Savings Program, and the ACO's intent to request beneficiary identifiable claims data. The mailed notification contains template language that was developed in conjunction with the Medicare Ombudsman's office with input from beneficiaries. If the beneficiary wishes to decline claims data sharing, the beneficiary is instructed to sign the mailed notification and return it to the ACO or call 1-800-MEDICARE directly. If the ACO chooses to contact beneficiaries via a mailed notification, rather than waiting to notify them at the point of care, the ACO must wait 30 days before submitting the beneficiary's preference and receiving access to the data for those beneficiaries that have chosen not to decline claims data sharing. The 30-day waiting period provides beneficiaries with an opportunity to mail back the notification or to call 1-800-MEDICARE before the ACO receives access to their claims data. In addition, in order to ensure transparency, beneficiary engagement and meaningful choice, the notification and opportunity to decline claims data sharing must be repeated at the beneficiary's first primary care visit with an ACO participant upon whom assignment is based (76 FR 67850 and 67851). Finally, in addition to the point of care and mailed notifications provided by ACOs, all Medicare FFS beneficiaries are notified through the Medicare & You Handbook about ACOs and the opportunity to decline claims data sharing by contacting CMS directly at 1-800-MEDICARE.
Once the ACO has notified the beneficiaries according to program rules, and any applicable wait periods are over, the ACO submits the beneficiaries' preferences to CMS. Beneficiary preferences submitted by ACOs are combined with preferences received by CMS through 1-800-MEDICARE. Based on these beneficiary preferences, we generate a claims file containing the beneficiary identifiable claims data of beneficiaries that have not declined data sharing. These claims files are then made available for ACO access on a monthly basis.
Once a beneficiary has declined data sharing, the beneficiary may choose to reverse the decision by signing another form and sending it to the ACO (who in turn notifies CMS of the beneficiary's updated preference) or by calling 1-800-MEDICARE directly. We then include the beneficiary's claims data in the claims file provided to the ACO the following month.
In the November 2011 final rule (76 FR 67849), we acknowledged that it is possible that a beneficiary may decline to have his or her claims data shared with an ACO but would choose to continue to receive care from ACO participants and ACO providers/suppliers. In such a case, the ACO would still be responsible for that beneficiary's care, and, as such, although the beneficiary's claims data would not be shared with the ACO, CMS would continue to use the beneficiary's claims data in its assessment of the ACO's quality and financial performance.
In the November 2011 final rule (76 FR 67849 through 67850) we expressed our view that beneficiaries should be notified of their health care provider's participation in an ACO in order to have some control over who has access to their health information for purposes of the Shared Savings Program. Further, we indicated that the requirement that an ACO provider/supplier engage patients in a discussion about the inherent benefits, as well as the potential risks, of claims data sharing provided an opportunity for true patient-centered care and would create incentives for ACOs, ACO participants, and ACO providers/suppliers to develop Start Printed Page 72788positive relationships with each beneficiary under their care. Additionally, we stated that this policy would provide ACO participants and ACO providers/suppliers the opportunity to engage with beneficiaries by explaining the Shared Savings Program and its potential benefits for both the beneficiaries and the health care system as a whole.
Since implementation of the Shared Savings Program, we have shared claims data on over 5 million beneficiaries with over 300 Shared Savings Program ACOs. We have received informal feedback from ACOs that are putting the opt-out requirement into practice, and from beneficiaries who have received notifications from an ACO that wanted to request access to their claims data. We have learned the following from this feedback:
- The option for ACOs to mail notifications and then conduct in-office follow-up adds to ACOs' financial costs and delays their ability to access claims data in a timely manner. ACOs must wait until January 1 of the first performance year to send out mailings. After waiting the requisite 30 days, the earliest the ACO may submit beneficiary preferences to CMS is in February. The first set of claims data is then available in mid-March. In addition, some ACOs struggle with obtaining current mailing information for preliminarily prospectively assigned beneficiaries, which can delay the mailing of notifications to later in the performance year. Thus, the earliest opportunity for ACOs to receive claims data is mid-February, and that is only the claims data for beneficiaries who visited primary care providers in early January and were given the opportunity to decline claims data sharing at the point of care.
- Stakeholders, including ACOs, ACO participants, and ACO providers/suppliers, continually confuse the notification regarding the ACO's intent to request access to claims data with the separate requirement that all FFS beneficiaries must be notified of ACO participants' and ACO providers/suppliers' participation in the program. Beneficiaries must be notified at the point of care of the ACO participants' and ACO providers/suppliers' participation in an ACO, regardless of whether the ACO has or intends to request access to claims data.
- ACOs have commented that beneficiaries are confused about why their providers do not already have access to information regarding other care they may receive, which potentially erodes rather than strengthens the patient-provider relationship. Beneficiaries often assume their providers have all the information they need to care for them. However, as noted previously, the ACO, its ACO participants, and ACO providers/suppliers would not have claims data for services rendered outside the ACO, and would not necessarily have knowledge about that care.
- Beneficiaries can choose to receive care from providers outside an ACO, so beneficiaries may receive notices regarding data sharing from more than one ACO. This is most likely to occur in markets with high ACO penetration where a beneficiary may receive primary care services from several different ACO professionals, each participating in different ACOs. Beneficiaries report confusion, concern, and annoyance over receiving multiple mailings from ACOs, and question why their health care providers do not already have the information they need to appropriately coordinate their care.
- Beneficiaries receiving the notifications giving them the opportunity to decline claims data sharing may mistakenly believe they are being asked to “opt-out” of ACO care and/or Medicare FFS, or that they have been placed in a managed care plan without their consent.
- Beneficiaries that receive the letters in the mail notifying them of their provider's participation in an ACO and offering them the opportunity to decline claims data sharing often mistakenly believe that these letters are fraudulent and do not know what to do. Many ACOs are entities that have been newly formed by providers and suppliers for purposes of participating in the Shared Savings Program. While the beneficiary may have a strong relationship with his or her primary care provider, the beneficiary may not recognize the name of the newly formed ACO and therefore may have concerns and question the legitimacy of the notification.
- Our data indicate that approximately 2 percent of beneficiaries have declined claims data sharing. This is consistent with other CMS initiatives that have included data sharing, such as the Medicare Health Support demonstration, the Multi-Payer Advanced Primary Care Practice demonstration, the Physician Group Practice demonstration, and the Physician Group Practice Transition demonstration.
As discussed previously, beneficiaries currently have the opportunity to decline claims data sharing by responding to the letters that ACOs send to their preliminarily prospectively assigned beneficiaries, by informing an ACO provider/supplier during a face-to-face primary care service visit, or by contacting 1-800-MEDICARE directly. We continue to be committed to offering beneficiaries some control over ACO access to their beneficiary identifiable information for purposes of the Shared Savings Program. However, in light of the feedback we have received, we were motivated to review our claims data sharing policies and processes to determine what refinements could be made to mitigate the concerns raised by stakeholders regarding the burden imposed on both beneficiaries and those entities participating in the Shared Savings Program. We considered several aspects of our claims data sharing policies, including the use of various formats to communicate with beneficiaries regarding claims data sharing under the program such as: Mailed notifications to the list of preliminarily prospectively assigned beneficiaries by the ACO; face-to-face discussions with healthcare providers during primary care visits; and CMS's use of 1-800-MEDICARE and the Medicare & You Handbook. As discussed in the April 2011 proposed rule (76 FR 19558) and the November 2011 final rule (76 FR 67846), we are convinced by stakeholders that Medicare claims data provide an important supplement to the data to which the ACO and its ACO participants and ACO providers/suppliers already have access. Current law allows CMS to share certain beneficiary identifiable claims data with ACOs when those data are necessary for purposes of certain health care operations. HIPAA does not require that beneficiaries be presented with an opportunity to decline claims data sharing before their PHI can be shared. Moreover, several other CMS initiatives, including the Medicare Health Support demonstration, the Multi-Payer Advanced Primary Care Practice demonstration, the Physician Group Practice demonstration, and the Physician Group Practice Transition demonstration, have successfully shared claims data with providers in the absence of an opportunity for beneficiaries to decline claims data sharing. Therefore, we considered how to retain meaningful beneficiary choice in claims data sharing while reducing the confusion and burden caused by our current claims data sharing policies. We believe meaningful beneficiary choice in claims data sharing is maintained when the purpose and rationale for such claims data sharing are transparent and communicated to beneficiaries, and there is a mechanism in place for beneficiaries to decline claims data Start Printed Page 72789sharing. Thus, in revisiting our claims data sharing policies, we sought to maintain claims data sharing transparency and a mechanism for beneficiaries to decline claims data sharing.
b. Proposed Revisions
Based on our experiences with data sharing under the Shared Savings Program to date, we are proposing to modify our processes and policy for claims data sharing while remaining committed to retaining meaningful beneficiary choice over claims data sharing with ACOs. First, we propose to provide beneficiaries with the opportunity to decline claims data sharing directly through 1-800-MEDICARE, rather than through the ACO. We note that 1-800-MEDICARE has the capability for beneficiaries to use accessible alternative or appropriate assistive technology, if needed. We would continue to maintain a list of beneficiaries that have declined data sharing and ensure that their claims information is not included in the claims files shared with ACOs. Second, we propose to provide advance notification to all FFS beneficiaries about the opportunity to decline claims data sharing with ACOs participating in the Shared Savings Program through CMS materials such as the Medicare & You Handbook. The Handbook would include information about the purpose of the program, describe the opportunity for ACOs to request beneficiary identifiable claims data for health care operations purposes, and provide instructions on how beneficiaries may decline claims data sharing by contacting CMS directly through 1-800-MEDICARE. The Handbook would also contain instructions on how a beneficiary may reverse his or her preference to decline claims data sharing by contacting 1-800-MEDICARE. Third, to reduce burden for both beneficiaries and ACOs, we propose to remove the option for ACOs to mail notifications to beneficiaries and for beneficiaries to sign and return the forms to the ACO in order to decline claims data sharing. This process would be replaced by a simpler, direct process through notification at the point of care and through 1-800-MEDICARE as described previously.
We also propose to continue to require that ACO participants notify beneficiaries in writing at the point of care that their providers and suppliers are participating in the Shared Savings Program as required under § 425.312(a). We propose that ACO participants would continue to be required to post signs in their facilities using required template language. Rather than requiring ACO participants furnishing primary care services to provide a written form regarding claims data sharing to all beneficiaries who have a primary care service office visit, we propose to update the required notification template language for these signs to include information regarding claims data sharing. We would update the template language with the assistance of the Medicare Ombudsman's Office and beneficiary input to inform beneficiaries about both the Shared Savings Program and also that the ACO may request access to beneficiary identifiable claims data from CMS in order to perform health care operations as defined under the first and second paragraphs of the definition of health care operations at 45 CFR 164.501. The signs would also provide beneficiaries with information about their opportunity to decline this data sharing and instructions to call 1-800-MEDICARE if they would prefer that we not share their claims data with an ACO and its ACO participants and ACO providers/suppliers. The signs would likewise include instructions for how beneficiaries may reverse their opt-outs through 1-800-MEDICARE, if they determine in the future they would prefer to have their claims data made available to ACOs and their ACO participants and ACO providers/suppliers. Because ACO participants are required to post these signs in their facilities at all times, this written notification through the signs would occur at each visit, including the first visit the beneficiary has with an ACO participant during a performance year.
We also anticipate that some beneficiaries may continue to want to have the ability to take the information home or into their visit with their primary care provider for further discussion. Therefore, in addition to the signs, we propose to retain our policy that ACO participants that submit claims for primary care services used to determine the ACO's assigned beneficiary population be required to make a separate written notification form available to the beneficiary upon request.
We propose to modify § 425.312 and § 425.708 for clarity and to reflect these revised notification policies.
Finally, under Tracks 1 and 2, we propose to make beneficiary identifiable claims data available in accordance with applicable law on a monthly basis for beneficiaries that are either preliminarily prospectively assigned to the ACO or who have received a primary care service during the past 12-month period from an ACO participant upon whom assignment is based. Because Tracks 1 and 2 use a preliminary prospective assignment methodology with retrospective reconciliation, we believe that ACOs, ACO participants, and ACO providers/suppliers in Tracks 1 and 2 would benefit from access to beneficiary identifiable claims information for all FFS beneficiaries that may be assigned to the ACO at the end of the performance year. In contrast, under Track 3, we propose to make beneficiary identifiable claims data available only for beneficiaries that are prospectively assigned to an ACO, because the beneficiaries on the prospective assignment list are the only beneficiaries for whom the ACO would be held accountable at the end of the performance year. Consistent with the existing requirements at § 425.704, in order to request beneficiary identifiable claims data, and regardless of track, an ACO must: (1) Certify that it is a covered entity or the business associate of a covered entity that has provided a primary care service to the beneficiary in the previous 12 months (2) enter into a DUA with CMS prior to the receipt of these beneficiary identifiable data; (3) submit a formal request to receive beneficiary identifiable claims data for such beneficiaries at the time of application to the Shared Savings Program; and (4) certify that the request reflects the minimum data necessary for the ACO to conduct either its own health care operations work that falls within the first or second paragraph of the definition of health care operations at 45 CFR 164.501 or health care operations work on behalf of its ACO participants and ACO providers/suppliers that are covered entities (as the business associate of these covered entities) that falls within the first or second paragraph of the definition of health care operations at 45 CFR 164.501.
We believe these proposed modifications to our data sharing rules would significantly improve the claims data sharing process. First, we believe the modified process would reduce burden for beneficiaries who would no longer have to mail back forms. In addition, it would minimize beneficiary confusion in situations where an ACO may be newly formed and may not yet have established a relationship with the beneficiary. Instead, the beneficiary would be able decline claims data sharing, and reverse a decision to decline claims sharing, by contacting CMS directly using 1-800-MEDICARE. We believe beneficiaries would be more comfortable expressing their claims data Start Printed Page 72790sharing preferences directly through CMS, an agency with which beneficiaries have an existing relationship. Moreover, we believe our proposals would streamline ACO operations and would allow ACOs to access beneficiary identifiable claims data earlier in the performance year than is possible under our current policies. Beneficiary identifiable claims data would still be available on a monthly basis, but the new process would be operationally more efficient and less expensive for ACOs. By removing the 30-day delay before ACOs may request beneficiary identifiable claims data for their preliminarily prospectively assigned beneficiaries under Tracks 1 and 2 and prospectively assigned beneficiaries under Track 3, and reducing operational complexities associated with providing these data, ACOs would have access to beneficiary identifiable claims data in a more timely fashion. This may allow ACOs to intervene in the care of beneficiaries earlier during the performance year. In addition, as discussed previously, while we initially believed that requiring ACOs to notify beneficiaries of the opportunity to decline claims data sharing would improve engagement between ACO providers/suppliers that furnish primary care services and their patients, we now realize that this policy unintentionally created burden and confusion for both ACOs and beneficiaries, as many beneficiaries assume that their health care providers already have the information needed to optimally coordinate their care, even though this is not always the case. We believe that the proposed revisions to our claims data sharing policy would reduce beneficiary confusion about the Shared Savings Program and the role an ACO plays in assisting the beneficiary's health care providers to improve their health and health care experience, while still retaining a beneficiary's meaningful opportunity to decline claims data sharing.
We note that, since implementation of the program, a small percentage of FFS beneficiaries have requested that their identifiable claims data not be shared and have done so either by notifying the ACO or by contacting 1-800-MEDICARE to decline claims data sharing. None of our proposed revisions would have any effect on any existing beneficiary preferences. Previously recorded beneficiary preferences would continue to be honored, unless and until a beneficiary changes his or her preference by contacting 1-800-MEDICARE. Accordingly, our proposal not only preserves the beneficiary's ability to decline claims data sharing by directly contacting CMS, but also has no effect on existing beneficiary claims data sharing preferences, unless the beneficiary subsequently amends his or her preferences to allow claims data sharing.
In summary, we propose to amend § 425.704 to reflect our proposal to begin sharing beneficiary identifiable claims data with ACOs participating under Tracks 1 and 2 that request claims data on beneficiaries that are included on their preliminary prospective assigned beneficiary list or that have received a primary care service from an ACO participant upon whom assignment is based during the most recent 12-month period, at the start of the ACO's agreement period, provided all other requirements for claims data sharing under the Shared Savings Program and HIPAA regulations are met. We also propose to share beneficiary identifiable claims data with ACOs participating under Track 3 that request beneficiary identifiable claims data on beneficiaries that are included on their prospectively assigned beneficiary list. We also propose to revise § 425.312(a) and § 425.708 to reflect our policy that ACO participants use CMS approved template language to notify beneficiaries regarding participation in an ACO and the opportunity to decline claims data sharing. In addition, we propose to modify § 425.708 to reflect the streamlined process by which beneficiaries may decline claims data sharing. We also propose to add a new paragraph (c) to § 425.708 to reflect our proposal to honor any beneficiary request to decline claims data sharing that is received under § 425.708 until such time as the beneficiary may reverse his or her claims data sharing preference to allow data sharing.
We note that the beneficiary identifiable information that is made available under § 425.704 would include Parts A, B and D data, but would exclude any information related to the diagnosis and treatment of alcohol or substance abuse. As we discussed in the April 2011 proposed rule (76 FR 19557), 42 U.S.C. 290dd-2 and the implementing regulations at 42 CFR part 2 restrict the disclosure of patient records by federally conducted or assisted substance abuse programs. Such data may be disclosed only with the prior written consent of the patient, or as otherwise provided in the statute and regulations. We note that we may revisit this approach as technology in the area of consent management advances.
We seek comment on these proposals. We also seek comment on other specific modifications that could be made to our existing policies on data sharing to improve the ability of ACOs to access beneficiary identifiable claims data, and to reduce burden and confusion for ACOs, ACO participants, ACO providers/suppliers, and beneficiaries.
E. Assignment of Medicare FFS Beneficiaries
1. Background
Section 1899(c) of the Act requires the Secretary to “determine an appropriate method to assign Medicare fee-for-service beneficiaries to an ACO based on their utilization of primary care services provided under this title by an ACO professional described in paragraph (h)(1)(A).” Section 1899(h)(1)(A) of the Act constitutes one element of the definition of the term “ACO professional.” Specifically, this provision establishes that “a physician (as defined in section 1861(r)(1) of the Act)” is an “ACO professional” for purposes of the Shared Savings Program. Section 1861(r)(1) of the Act in turn defines the term physician as “. . . a doctor of medicine or osteopathy legally authorized to practice medicine and surgery by the State in which he performs such function or action . . .” In addition, section 1899(h)(1)(B) of the Act defines “ACO professional” to include practitioners described in section 1842(b)(18)(C)(i) of the Act, such as physician assistants (PAs) and nurse practitioners (NPs).
As we explained in the November 2011 final rule (76 FR 67851) the term “assignment” refers only to an operational process by which Medicare determines whether a beneficiary has chosen to receive a sufficient level of the requisite primary care services from physicians associated with a specific ACO so that the ACO may be appropriately designated as exercising basic responsibility for that beneficiary's care. Consistent with section 1899(b)(2)(A) of the Act, an ACO is held accountable “for the quality, cost, and overall care of the Medicare fee-for service beneficiaries assigned to it.” The ACO may also qualify to receive a share of any savings that are realized in the care of these assigned beneficiaries due to appropriate efficiencies and quality improvements that the ACO may be able to achieve. The term “assignment” for purposes of the Shared Savings Program in no way implies any limits, restrictions, or diminishment of the rights of Medicare FFS beneficiaries to exercise freedom of choice in the physicians and other health care Start Printed Page 72791providers and suppliers from whom they receive their services.
In developing the process for assigning Medicare beneficiaries to ACOs, we considered several other elements in addition to the definition of an ACO professional (76 FR 67851): (1) The operational definition of an ACO (see the discussion of the formal and operational definitions of an ACO in section II.B. of this proposed rule) so that ACOs can be efficiently identified, distinguished, and associated with the beneficiaries for whom they are providing services; (2) the definition of primary care services for purposes of determining the appropriate assignment of beneficiaries; (3) whether to assign beneficiaries to ACOs prospectively, at the beginning of a performance year on the basis of services rendered prior to the performance year, or retrospectively, on the basis of services actually rendered by the ACO during the performance year; and (4) the proportion of primary care services that is necessary for a beneficiary to receive from an ACO in order to be assigned to that ACO for purposes of this program.
In the November 2011 final rule (76 FR 67851 through 67870), we finalized the methodology that we currently use to assign beneficiaries to ACOs for purposes of the Shared Savings Program. Beneficiaries are assigned to a participating ACO using the assignment methodology in Part 425, subpart E of our regulations. In addition, since the final rule was issued, we have provided additional guidance and more detailed specifications regarding the beneficiary assignment process in operational instructions which are available to the public on the CMS Web site. (http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Financial-and-Assignment-Specifications.html)
In this section of this proposed rule, we summarize several key policies and methodological issues to provide background for several revisions to the assignment methodology that we are proposing based on our initial experiences with the program and questions from stakeholders.
2. Basic Criteria for a Beneficiary To Be Assigned to an ACO
In order to develop operational procedures needed to implement the Shared Savings Program, and to respond to inquiries from ACOs and other stakeholders, we developed specific criteria to govern beneficiary eligibility for assignment to an ACO which we propose to codify in a new provision at § 425.401. We believe that revising the regulations to include these eligibility criteria would help promote understanding of the assignment methodology. The proposed criteria in new § 425.401 are consistent with the current assignment methodology under § 425.400 and § 425.402 as well as the discussion of the assignment methodology in the preamble to the November 2011 final rule and operational instructions that we have issued since the publication of the final rule (76 FR 67851).
First, to determine whether a beneficiary is eligible to be assigned to an ACO, we must have information about the beneficiary's Medicare enrollment status. As required by section 1899(h)(3) of the Act, and consistent with the definition of Medicare FFS beneficiary in § 425.20, only beneficiaries enrolled in traditional Medicare FFS under Parts A and B are eligible to be assigned to an ACO participating in the Shared Savings Program. Because of this statutory definition and because an important objective of this program is to help align incentives between Part A and Part B, beneficiaries who have coverage under only one of these parts are not eligible to be assigned to an ACO. Beneficiaries enrolled in a group health plan—including beneficiaries enrolled in Medicare Advantage (MA) plans under Part C, eligible organizations under section 1876 of the Act, and Programs of All Inclusive Care for the Elderly (PACE) under section 1894 of the Act—are also not eligible to be assigned. However, we note that Medicare Secondary Payer (MSP) status does not exclude a beneficiary from assignment to an ACO.
The statute includes a provision that precludes duplication in participation in initiatives involving shared savings. Section 1899(b)(4) of the Act states that providers of services or suppliers that participate in certain programs that involve shared savings are not eligible to participate in the Shared Savings Program. In the November 2011 final rule (76 FR 67830 through 67833), we finalized a proposal to implement this requirement and to adopt a process for ensuring that providers and suppliers participating in the Shared Savings Program do not concurrently participate in another Medicare program or demonstration involving shared savings at § 425.114. Specifically, applications for participation in the Shared Savings Program are reviewed to assess for overlapping ACO participant TINs. ACO participants that are already participating in another Medicare program, model or demonstration involving shared savings are prohibited from participating in the Medicare Shared Savings Program. An ACO application that contains ACO participants that are already participating in another Medicare program or demonstration involving shared savings is rejected.
The statutory prohibition against providers and suppliers participating in multiple programs and initiatives that involve shared savings limits but does not prevent the possibility for a beneficiary to be assigned to more than one shared savings initiative. However, we believe it is important that beneficiaries are not assigned to more than one initiative involving shared savings because we do not believe it is appropriate to make multiple shared savings payments for the same beneficiaries. Therefore, at § 425.114(c), we provide that if the other program or demonstration involving shared savings does not assign beneficiaries based upon the TINs of the health care providers from whom they receive care, but uses an alternate beneficiary assignment methodology, we will work with the developers of the respective demonstrations and initiatives to devise an appropriate method to ensure no duplication in shared savings payments. For example, beneficiaries cannot be assigned to a Shared Savings Program ACO for a performance year if they are associated with another Medicare shared savings initiative at the start of the Shared Savings Program ACO's performance year.
We have also implemented procedures to exclude beneficiaries whose residence is outside the United States, U.S. territories or possessions from assignment to an ACO. We make this determination based on the most recent available data in our beneficiary records regarding the beneficiary's residence at the end of the assignment window. We do not believe it is appropriate to expect ACOs to be responsible for coordinating the care provided to beneficiaries that reside outside the United States, as required under the Shared Savings Program, or to hold ACOs accountable for the care provided to beneficiaries that reside outside the United States because ACOs may have limited ability to interact with overseas providers and suppliers. In most situations, Medicare does not pay for health care or supplies furnished outside the United States. (Additional guidance about this policy is available at http://www.medicare.gov/Pubs/pdf/11037.pdf.) As a result, claims information regarding services received in other countries is not available to ACOs. United States (U.S.) residence includes the 50 states, the District of Columbia, Puerto Rico, the U.S. Virgin Start Printed Page 72792Islands, Guam, American Samoa, and the Northern Marianas. (See guidance at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/Shared-Savings-Losses-Assignment-Spec-v2.pdf.) We believe it is appropriate to amend the regulations governing the assignment process to incorporate these limitations. Thus, we propose to add a new provision at § 425.401(a) of the regulations to outline the criteria that a beneficiary must meet in order to be eligible to be assigned to an ACO. Specifically, a beneficiary would be eligible to be assigned to a participating ACO, for a performance year or benchmark year, if the beneficiary meets all of the following criteria during the assignment window (defined in section II.F. of this proposed rule as the 12-month period used for assignment):
- Has at least 1 month of Part A and Part B enrollment and does not have any months of Part A only or Part B only enrollment.
- Does not have any months of Medicare group (private) health plan enrollment.
- Is not assigned to any other Medicare shared savings initiative.
- Lives in the U.S. or U.S. territories and possessions as determined based on the most recent available data in our beneficiary records regarding the beneficiary's residence at the end of the assignment window.
If a beneficiary meets all of the criteria in § 425.401(a), then the beneficiary would be eligible to be assigned to an ACO in accordance with the two-step beneficiary assignment methodology in § 425.402 and § 425.404. We also propose to make a conforming change to § 425.400 to reflect the addition of this new provision.
We request comment on this proposal to amend the regulations to address specifically the criteria that would be used to determine whether a beneficiary is eligible to be assigned to an ACO.
3. Definition of Primary Care Services
a. Overview
Section 1899(c) of the Act requires the Secretary to assign beneficiaries to an ACO “based on their utilization of primary care services” provided by a physician. However, the statute does not specify which kinds of services may be considered “primary care services” for this purpose, nor the amount of those services that would be an appropriate basis for making assignments. In this section of this proposed rule, we summarize how we currently identify the appropriate primary care services on which we base assignment. In addition, we propose several revisions to our current policies for defining primary care services for this purpose, consistent with our statement in the November 2011 final rule (76 FR 67853), that we intended to monitor this issue and would consider making changes to the definition of primary care services to add or delete codes, if there is sufficient evidence that revisions are warranted.
We currently define “primary care services” for purposes of the Shared Savings Program in § 425.20 as the set of services identified by the following HCPCS/CPT codes: 99201 through 99215, 99304 through 99340, 99341 through 99350, the Welcome to Medicare visit (G0402), and the annual wellness visits (G0438 and G0439). In addition, as we will discuss later in this section, we have established a cross-walk for these codes to certain revenue center codes used by FQHCs (prior to January 1, 2011) and RHCs so that their services can be included in the beneficiary assignment process.
In the November 2011 final rule (76 FR 67853), we established the current list of codes that constitute primary care services for several reasons. First, we believed the listed codes represented a reasonable approximation of the kinds of services that are described by the statutory language which refers to assignment of “Medicare fee-for-service beneficiaries to an ACO based on their utilization of primary care services” furnished by physicians. Because the statute requires that assignment be based upon the utilization of primary care services furnished by physicians, only primary care services can be considered in the assignment process. In addition, we selected this list to be largely consistent with the definition of “primary care services” in section 5501 of the Affordable Care Act. That section establishes the Primary Care Incentive Payment Program (PCIP) to expand access to primary care services, and thus its definition of “primary care services” provides a compelling precedent for adopting a similar list of codes for purposes of the beneficiary assignment process under the Shared Savings Program. We slightly expanded the list of codes found in section 5501 of the Affordable Care Act to include the Welcome to Medicare visit (HCPCS code G0402) and the annual wellness visits (HCPCS codes G0438 and G0439) as primary care services for purposes of the Shared Savings Program. These codes clearly represent primary care services frequently received by Medicare beneficiaries, and in the absence of the special G codes the services provided during these visits would be described by one or more of the regular office visit codes that are included in the list under section 5501 of the Affordable Care Act.
Since the publication of the November 2011 final rule, we have received several suggestions from ACOs and others regarding specific codes that we would consider adding to the definition of primary care services so that they could be considered when assigning beneficiaries to ACOs. For example, commenters have noted that effective January 1, 2013, Medicare pays for two CPT codes (99495 and 99496) that are used to report physician or qualifying non-physician practitioner transitional care management (TCM) services for a patient following a patient's discharge to a community setting from an inpatient hospital or SNF or from outpatient observation status in a hospital or partial hospitalization. These codes were established to pay a patient's physician or practitioner to coordinate the patient's care in the 30 days following a hospital or skilled nursing facility (SNF) stay. We believe that providing separate payment for the work of community physicians and practitioners in treating a patient following discharge from a hospital or nursing facility would ensure better continuity of care for these patients and help reduce avoidable readmissions. We discussed this policy in the CY 2013 Physician Fee Schedule (PFS) final rule with comment period that appeared in the November 16, 2012 Federal Register (77 FR 68978 through 68994).
Further, in the CY 2014 PFS final rule with comment period that appeared in the December 10, 2013 Federal Register (78 FR 74414 through 74427), we indicated that for CY 2015, we planned to establish a separate payment for HCPCS code GXXX1 under the PFS for chronic care management (CCM) services furnished to patients with multiple (two or more) chronic conditions. Subsequently, in the CY 2015 PFS final rule with comment period that appeared in the November 13, 2014 Federal Register, we provided more details relating to the implementation of the new PFS policy, including coding, elements of service, and payment rates (79 FR 67715 through 67728). Chronic care management services generally include regular development and revision of a plan of care, communication with other treating health professionals, and medication management.
Accordingly, as part of our broader multiyear strategy to appropriately recognize and value primary care and care management services, effective January 1, 2015, we will make a separate Start Printed Page 72793payment for CCM services under the PFS. We believe that successful efforts to improve chronic care management for these patients could improve the quality of care while simultaneously decreasing costs, such as through reductions in hospitalizations, use of post-acute care services and emergency department visits.
We have also received a few suggestions from hospitalists and others that certain evaluation and management codes used for services furnished in SNFs and other nursing facility settings (CPT codes 99304 through 99318) should be excluded from the definition of primary care services. In some cases, hospitalists that perform evaluation and management services in SNFs requested this change so that their ACO participant TIN need not be exclusive to only one ACO based on the exclusivity policy established in the November 2011 final rule (76 FR 67810 through 67811). The requirement under § 425.306(b) that an ACO participant TIN be exclusive to a single ACO applies when the ACO participant TIN submits claims for primary care services that are considered in the assignment process. However, ACO participant TINs upon which beneficiary assignment is not dependent (that is, ACO participant TINs that do not submit claims for primary care services that are considered in the assignment process) are not required to be exclusive to a single ACO.
These requests from hospitalists and others were based on drawing a distinction between evaluation and management services performed in SNFs and those that are performed in other nursing facilities. Specifically, these commenters believe that evaluation and management services furnished in SNFs are more likely to be acute in nature and should not be considered primary care services. In contrast, the evaluation and management services performed in other nursing facilities, where patients tend to stay for longer periods, are arguably more likely to include primary care services. We have also received comments, however, from others who support the inclusion of these services in the definition of primary care for the Shared Savings Program. They suggest that including the codes for evaluation and management services furnished in SNFs in the assignment process could help provide important incentives for ACOs to manage and coordinate the care of these vulnerable patients because ACOs would be held accountable for these patients if they receive the plurality of their primary care services from ACO professionals during a performance year.
In the November 2011 final rule, we discussed comments both for and against including the codes for SNF visits in the definition of primary care services (76 FR 67852 through 67853). However, we ultimately concluded that it was appropriate to include these codes. We continue to believe that including the codes for SNF and other nursing facility visits in the list of codes that constitute primary care services for purposes of assignment to an ACO is appropriate for a number of reasons. As we stated in the November 2011 final rule (76 FR 67853), beneficiaries often stay for long periods of time in SNFs (Medicare covers up to 100 days of SNF services in each benefit period) and it is reasonable to conclude that these codes represent basic evaluation and management services that would ordinarily be provided in physician offices if the beneficiaries were not residing in nursing homes. If these services are performed by ACO professionals, we continue to believe that it is reasonable to hold the ACO accountable for the care of these beneficiaries. In addition, as we noted previously, the PCIP program established under section 5501 of the Affordable Care Act was established to expand access to “primary care services”. Under this program, beginning January 1, 2011 and continuing through December 31, 2015, we pay an incentive payment of 10 percent of Medicare program payments to qualifying primary care physicians and certain non-physician practitioners who furnish specified primary care services. We believe it is compelling that these SNF codes are included in the definition of “primary care services” in section 5501 of the Affordable Care Act, which established this incentive program. We would also note that CPT codes 99304 through 99318 do not differentiate between evaluation and management services performed in SNFs and other nursing facilities. Thus, services furnished in SNFs and other nursing facilities are included in the definition of “primary care services” for purposes of section 5501. Finally, in the CY 2015 PFS final rule with comment period (79 FR 67910 through 67911), we added the Skilled Nursing Facility 30-Day All-Cause Readmission Measure (SNFRM) to the quality performance measure set used to evaluate the quality of the care furnished by ACOs. We believe the addition of this measure helps to fill a gap in the current Shared Savings Program measure set and provides a focus on an area where ACOs are targeting redesign. Therefore, we continue to believe that it is reasonable to conclude that services provided in SNFs with CPT codes 99304 through 99318 represent basic evaluation and management services that would ordinarily be provided in physician offices if the beneficiaries were not residing in nursing homes and should continue to be included in the definition of primary care services used for purposes of beneficiary assignment to an ACO participating in the Shared Savings Program. Although we are not making a proposal at this time regarding CPT codes 99304 through 99318, we welcome comment from stakeholders on the implications of retaining these codes in the definition of primary care services.
b. Proposed Revisions
We believe that the TCM services represented by CPT codes 99495 and 99496 represent primary care services that should be considered in the beneficiary assignment methodology under the Shared Savings Program. In order to receive payment for these codes, the physician or non-physician practitioner is required to accept care of the beneficiary post-discharge from an inpatient hospital or SNF without a gap and must take responsibility for the beneficiary's overall care for a period of 30 days following the discharge. Likewise, we believe that the CCM services represented by HCPCS code GXXX1 are primary care services that should also be considered in the beneficiary assignment methodology under the Shared Savings Program. The CCM service includes continuity of care with a designated practitioner or member of the care team with whom the patient is able to get successive routine appointments. The CCM service also includes access to care management services 24-hours-a-day, 7-days-a-week, which means providing beneficiaries with a means to make timely contact with health care providers to address the patient's urgent chronic care needs regardless of the time-of-day or day of the week. Additional explanation of these and the other required elements for billing CCM services can be found in the CY 2015 PFS final rule with comment period (79 FR 67715 through 67728). Therefore, we propose to update the definition of primary care services at § 425.20 to include both TCM codes (CPT codes 99495 and 99496) and the CCM code (HCPCS code GXXX1) and to include these codes in our beneficiary assignment methodology under § 425.402.
Further, in order to promote flexibility for the Shared Savings Start Printed Page 72794Program and to allow the definition of primary care services used in the Shared Savings Program to respond more quickly to HCPCS/CPT coding changes made in the annual PFS rulemaking process, we propose to make any future revisions to the definition of primary care service codes through the annual PFS rulemaking process. If we intend to add any proposed new HCPCS/CPT or revenue center codes to the definition of primary care services for purposes of the Shared Savings Program, we would include a discussion of the proposed addition in the preamble to the PFS proposed rule to allow an opportunity for comment before we announce our final decision in the PFS final rule. Such an approach would enable the Shared Savings Program to be more flexible and responsive to incorporate any changes to primary care oriented codes that are made through the PFS rulemaking process. We believe this process for making changes to the Shared Savings Program's definition of primary care services under § 425.20 would help to ensure that the definition of primary care services used under the Shared Savings Program properly reflects the full range of primary care services that beneficiaries may receive under Medicare and that the assignment methodology accurately aligns beneficiaries with the entities that are responsible for managing their overall care. In addition, revising the definition of primary care services for purposes of the Shared Savings Program through the annual rulemaking for the PFS would enable us to efficiently update and revise primary care service codes used for purposes of beneficiary assignment under the Shared Savings Program to reflect any administrative HCPCS/CPT coding changes, such as changes to reflect successive coding changes. Accordingly, we also propose to amend the definition of primary care services at § 425.20 to include additional codes designated by CMS as primary care services for purposes of the Shared Savings Program, including new HCPCS/CPT codes or revenue codes and any subsequently modified or replacement codes.
We seek comments on these proposals. In addition, we seek comments as to whether there are any additional existing HCPCS/CPT codes that we should consider adding to the definition of primary care services in future rulemaking for purposes of assignment of beneficiaries to ACOs under the Shared Savings Program. It would be most helpful if such comments include a detailed discussion of the basis for such an addition.
4. Consideration of Physician Specialties and Non-Physician Practitioners in the Assignment Process
a. Overview
Primary care services can generally be defined based on the type of service provided, the type of provider specialty that provides the service, or both. In the November 2011 final rule establishing the Shared Savings Program (76 FR 67853 through 67856), we adopted a balanced assignment process that simultaneously maintains the requirement to focus on primary care services in beneficiary assignment, while recognizing the necessary and appropriate role of specialists in providing primary care services, such as in areas with primary care physician shortages.
Under § 425.402, after identifying all patients that had a primary care service with a physician who is an ACO professional (and who are thus eligible for assignment to the ACO under the statutory requirement to base assignment on “utilization of primary care services” furnished by physicians), we employ a step-wise approach as the basic assignment methodology. This step-wise assignment process takes into account two particular decisions that we described in the November 2011 final rule (76 FR 67853 through 67858): (1) Our decision to base assignment on the primary care services of specialist physicians in the second step of the assignment process; and (2) our decision also to take into account the plurality of all primary care services provided by ACO professionals, including both primary care and specialist physicians and certain non-physician practitioners, in determining which ACO is truly responsible for a beneficiary's primary care in the second step of the assignment process. Our current step-wise assignment process thus occurs in the following two steps:
Step 1: In this step, the beneficiary would be assigned to the ACO if the allowed charges for primary care services furnished to the beneficiary by primary care physicians who are ACO professionals are greater than the allowed charges for primary care services furnished by primary care physicians who are ACO professionals in any other ACOs, and greater than the allowed charges for primary care services billed to Medicare by any other solo practice/group containing primary care physicians, identified by a Medicare-enrolled TIN, that is unaffiliated with any ACO. In other words, first we add up the allowed charges for primary care services billed by primary care physicians through the TINs of ACO participants in the ACO. Next, we add up the allowed charges for primary care services furnished by primary care physicians that are billed through other Medicare-enrolled TINs (or through a collection of ACO participant TINs in the case of another ACO). If the allowed charges for the services furnished by ACO participants are greater than the allowed charges for services furnished by the participants in any other ACO or by any non-ACO participating Medicare-enrolled TIN, then the beneficiary is assigned to the ACO in the first step of the assignment process.
Step 2: This step applies only for beneficiaries who have not received any primary care services from a primary care physician. We assign a beneficiary to an ACO in this step if the beneficiary received at least one primary care service from a physician participating in the ACO, and more primary care services (measured by Medicare allowed charges) from ACO professionals (physician regardless of specialty, nurse practitioner, physician assistant or clinical nurse specialist) at the ACO than from ACO professionals in any other ACO or solo practice/group of practitioners identified by a Medicare-enrolled TIN or other unique identifier, as appropriate, that is unaffiliated with any ACO.
Since publication of the November 2011 final rule (76 FR 67853 through 67858), we have gained further experience with this assignment methodology. We have learned from its application for the first 220 ACOs participating in the program that, on average, about 92 percent of the beneficiaries assigned to ACOs are assigned in step 1, with only about 8 percent of the beneficiaries being assigned in step 2.
We have adopted a similar beneficiary assignment approach for some other programs, such as the PQRS Group Practice Reporting Option via the GPRO web interface (77 FR 69195 through 69196). We would note that in the CY 2015 PFS final rule with comment period that appeared in the November 13, 2014 Federal Register, we revised the Value Modifier (VM) beneficiary attribution methodology and the PQRS GPRO web interface beneficiary assignment methodology to make them slightly different from the Medicare Shared Savings Program assignment methodology, namely—(1) eliminating the primary care service pre-step that is statutorily required for the Shared Savings Program; and (2) including NPs, PAs, and CNSs in step 1 rather than in step 2 of the attribution process (see 79 FR 67790 and 79 FR 67962).Start Printed Page 72795
b. Proposed Revisions
We continue to believe that the current step-wise assignment methodology generally provides a balance between maintaining a strong emphasis on primary care while ultimately allowing for assignment of beneficiaries on the basis of how they actually receive their primary care services. However, we have received several suggestions for possible improvements to the assignment methodology for consideration.
Some stakeholders have suggested that primary care services by non-physician practitioners (NPs, PAs, and CNSs) should be included in step 1 of the assignment methodology rather than only in step 2 as they are under the current process. These stakeholders have indicated that non-physician practitioners very often serve as a beneficiary's sole primary care provider, based on beneficiary preferences or other factors, especially in rural areas and other areas where there is a shortage of primary care physicians. We considered this recommendation for a number of reasons.
As previously explained in the November 2011 final rule (76 FR 67853 through 67858), in establishing the Shared Savings Program, we adopted certain key features of the Shared Savings Program (for example, the decision not to include physician specialties in step 1 of the assignment methodology and the definition of primary care physician under § 425.20) to align with other Affordable Care Act provisions that place a strong emphasis on primary care. In particular, we referred to section 5501 of the Affordable Care Act which established the PCIP. For purposes of section 5501 of the Affordable Care Act, a “primary care practitioner” is defined as a physician who has a primary specialty designation of family medicine, internal medicine, geriatric medicine, or pediatric medicine or as a “nurse practitioner, clinical nurse specialist, or physician assistant.” Therefore, we believe it would be appropriate to better align the assignment methodology under the Shared Savings Program with the primary care emphasis in other provisions of the Affordable Care Act by including these non-physician practitioners in step 1 of the assignment process. Further, we believe that including these non-physician practitioners in step 1 would be supported by the statute as long as we continue under § 425.402 to first identify all patients that have received a primary care service from a physician who is an ACO professional and who are thus eligible for assignment to the ACO under the statutory requirement to base assignment on “utilization of primary care services” furnished by physicians. Finally, we believe that it would be appropriate to include primary services furnished by NPs, PAs, and CNSs in step 1 of the beneficiary assignment methodology (after satisfying the statutory criterion that assignment be based on primary care services by physicians). Under section 1899(b)(2)(D), the ACO is required to have sufficient primary care ACO professionals to care for the number of FFS beneficiaries assigned to the ACO. The statute includes NPs, PAs, and CNSs in its definition of ACO professional; thus recognizing the important role played by these non-physician practitioners in managing and coordinating the care of Medicare FFS beneficiaries.
We believe including these practitioners in step one of the assignment process could also further strengthen our current assignment process, which we designed to simultaneously maintain a primary care centric approach to beneficiary assignment, by including services furnished by physicians from all of the primary care specialties in step 1, while also recognizing the necessary and appropriate role of specialists in providing primary care services by including services furnished by specialist physicians in step 2. Including services furnished by NPs, PAs, and CNSs in determining the plurality of primary care services in step 1 of the assignment process may help ensure that beneficiaries are assigned to the ACO (or non-ACO entity) that is actually providing the plurality of primary care for that beneficiary and thus, should be responsible for managing the patient's overall care. In this way, all primary care services furnished by ACO professionals, including the entire primary care physician and practitioner team (including NPs, PAs, and CNSs working in clinical teams in collaboration with or under the supervision of physicians), would be considered for purposes of determining where a beneficiary received the plurality of primary care services under step 1 of the assignment methodology. Accordingly, we are proposing to amend the assignment methodology to include primary care services furnished by NPs, PAs, and CNSs in step 1 of the assignment process.
However, we would note that there could also be some concerns about adding NPs, PAs, and CNSs to step 1 of the assignment methodology. Unlike for physicians, the CMS self-reported specialty codes reported on claims for NPs, PAs, and CNSs are not further broken down by specific specialty areas and therefore do not allow practitioners to indicate whether they are typically functioning as primary care providers or as specialists. Therefore, we are concerned that by considering services furnished by NPs, PAs, and CNSs in step 1, we may ultimately assign some beneficiaries to an ACO inappropriately based on specialty care over true primary care. Thus, while we invite comments on our proposal to include primary care services furnished by NPs, PAs, and CNSs in step 1 of the assignment methodology, we also seek comment on the extent to which these non-physician practitioners provide non-primary care services and whether there are ways to distinguish between primary care services and non-primary care services billed by these non-physician practitioners.
Some other stakeholders have suggested that certain physician specialties are inappropriately included in the assignment process and therefore request that we exclude certain physician specialties from step 2 of the assignment process. These stakeholders are concerned that by being included in step 2 of the assignment process, the ACO participants that submit claims for services furnished by these specialists are inappropriately limited to participating in only one ACO because of the exclusivity requirement under § 425.306(b) of the regulations. This requirement is discussed in the November 2011 final rule (76 FR 67810 through 67811). Further, some stakeholders have indicated that they are confused by the current exclusivity requirement and inappropriately believe that an ACO participant can participate in more than one ACO as long as none of the beneficiaries for whom the ACO participant has submitted claims for primary care services have been assigned to the ACO.
We would like to emphasize that under § 425.306(b), the requirement that an ACO participant must be exclusive to a single ACO applies whenever primary care service claims submitted by the ACO participant are considered in the beneficiary assignment process. The application of the current exclusivity requirement to an ACO participant is not affected by whether or not a FFS beneficiary for whom an ACO participant has submitted claims for primary care services is ultimately assigned to the ACO. Rather, an ACO participant that submits claims to Medicare for primary care services must be exclusive to a single ACO because Start Printed Page 72796the claims for primary care services submitted by the ACO participant are used to determine beneficiary assignment to the ACO. Additionally, the current exclusivity requirement is not affected by whether or not the primary care services for which the ACO participant submits claims are services furnished by primary care physicians, specialist physicians, or NPs, PAs, and CNSs. Furthermore, this exclusivity requirement applies only to the ACO participant and not to individual practitioners. Individual practitioners are free to participate in multiple ACOs, provided they are billing under a different Medicare-enrolled TIN for each ACO in which they participate. (See 76 FR 67810 through 67811). For example, there may be practitioners who work in multiple settings and bill Medicare for primary care services through several different TINs, depending on the setting. If each of these TINs represents an ACO participant in a different ACO, then the practitioner would be an ACO professional in more than one ACO.
Some stakeholders have argued that certain specialties that bill for some of the evaluation and management services designated as primary care services under § 425.20 do not actually perform primary care services. This is because most of the CPT and other HCPCS codes that are included in the definition of primary care services under § 425.20 are actually more general purpose codes used for a wide variety of clinical practices that are not specific to primary care, such as CPT office visit codes. For example, cataract surgeons bill for some of the office visit codes included in the definition of “primary care” but in actual practice these surgeons do not perform primary care when they report these codes. These commenters believe that the wide spread use of these codes is the reason that for purposes of PCIP, the CPT code-based definition of “primary care services” is paired with the definition of “primary care practitioners” under that statute. In other words, to identify true primary care services, the CPT codes for primary care services must be billed by practitioners that render primary care services.
We agree that although some specialties such as surgeons and certain others bill Medicare for some of the Shared Savings Program “primary care” codes, in actual practice the services such specialists perform when reporting these codes do not typically represent primary care services because the definitions of HCPCS/CPT codes for office visits and most other evaluation and management services are not based on whether primary care is provided as part of the service. Accordingly, we agree that to identify primary care services more accurately, the CPT codes for primary care services should be paired with the specialties of the practitioners that render those services and that it would be appropriate to exclude services provided by certain physician specialties from the beneficiary assignment process.
Therefore, we are proposing to exclude services provided by certain CMS physician specialties from the beneficiary assignment process. The net effect of this proposal would be to exclude certain claims from determining the ACO's assigned population. The proposed lists of physician specialties that would be included in and excluded from the assignment process (provided in Tables 1 through 4 of this proposed rule) are based on recommendations by CMS medical officers knowledgeable about the services typically performed by physicians and non-physician practitioners. However, we note that given the many requests and comments from specialists and specialty societies asking to have their services included in the assignment methodology that we received during the original rulemaking to establish the Shared Savings Program, we attempted to limit the list of physician specialty types that would be excluded from the assignment process to those physician specialties that would very rarely, if ever, provide primary care to beneficiaries. As a general rule, for example, we expect that physicians with an internal medicine subspecialty such as nephrology, oncology, rheumatology, endocrinology, pulmonology, and cardiology would frequently be providing primary care to their patients. Especially for beneficiaries with certain chronic conditions (for example, certain heart conditions, cancer or diabetes) but who are otherwise healthy, we expect that these specialist physicians often take the role of primary care physicians in the overall treatment of the beneficiaries if there is no family practitioner or other primary care physician serving in that role. In contrast we expect that most surgeons, radiologists, and some other types of specialists would not typically provide a significant amount of primary care, if any, and therefore we propose to exclude their services from the assignment process.
More specifically, the following 4 tables display the specific CMS physician specialty codes that we are proposing to include and exclude for beneficiary assignment purposes under the Shared Savings Program.
- Table 1 shows the CMS physician specialty codes that would continue to be included in step 1.
- Table 2 lists the physician specialties that we are proposing would continue to be included in step 2.
- Table 3 lists the physician specialties that we are proposing to exclude from the beneficiary assignment methodology under step 2. Under this proposal, services furnished by these physician specialties would also be excluded for purposes of determining if a beneficiary has received a primary care service from a physician who is an ACO professional, which under § 425.402(a) is a precondition for assignment to an ACO.
- Table 4 shows the CMS specialty codes for NPs, PAs, and CNSs that under our proposal would be included in beneficiary assignment step 1.
Table 1—CMS Physician Specialty Codes That Would Continue To Be Included in Assignment Step 1
Code Specialty name 01 General Practice. 08 Family Practice. 11 Internal Medicine. 38 Geriatric Medicine. Start Printed Page 72797Table 2—CMS Physician Specialty Codes That Would Continue To Be Included in Assignment Step 2
Code Specialty name 03 Allergy/immunology. 06 Cardiology. 10 Gastroenterology. 13 Neurology. 16 Obstetrics/gynecology. 17 Hospice and palliative care. 23 Sports medicine. 25 Physical medicine and rehabilitation. 29 Pulmonary disease. 37 Pediatric medicine. 39 Nephrology. 44 Infectious disease. 46 Endocrinology. 66 Rheumatology. 70 Multispecialty clinic or group practice. 82 Hematology. 83 Hematology/oncology. 84 Preventive medicine. 90 Medical oncology. 98 Gynecology/oncology. Table 3—CMS Physician Specialty Codes That We Propose To Exclude From Assignment Step 2
Code Specialty name 02 General surgery. 04 Otolaryngology. 05 Anesthesiology. 07 Dermatology. 09 Interventional pain management. 12 Osteopathic manipulative therapy. 14 Neurosurgery. 18 Ophthalmology. 20 Orthopedic surgery. 21 Cardiac electrophysiology. 22 Pathology. 24 Plastic and reconstructive surgery. 26 Psychiatry. 27 Geriatric psychiatry. 28 Colorectal surgery. 30 Diagnostic radiology. 33 Thoracic surgery. 34 Urology. 36 Nuclear medicine. 40 Hand surgery. 72 Pain management. 76 Peripheral vascular disease. 77 Vascular surgery. 78 Cardiac surgery. 79 Addiction medicine. 81 Critical care (intensivists). 85 Maxillofacial surgery. 86 Neuro-psychiatry. 91 Surgical oncology. 92 Radiation oncology. 93 Emergency medicine. 94 Interventional radiology. 99 Unknown physician specialty. C0 Sleep medicine. Table 4—CMS Non-Physician Specialty Codes That Would Be Included in Assignment Step 1
Code Specialty name 50 Nurse practitioner. 89 Clinical nurse specialist. 97 Physician assistant. The primary benefit of this proposal is that it could help ensure that beneficiaries are correctly assigned to the ACO or other entity that is actually providing primary care and managing the patient's overall care. Otherwise, for example, a beneficiary could inadvertently be assigned to an ACO based on services furnished by a surgeon who had not provided primary care but had provided a number of consultations for a specific clinical condition. Another important benefit of this proposal is that the ACO participants that submit claims solely for services performed by the categories of specialists that we are proposing to exclude from the assignment process would have greater flexibility to participate in more than one ACO if the ACO participant does not submit claims for any primary care services performed by other physicians or non-physician practitioners that are included in the assignment process. This could especially be the case for small physician practices which only submit claims for specialty services. Allowing such ACO participants that are composed solely of excluded specialists to participate in more than one ACO would support our goal of facilitating competition among ACOs by increasing the number of specialists that can participate in more than one ACO. This proposal would not be expected to have a significant impact on the overall number of beneficiaries assigned to each ACO because we believe most of the specialties that we propose to exclude from the assignment methodology provide a relatively modest number of services under the codes included in the definition of primary care services or are not typically the only physician that a beneficiary sees. For example, patients that are furnished consultations by a thoracic surgeon would typically also concurrently receive care from a primary care physician, cardiologist or other medical specialist.
We propose to amend § 425.402 to reflect these proposed changes to the assignment methodology. Specifically, we propose to revise § 425.402(a) to include NPs, PAs, and CNSs as ACO professionals that would be considered in step 1 of the assignment process. In addition, we propose to amend § 425.402 by adding a new paragraph (b) to identify the physician specialty designations that would be considered in step 2 of the assignment process. We also propose to modify the exclusivity requirement at § 425.306(b) to clarify how the exclusivity rules would be affected by this proposal to exclude certain specialists from step 2 of the assignment methodology. Specifically, we propose to revise § 425.306(b) to indicate that each ACO participant that submits claims for primary care services used to determine the ACO's assigned population (that is, services rendered by the primary care physicians or ACO professionals listed in Tables 1, 2, and 4) must be exclusive to one Medicare Shared Savings Program ACO.
In addition, we propose to make several conforming and technical changes to § 425.402(a). First, we propose a modification to provide that for purposes of determining whether a beneficiary has received a primary care service from a physician who is an ACO professional, we would consider only services furnished by primary care physicians or physicians with a specialty listed in new paragraph (b). Second, we propose to make modifications to conform with changes in the definitions of “assignment”, “ACO professional”, and “ACO provider/supplier” in addition to our proposal to adopt a prospective assignment approach under proposed Track 3 in section II.F. of this proposed rule. We seek comment on these proposals.
Finally, as part of our process of reviewing both recommendations discussed previously, we considered another alternative approach to assignment. We considered whether it might be preferable, after excluding the specialties listed in Table 3 from step 2 of the assignment process, to further simplify beneficiary assignment by establishing an assignment process that involves only a single step. More specifically, we considered whether we should replace the current two step assignment methodology with a new one step assignment process in which the plurality of primary care services provided by the physicians listed in Tables 1 and 2, and the non-physician practitioners in Table 4, would all be considered in a single step. Arguably, this approach could at least partially address the comments we have received about the current assignment methodology and also help further simplify the assignment process.
However, while it has some attractive features, we also have some important concerns about this approach. For example, beneficiaries receiving concurrent care from both primary care physicians and specialists could inappropriately be assigned to an ACO or other entity that is not responsible for managing their overall care. To illustrate, under an assignment process with only one step, if a beneficiary has a long term, continuing relationship with a family practitioner who is an ACO professional but also requires specialty care for a chronic allergy condition from an allergist who is not participating in an ACO, then in any given performance year the beneficiary could be assigned to the ACO or not depending merely on the allowed charges for primary care services furnished by the family practitioner versus the allowed charges for services furnished by the allergist. Under our current two step assignment methodology, this beneficiary would be consistently and appropriately assigned to the ACO in which the beneficiary's family practitioner participates. We believe this result would be appropriate because, in this example, the family practitioner is responsible for managing the overall care of this patient whereas Start Printed Page 72798the allergist is providing more specialized care. A similar problem would exist for some other beneficiaries, such as those who temporarily require specialty care for an acute condition during a performance year. Therefore, we are concerned that by establishing an assignment methodology based on a single step, we may reduce our focus on primary care and ultimately assign some beneficiaries to an ACO inappropriately based on specialty care over true primary care. A one-step assignment methodology could also introduce additional instability into the assignment process. Therefore, we are not proposing to combine the two steps used under the current assignment methodology.
Although we are not proposing this change at this time, we seek comments as to whether it would be preferable, after excluding the physician specialties listed in Table 3 from the assignment process, to further simplify the assignment methodology by establishing an assignment process that involves only a single step. We will consider comments on this issue during the development of the final rule.
We also welcome any comments about the possible impact these potential changes to the assignment methodology might have on other CMS programs that use an assignment methodology that is generally aligned with the Shared Savings Program, such as PQRS GPRO reporting via the GPRO web interface and VM. We note that as previously discussed, we revised the assignment methodology for PQRS GPRO reporting via the GPRO web interface and VM in the CY 2015 PFS final rule with comment period that appeared in the November 13, 2014 Federal Register (79 FR 67790 and 79 FR 67962).
5. Assignment of Beneficiaries to ACOs That Include FQHCs, RHCs, CAHs, or ETA Hospitals
In this section, we summarize the regulatory policies in § 425.404 for assignment of beneficiaries to ACOs that include FQHCs and RHCs as ACO participants and subsequent operational procedures and instructions that we have established in order to allow FQHCs and RHCs as well as CAHs billing under section 1834(g)(2) of the Act (referred to as Method II), and ETA hospitals to fully participate in the Shared Savings Program. These types of providers may submit claims for physician and other professional services when certain requirements are met, but they do not submit their claims through the standard Part B claims payment system. Accordingly, we have established operational processes so that we can consider claims for professional services submitted by these providers in the process for assigning beneficiaries to ACOs. However, each of these four provider types (that is, FQHCs, RHCs, CAHs, ETA hospitals) generally have differing circumstances with respect to their provider and medical service code reporting requirements, claims forms used, and the payment methodology that applies to professional services. Although there are important differences between the payment policy and claims processing for FQHCs and RHCs, they do share some key characteristics. Therefore, we will discuss FQHCs and RHCs jointly, and then address CAHs and ETA hospitals separately.
a. Assignment of Beneficiaries to ACOs That Include FQHCs and RHCs
(1) Overview
FQHCs and RHCs are facilities that furnish services that are typically furnished in an outpatient clinic setting. They are currently paid an all-inclusive rate (AIR) per visit for qualified primary and preventive health services furnished to Medicare beneficiaries. On October 1, 2014, FQHCs began to transition to a new FQHC prospective payment system (PPS). FQHCs have been required to use HCPCS coding on all their claims since January 1, 2011, to inform the development of the PPS and for limited other purposes, and would be required to use HCPCS coding for payment purposes under the FQHC PPS. Under the current payment methodology, FQHCs and RHCs submit claims for each encounter with a beneficiary and receive an interim payment based on their AIR for qualifying visits. The claims contain revenue codes that distinguish general classes of services (for example, clinic visit, home visit or mental health service). Claims submitted by FQHCs and RHCs also identify the beneficiary to whom the service was provided, and include other information relevant to determining whether the AIR can be paid for the service. The claims contain very limited information regarding the individual practitioner, or the type of health professional (for example, physician, PA or NP) who provided the service.
Based on detailed comments from some FQHC and RHC representatives, in the November 2011 final rule, we established a beneficiary assignment process that allows primary care services furnished in FQHCs and RHCs to be considered in the assignment process for any ACO that includes an FQHC or RHC as an ACO participant. This process is codified in the regulations at § 425.404. (This assignment process also enables FQHCs and RHCs to form ACOs independently, without the participation of other types of eligible entities, provided they meet all other eligibility requirements (76 FR 67814)). Operationally we assign beneficiaries to ACOs that include FQHCs or RHCs in a manner generally consistent with how we assign beneficiaries to other ACOs based on primary care services performed by physicians as described previously. However, to address the requirement under section 1899(c) of the Act that beneficiaries be assigned to an ACO based on their use of primary care services furnished by physicians, we require ACOs that include FQHCs or RHCs to identify, through an attestation (see § 425.404(a)), the physicians that provide direct patient primary care services in their ACO participant FQHCs or RHCs. This additional step is not necessary in the case of other types of ACO participants that bill Medicare for primary care services because the claims clearly identify the practitioner furnishing the service. The attestation must be submitted to CMS as part of the application process for all ACOs that include FQHCs or RHCs as ACO participants and must include the NPIs and other identifying information for the physicians that directly provide primary care services in the ACO participant FQHCs or RHCs (see § 425.204(c)(5)(iii)(A)). Subsequently, we use the combination of the FQHC or RHC ACO participant TIN (and other unique identifier such as CCN, where appropriate) and the NPIs of the FQHC or RHC physicians provided to us through the attestation process to identify those beneficiaries that received a primary care service from a physician in the FQHC or RHC and who are therefore eligible to be assigned to the ACO as provided under § 425.402(a)(1). Then, we assign those beneficiaries to the ACO, using the step-wise assignment methodology under § 425.402(a)(3) and (4), if they received the plurality of their primary care services, as determined based on allowed charges for the HCPCS codes and revenue center codes included in the definition of primary care services at § 425.20, from ACO professionals.
We are able to crosswalk the revenue center codes reported by RHCs (and FQHCs for services performed prior to January 1, 2011) to comparable “primary care” HCPCS codes based on their code definitions. For example, CPT codes 99201 through 99215 (office/Start Printed Page 72799outpatient visits) are cross-walked to revenue center code 0521. Because the focus of FQHCs and RHCs is on primary care, we continue to believe these revenue center codes, when reported by FQHCs/RHCs, represent primary care services and not more specialized care. This crosswalk allows us to use the available revenue center codes as part of the beneficiary assignment process for RHC services (and for FQHC services furnished prior to January 1, 2011, when FQHCs were required to start submitting HCPCS codes) in place of the HCPCS codes which are used more generally. We established and have updated this crosswalk through contractor instructions. For claims submitted by FQHCs on or after January 1, 2011, we use the HCPCS codes which are included on the claims to identify the service provided.
To summarize, the special procedures that we have established in the November 2011 final rule and through operational program instructions (see program specifications on our Web site at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/Shared-Savings-Losses-Assignment-Spec-v2.pdf) for processing FQHC and RHC claims in order to allow these services to be considered in the beneficiary assignment process for the Shared Savings Program are as follows:
- FQHC and RHC services are billed on an institutional claim form and require special handling to incorporate them into the beneficiary assignment process. In general, ACO participants are identified through their TIN(s). However, the TINs for FQHCs and RHCs are not included in the CMS claims files. Therefore, we require that the CCNs also be reported for FQHCs and RHCs that are ACO participants. We use the CCN as the unique identifier for an individual FQHC or RHC. We require ACOs to include the CCN, the TIN, and the organizational NPI for FQHCs and RHCs that are participating in the ACO on their ACO participant lists. For example, the instructions for entities applying to the Shared Savings Program for 2015 were provided on our Web site at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/HowTo-Participant-List-Template.pdf.
- For FQHCs/RHCs that are ACO participants, we treat a FQHC or RHC service reported on an institutional claim as a primary care service performed by a primary care physician if the claim includes a HCPCS or revenue center code that is included in the definition of a primary care service at § 425.20 and the service was furnished by a physician that was identified as providing direct primary care services in the attestation submitted as part of the ACO's application. All such physicians are considered primary care physicians for purposes of the assignment methodology and no specialty code is required for these claims.
- A primary care physician is any physician NPI included in the attestation provided as part of the application submitted by an ACO that includes an FQHC or RHC as an ACO participant.
- For FQHCs/RHCs that are ACO participants, if the claim is for a primary care service furnished by someone other than a physician listed on the attestation, we treat the service as a primary care service furnished by a non-physician ACO professional. We established this operational policy in order to be able to include these FQHC/RHC primary care services in step 2 of the current beneficiary assignment methodology, as long as all other assignment requirements are met. We believe this is a reasonable assumption because FQHC/RHC covered services represented by the primary care HCPCS or revenue center codes would primarily represent services furnished by a non-physician ACO professional, if not by a primary care physician. We would note that covered services in RHCs or FQHCs include services furnished by certain other professionals who are not ACO professionals (that is, a certified nurse midwife, clinical psychologist, clinical social worker or, in very limited situations, a visiting nurse). However, such services are not reported under the HCPCS codes and revenue center codes that we have defined as being primary care services at § 425.20 for purposes of the Shared Savings Program. (See RHC/FQHC general billing requirements in the Medicare Claims Processing Manual, Chapter 9—Rural Health Clinics/Federally Qualified Health Centers, section 100 at http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c09.pdf).
- For FQHCs/RHCs that are not ACO participants, we treat a FQHC or RHC service reported on an institutional claim as a primary care service performed by a primary care physician if the claim includes a HCPCS or revenue center code that meets the definition of a primary care service at § 425.20. That is, for non-ACO participant FQHCs and RHCs, we assume a primary care physician performed all primary care services. As we explained previously in the November 2011 final rule (76 FR 67860), FQHC/RHC claims contain limited information as to the type of practitioner providing a service because such information is not necessary to determine payment rates for services in FQHCs/RHCs. Further, the attestation requirement at § 425.404(a) does not, of course, apply to FQHCs/RHCs that are not participating in an ACO. As a result, for non-ACO participant FQHCs/RHCs we are not able to determine whether a primary care service was furnished by a primary care physician, and thus should be considered in step 1, or was furnished by a specialist physician or NP/PA/CNS, and thus should be considered under step 2 of the assignment methodology. We chose to assume such primary care services were furnished by primary care physicians so that these services would be considered in step 1 of the assignment methodology. We established this operational procedure to help make sure we do not disrupt established relationships between beneficiaries and their care providers in non-ACO participant FQHCs and RHCs, by inappropriately assigning beneficiaries to ACOs that are not primarily responsible for coordinating their overall care.
To illustrate, we offer the following example: Assume Medicare is billed for five primary care services (all with equal allowable charges) for a particular beneficiary during a given performance year. One of those primary care services was provided by a primary care physician who is an ACO provider/supplier not affiliated with an FQHC. Four of the services were provided by an FQHC that is not an ACO participant. In this case, if we had assumed that the FQHC services were performed by NPs/PAs/CNSs, then the beneficiary would have been assigned to the ACO under step 1 of the assignment methodology and not the FQHC. Instead, by assuming the non-ACO participant FQHC services were performed by primary care physicians, this beneficiary would be assigned to the FQHC under step 1 and not to the ACO. In this scenario we believe it would be more appropriate for the beneficiary to be assigned to the FQHC since the FQHC is the entity that is primarily responsible for overseeing the care for this beneficiary. Also, we do not believe it would be appropriate to hold the ACO accountable for the beneficiary in this example given that the ACO is not providing the plurality of primary care.
(2) Proposed Revisions
As currently drafted, § 425.404(b) conflates the question of whether a service billed by an FQHC or RHC is Start Printed Page 72800provided by a physician with the question of whether the service is a primary care service. As a consequence, the provision arguably does not address situations where the FQHC/RHC claim is for a primary care service as defined under § 425.20, but the NPI reported on the claim is not the NPI of a physician included in the attestation submitted under § 425.404(a). As with other types of ACO participants, under the step-wise assignment methodology we believe it is appropriate to separately address the questions of whether the service is a primary care service, whether the service is a primary care service provided by an ACO professional who is a primary care physician, and whether the service is a primary care service provided by another ACO professional. Therefore, we propose to revise § 425.404(b) to better reflect the program rules and operational practices as previously outlined. In addition, we propose to revise § 425.404(b) to reflect the proposal discussed earlier to revise § 425.402(a)(1) to include services furnished by NPs, PAs, and CNSs as services that will be considered in step 1 of the assignment process. Under these proposals, we would assign beneficiaries to ACOs that include FQHCs and RHCs in the following manner.
To address the requirement under section 1899(c) of the Act that beneficiaries be assigned to an ACO based on their use of primary care services furnished by physicians, we would continue to require ACOs that include FQHCs and RHCs to identify, through an attestation (see § 425.404(a)), the physicians that provide direct patient primary care services in their ACO participant FQHCs or RHCs. Previously, we used this attestation information both for purposes of determining whether a beneficiary was “assignable” to an ACO and also for purposes of assigning beneficiaries to the ACO under step 1. However, we now propose to use this attestation information only for purposes of determining whether a beneficiary is assignable to an ACO. We refer to this determination under § 425.402(a)(1) as being the assignment “pre-step”. If a beneficiary is identified as an “assignable” beneficiary in the assignment pre-step, then we would use claims for primary care services furnished by all ACO professionals submitted by the FQHC or RHC to determine whether the beneficiary received a plurality of his or her primary care services from the ACO under Step 1. We propose to make revisions to § 425.404(b) to reflect these policies. To illustrate the assignment methodology for an ACO that includes FQHCs/RHCs we offer the following example. Assume Medicare is billed for five primary care services (all with equal allowable charges) for a particular beneficiary during a given performance year. One of those primary care services was provided by a specialist physician who is an ACO professional not affiliated with the FQHC. Two of the services were provided in an FQHC that is an ACO participant in the same ACO. Under the presumption discussed previously, these services are assumed to have been provided by NPs, PAs, or CNSs in the FQHC. The remaining two services were provided by specialist physicians billing under a common TIN but unaffiliated with the ACO. In this case, the beneficiary would be assignable to the ACO because the beneficiary had at least one primary care service with a physician who is an ACO professional. The beneficiary would be assigned to the ACO in Step 1 because two of the beneficiary's five primary care services during the performance year were provided by NPs, PAs, or CNSs who are ACO professionals in the ACO. These two services would be considered in step 1, consistent with the proposal to include NP, PA, and CNS primary care services in step 1 of the assignment methodology. In this hypothetical example, if we did not consider the FQHC claims for the services performed by NPs, PAs, or CNSs, the beneficiary would appear to have had only three valid claims to be used for assignment and would be assigned outside the ACO under Step 2 because there is only one claim for primary care services furnished by the specialist physician who is an ACO professional in the ACO but two of the claims were for services furnished by specialist physicians outside the ACO. However, by considering the FQHC claims, the beneficiary would have five claims for primary care services and would be assigned to the ACO under step 1 because two of the services were rendered by NPs, PAs, or CNSs who are ACO professionals, in contrast to the two claims for primary care services furnished by specialist physicians outside the ACO.
We have also encountered instances where an assignable beneficiary has received primary care services from FQHCs or RHCs that are not participants in an ACO. For non-ACO participant FQHCs and RHCs, we have previously assumed that all of their primary care services are performed by primary care physicians. We believe that this assumption, which we established in operational guidance as noted previously, has helped to assure that while beneficiaries are appropriately assigned to ACOs, we do not disrupt established relationships between beneficiaries and their care providers in FQHCs and RHCs that are not ACO participants. However, we note that this special assumption for non-ACO FQHCs/RHCs would no longer be necessary under the proposed revision to the assignment methodology at § 425.402 to consider primary care services furnished by NPs, PAs, and CNSs in step 1 of the assignment methodology rather than step 2 because: (1) As indicated earlier we believe that when a physician provides a service in an FQHC or RHC, the physician is functioning as a primary care physician, regardless of his or her specialty designation in the CMS enrollment records, and (2) there is no need to differentiate between primary care services performed by physicians and primary care services furnished by NPs, PAs, and CNSs for non-ACO FQHCs/RHCs because the requirement under section 1899(c) of the Act that beneficiaries be assigned to an ACO based on their use of primary care services furnished by physicians does not apply to entities that are not participating in an ACO. Instead, for all FQHCs/RHCs regardless of whether or not they are ACO participants, we would we treat all such claims for primary care services that are furnished by someone other than a physician listed on the attestation submitted by the ACO under § 425.404(a) as a service furnished by an NP, PA or CNS. Therefore, all primary care services furnished by non-ACO FQHCs/RHCs would be considered in step 1 of the assignment methodology, and there would no longer be a need to assume such primary care services were provided by primary care physicians in order to achieve this result.
We recognize the unique needs and challenges of rural communities and the importance of rural providers in assuring access to health care. FQHCs, RHCs and other rural providers play an important role in the nation's health care delivery system by serving as safety net providers of primary care and other health care services in rural and other underserved areas and for low-income beneficiaries. We have attempted to develop and implement regulatory and operational policies to facilitate full participation of rural providers in the Shared Savings Program, within the statutory requirements for the program. We welcome comments on our Start Printed Page 72801proposed revisions to § 425.404(b) and our current procedures for using claims submitted by FQHCs and RHCs in the assignment methodology and suggestions on how we might further support participation of FQHCs and RHCs in the Shared Savings Program in a manner that is consistent with the statutory requirements.
b. Assignment of Beneficiaries to ACOs That Include CAHs
We briefly addressed certain issues regarding ACOs that include CAHs in both the proposed rule (76 FR 19538 through 19539) and final rule (76 FR 67812 through 67814) establishing the Shared Savings Program. We indicated that we determined that current Medicare payment and billing policies could generally support the participation of CAHs in ACOs. However, we explained that the situation is somewhat complicated with regard to CAHs because section 1834(g) of the Act provides for two different payment methods for outpatient CAH services.
CAHs billing under section 1834(g)(1) of the Act (referred to as method I) can participate in the Shared Savings Program by establishing partnerships or joint venture arrangements with ACO professionals, just like other hospitals. CAHs billing under section 1834(g)(2) of the Act (referred to as method II) may form independent ACOs if they meet the eligibility requirements specified in the regulations. Professional services billed by method II CAHs are reported using HCPCS/CPT codes and are paid using a methodology based on the PFS. As a result, it is possible to use claims submitted by method II CAHs in the assignment methodology under § 425.402. However, method II CAH claims that include professional services require special processing because they are submitted as part of institutional claims. Therefore, we have developed operational procedures that allow these claims to be considered in the assignment process under § 425.402. Although we are not making any proposals at this time regarding the use of services billed by method II CAHs in the assignment process, we note that our procedures for incorporating claims billed by method II CAHs into the assignment methodology are available on our Web site at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/Shared-Savings-Losses-Assignment-Spec-v2.pdf (see section 3.3.) These technical specifications allow interested parties to understand how these claims are considered in the assignment methodology under § 425.402 and to compare the manner in which claims submitted by method II CAHs are processed with the processing of claims submitted by other providers that also require special processing before they can be considered in the assignment process. We believe this additional information in the technical specifications allows for a better understanding of the differences in our procedures, and the reasons for these differences.
One question we frequently receive from ACO applicants is about the identification numbers we use for different provider types. In general, ACO participants are identified by Medicare-enrolled TINs. However, the TINs for method II CAHs are not included in the CMS claims files. Therefore, in accordance with § 425.204(c)(5)(ii), we require that as part of their application, ACO applicants also include the CCNs for any CAHs that are included as ACO participants. In the assignment methodology under § 425.402, we use the CCN as the unique identifier for an individual method II CAH.
c. Assignment of Beneficiaries to ACOs That Include ETA Hospitals
After finalizing the beneficiary assignment rules established at § 425.400 through § 425.404 in the November 2011 final rule (76 FR 67851 through 76 FR 67870), we received inquiries regarding whether primary care services performed by physicians at ETA hospitals would be included in the assignment of beneficiaries to ACOs. ETA hospitals are hospitals that, under section 1861(b)(7) of the Act and § 415.160 of our regulations, have voluntarily elected to receive payment on a reasonable cost basis for the direct medical and surgical services of their physicians in lieu of Medicare PFS payments that might otherwise be made for these services. As a result of this election, we do not receive separate claims for such physician services furnished in ETA hospitals. However, ETA hospitals do bill separately for their outpatient hospital facility services, and these bills include the information needed to assign beneficiaries to an ACO. Therefore, we have developed operational instructions and processes (available at Section 3.5 of the specification document available on our Web site at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/Shared-Savings-Losses-Assignment-Spec-v2.pdf) that enable us to include primary care services performed by physicians at ETA hospitals in the assignment of beneficiaries to ACOs under § 425.402.
- We include TINs and other identifiers (including the hospital CCN) for ETA hospitals in the assignment algorithm in both steps 1 and 2 of the assignment process using claims from the outpatient (institutional) file.
- It is necessary for us to use institutional claims submitted by ETA hospitals in the assignment process because ETA hospitals are paid for physician professional services on a reasonable cost basis through their cost reports and no other claim is submitted for such services. However, ETA hospitals bill us for their separate facility services when physicians and other practitioners provide services in the ETA hospital and the institutional claims submitted by ETA hospitals include the HCPCS code for the services provided. We use the HCPCS code included on this institutional claim to identify whether a primary care service was rendered to a beneficiary in the same way as for any other claim.
- To determine the rendering physician for ETA institutional claims, we use the NPI listed in the “other provider” NPI field.
- Then we use PECOS to obtain the CMS specialty for the NPI listed on the ETA institutional claim.
- These institutional claims do not include allowed charges, which are necessary to determine where a beneficiary received the plurality of primary care services as part of the assignment process. Accordingly, we use the amount that would otherwise be payable under the PFS for the applicable HCPCS code, in the applicable geographic area as a proxy for the allowed charges for the service.
We believe it is appropriate to use ETA institutional claims for purposes of identifying primary care services furnished by physicians in ETA hospitals in order to allow these services to be included in the stepwise methodology for assigning beneficiaries to ACOs. We believe including these claims increases the accuracy of the assignment process by helping ensure that beneficiaries are assigned to the ACO or other entity that is actually managing the beneficiary's care. ETA hospitals are often located in underserved areas and serve as providers of primary care for the beneficiaries they serve. We believe it is appropriate that their patients benefit from the opportunity for ETA hospitals to fully participate in the Shared Savings Program. Therefore, we propose to revise § 425.402 by adding a new paragraph (c) to provide that when considering services furnished by Start Printed Page 72802physicians in ETA hospitals in the assignment methodology, we would use the amount payable under the PFS for the specified HCPCS code as a proxy for the amount of the allowed charges for the service. In addition, because we are able to consider claims submitted by ETA hospitals as part of the assignment process, we also propose to amend § 425.102(a) to add ETA hospitals to the list of ACO participants that are eligible to form an ACO that may apply to participate in the Shared Savings Program.
We invite comments on the use of institutional claims submitted by ETA hospitals for purposes of identifying primary care services furnished by physicians in order to allow these services to be considered in the assignment of beneficiaries to ACOs. We also invite comments on whether there are any other types of potential ACO participants that submit claims representing primary care services that CMS should also consider including in (or excluding from) its methodology for assigning beneficiaries to ACOs participating in the Shared Savings Program.
6. Effective Date for Finalization of Proposals Affecting Beneficiary Assignment
As indicated in section II.A. of this proposed rule, the effective date for the final rule would be 60 days after the final rule is published. However, we propose that any final policies that affect beneficiary assignment would be applicable starting at the beginning of the next performance year. We believe that implementing any revisions to the assignment methodology at the beginning of a performance year is reasonable and appropriate because it would permit time for us to make the necessary programming changes and would not disrupt the assessment of ACOs for the current performance year. Moreover, we propose to adjust all benchmarks at the start of the first performance year in which the new assignment rules are applied so that the benchmark for the ACO reflects the use of the same assignment rules as would apply in the performance year. For example, any new beneficiary assignment policies that might be included in a final rule issued in early 2015 would apply to beneficiary assignment starting at the beginning of the following performance year, which in this example would be January 1, 2016. In this hypothetical example, we would also adjust performance benchmarks that apply for the 2016 and subsequent performance years, as applicable, to reflect changes in our assignment methodology.
In addition, we would not retroactively apply any new beneficiary assignment policies to a previous performance year. For example, if the assignment methodology is applied beginning in 2016, we would not use it in mid-2016 to reconcile the 2015 performance year. In other words, the assignment methodology used at the start of a performance year would also be used to conduct the final reconciliation for that performance year.
F. Shared Savings and Losses
1. Background
Section 1899(d) of the Act establishes the general requirements for payments to participating ACOs. Specifically, section 1899(d)(1)(A) of the Act provides that ACO participants will continue to receive payment “under the original Medicare fee-for-service program under parts A and B in the same manner as they would otherwise be made,” and that an ACO is eligible to receive payment for shared Medicare savings provided that the ACO meets both the quality performance standards established by the Secretary, and demonstrates that it has achieved savings against a benchmark of expected average per capita Medicare FFS expenditures. Additionally, section 1899(i)(3) of the Act authorizes the Secretary to use other payment models in place of the one-sided model outlined in section 1899(d) of the Act as long as the Secretary determines these other payment models will improve the quality and efficiency of items and services furnished to Medicare beneficiaries without additional program expenditures.
In our November 2011 final rule (76 FR 67904 through 67909) establishing the Shared Savings Program, we considered a number of options for using this authority. For example, commenters suggested we consider such options as blended FFS payments, prospective payments, episode/case rate payments, bundled payments, patient centered medical homes or surgical homes payment models, payments based on global budgets, full or partial capitation, and enhanced FFS payments for care management. However, in the November 2011 final rule (76 FR 67905), we opted not to use our authority under section 1899(i) of the Act to integrate these kinds of alternative payment models at that time, noting that many of the suggested payment models were untested. We expressed concern that immediately adopting untested and/or unproven models with which we had little experience on a national scale could lead to unintended consequences for the FFS beneficiaries we serve or for the health care system more broadly. We also noted that the Affordable Care Act had established a new Center for Medicare and Medicaid Innovation (Innovation Center) at CMS. The Innovation Center is charged with developing, testing, and evaluating innovative payment and service delivery models in accordance with the requirements of section 1115A of the Act. Many of the approaches suggested by stakeholders and commenters on the Shared Savings Program rule are the subject of ongoing testing and evaluation by the Innovation Center. In the November 2011 final rule (76 FR 67905), we noted that while we did not yet have enough experience with novel payment models to be comfortable integrating them into the Shared Savings Program at the time, we anticipated that what we learned from these models might be incorporated into the program in the future.
In the November 2011 final rule establishing the Shared Savings Program (76 FR 67909), we created two tracks from which ACOs could choose to participate: A one-sided risk model (Track 1) that incorporates the statutory payment methodology under section 1899(d) of the Act and a two-sided model (Track 2) that is also based on the payment methodology under section 1899(d) of the Act, but incorporates performance-based risk using the authority under section 1899(i)(3) of the Act to use other payment models. Under the one-sided model, ACOs qualify to share in savings but are not responsible for losses. Under the two-sided model, ACOs qualify to share in savings with an increased sharing rate, but also must take on risk for sharing in losses.
In the November 2011 final rule (76 FR 67904), we discussed our belief that offering these two tracks would create an on ramp for the program to attract both providers and suppliers that are new to value-based purchasing as well as more experienced entities that are ready to share in losses. We expressed our belief that a one-sided model would have the potential to attract a large number of participants to the program and introduce value-based purchasing broadly to providers and suppliers, many of whom may never have participated in a value-based purchasing initiative before. Another reason we included the option for a one-sided track with no downside risk was our belief that this model would be accessible to and attract smaller group participation. Indeed, commenters persuaded us that ACOs new to the Start Printed Page 72803accountable care model—particularly small, rural, safety net, and physician-only ACOs—would benefit from spending time under a one-sided model before being required to accept performance-based risk (76 FR 67907).
We also noted, however, that while a one-sided model could provide incentives for participants to improve quality, it might not be sufficient incentive for participants to improve the efficiency and cost of health care delivery (76 FR 67904). Therefore, we used our authority under section 1899(i)(3) of the Act to create a performance-based risk option, Track 2, where ACOs would not only be eligible to share in savings, but also must share in losses. We believed a performance-based risk option would have the advantage of providing more experienced ACOs an opportunity to enter a sharing arrangement that provides greater reward for greater responsibility. Commenters supported our belief that models where ACOs bear a degree of financial risk hold the potential to induce more meaningful systematic change. This input from commenters underscored our own views regarding the importance of offering a pathway for ACOs to transition from the one-sided model to risk-based arrangements. These comments persuaded us that having Track 1 as a shared savings only option, while offering Track 2 as a shared savings/losses model, would be the most appropriate means to achieve our objectives. Thus, we made final these two tracks which offered the two-sided model under Track 2 to ACOs willing and able to take on performance-based risk in exchange for a greater share of any savings, and also a shared savings only model under Track 1 for the duration of an ACO's first 3-year agreement period for entities needing more experience before taking on risk. In the final rule, we required that ACOs that participate in Track 1 during their first agreement period must transition to Track 2 for all subsequent agreement periods. We noted our belief that offering the two tracks, but requiring a transition to Track 2 in subsequent agreement periods, would increase interest in the Shared Savings Program by providing a gentler “on ramp” while maintaining the flexibility for more advanced ACOs to take on greater performance-based risk in return for a greater share of savings immediately upon entering the program (76 FR 67907). Therefore, as specified in the November 2011 final rule (76 FR 67909), ACOs may enter the program in one of two tracks:
Track 1: Under Track 1, the ACO operates under the one-sided shared savings only model for its initial 3-year agreement period.
Track 2: Under Track 2, the ACO operates under the two-sided shared savings/losses model for the 3-year agreement period.
Although most of the program requirements that apply to ACOs in Track 1 and Track 2 are the same, the financial reconciliation methodology was designed so that ACOs that accept performance-based risk under Track 2 would have the opportunity to earn a greater share of savings. Thus, the same eligibility criteria, beneficiary assignment methodology, benchmark and update methodology, quality performance standards, data reporting requirements, data sharing provisions, monitoring for avoidance of at-risk beneficiaries, provider screening, and transparency requirements apply to ACOs under both models. However, the financial reconciliation methodology was modified for Track 2 in order to allow an opportunity for ACOs to earn a greater share of savings, in exchange for their willingness to accept performance-based risk. Specific differences between the two tracks include the minimum savings rate (MSR), the sharing rate based on quality performance, and the performance payment limit. Table 7 summarizes the differences between the existing one-sided and two-sided models.
In this section, we discuss various proposals for modifications to the program tracks and the financial model based on our experience to date, and propose to offer organizations an additional two-sided model (Track 3) as a further option for participation.
2. Modifications to the Existing Payment Tracks
a. Overview
Because we believe that payment models where ACOs bear a degree of financial risk have the potential to induce more meaningful systematic change in the behavior of providers and suppliers, it was our intent in the November 2011 final rule to establish the Shared Savings Program to encourage ACOs not only to enter the program, but also to progress to increased risk. Therefore, as discussed previously, we established a requirement that an ACO entering the program under Track 1 may only operate under the one-sided model for its first agreement period. For subsequent agreement periods, an ACO would not be permitted to operate under the one-sided model (§ 425.600(b)). If the ACO wishes to participate in the program for a second agreement period, it must do so under Track 2 (shared savings/losses). Additionally, an ACO experiencing a net loss during its initial agreement period may reapply to participate in the program, but the ACO must identify in its application the cause(s) for the net loss and specify what safeguards are in place to enable the ACO to potentially achieve savings in its next agreement period (§ 425.600(c)). In our view, this allowance for a full first agreement period under the one-sided model and required transition to performance-based risk in the subsequent agreement period struck a balance between our intent to encourage program participation by small, rural, or physician-only ACOs with the need to ensure that ACOs quickly transition to taking downside risk.
We are encouraged by the popularity of the Shared Savings Program, particularly the popularity of the one-sided model. Over 98 percent of ACOs participating in the Shared Savings Program (over 330 ACOs) have chosen Track 1, with only 5 ACOs participating under Track 2 as a starting option. About half of the ACOs participating in the program are small, provider-based, or rural ACOs, each having less than 10,000 assigned beneficiaries. We continue to believe that one 3-year agreement period under Track 1 is sufficient for many organizations to progress along the on-ramp to performance-based risk. We also continue to believe, as discussed in the November 2011 final rule (76 FR 67907), that payment models where ACOs bear a degree of financial risk have the potential to induce more meaningful systematic change in providers' and suppliers' behavior, so it remains our intent to continue to encourage forward movement up the ramp. However, based on our experience with the program, we recognize that many of the organizations that are currently participating in the program are risk averse and lack the infrastructure and readiness to manage increased performance-based risk. Given the short time period between finalization of the November 2011 final rule and the first application cycles, is it our impression that many ACOs, particularly smaller ACOs, focused initially on developing their operational capacities rather than on the implementation of care redesign processes. Therefore, we have some concerns about the slope of the on-ramp to performance-based risk created by the two existing tracks and the policy that requires ACOs in Track 1 (shared Start Printed Page 72804savings only) to transition to Track 2 (shared savings/losses) for their second agreement period. We are particularly concerned that the current transition from one- to two-sided risk may be too steep for some organizations, putting them into a situation where they must choose between taking on more risk than they can manage or dropping out of program participation altogether. For instance, we believe that some smaller and less experienced ACOs are likely to drop out of the program when faced with this choice, because the smaller an ACO's assigned beneficiary population, the greater the chances that shared losses could result from normal variation. Also, we are aware of the concern among some stakeholders that one agreement period under the one-sided model may be not be a sufficient amount of time for some ACOs to gain the level of experience with population management or program participation needed for them to be comfortable taking on performance-based risk. For some organizations, having additional experience in the Shared Savings Program under Track 1 could help them be in a better position to take on performance-based risk over time. We are also concerned that the existing features of Track 2 may not be sufficiently attractive to ACOs contemplating entering a risk-based arrangement. Finally, some ACOs have reported that establishing the repayment mechanism required to participate under the two-sided model is difficult and ties up capital that otherwise could be used to implement the care processes necessary to succeed in the program. We continue to believe the requirement that ACOs entering the two-sided model demonstrate an adequate repayment mechanism is important for protecting the Medicare program. However, as discussed in more detail later in this section, we are proposing certain modifications to the repayment mechanism requirements applicable to ACOs under the program's two-sided model(s) (Track 2 and proposed Track 3). These proposed modifications are based on our experience with the repayment mechanism requirements and are intended to reduce the burden of these requirements on ACOs.
Hence, we are revisiting our policies related to Tracks 1 and 2 in order to smooth the on ramp for organizations participating in the Shared Savings Program. First, we propose to remove the requirement at § 425.600(b) for Track 1 ACOs to transition to Track 2 after their first agreement period. Second, we propose to modify the financial thresholds under Track 2 to reduce the level of risk that ACOs must be willing to accept. Taken together, we believe there are a number of advantages to smoothing the on ramp by implementing these proposed policies. We believe that removing the requirement that ACOs transition to a two-sided model in their second agreement period will provide organizations, especially newly formed, less experienced, and smaller organizations, more time to gain experience in the program before accepting performance-based risk. In particular, we believe the proposed changes would encourage continued participation in the program by potentially successful ACOs that would otherwise drop out because of the requirement to transition to the two-sided model in their second agreement period. We further believe the proposal to allow organizations to gain more experience under a one-sided model before moving forward to a two-sided model would encourage earlier adoption of the shared savings model by organizations concerned about being required to transition to performance-based risk before realizing savings under a one-sided model. We believe incorporating the opportunity for ACOs to remain in Track 1 beyond their first agreement period could have a beneficial effect with respect to the care that beneficiaries receive. Specifically, to the extent that more ACOs are able to remain in the program, a potentially broader group of beneficiaries will have access to better coordinated care through an ACO. In addition, allowing ACOs additional time to make the transition to performance-based risk would reduce the chances that a high-performing ACO, which believes that it is not yet ready to assume greater financial risk, will either cease to participate in the program to avoid risk or find it necessary to engage in behaviors primarily intended to minimize that risk rather than improve patient care.
Further, we believe that ACOs that accept financial responsibility for the care of beneficiaries have the greatest beneficial effects for the Medicare program and its beneficiaries. Therefore, we expect that ACOs participating in the Shared Savings Program move in the direction of accepting performance-based risk. Thus, while we believe it is appropriate to offer additional time for ACOs under a one-sided model, we also believe there should be incentives for participants to voluntarily take on additional financial risk. There should also be disincentives to discourage organizations from persisting in a shared savings only risk track indefinitely. Therefore, we believe that distinguishing the financial attractiveness of the one-sided model from the two-sided model by dropping the sharing rate in Track 1 for ACOs participating in Track 1 for a subsequent agreement period and modifying the risk inherent in Track 2 would signal to ACOs the importance of moving toward performance-based risk and encourage ACOs to voluntarily enter the two-sided model as soon as they are able. Finally, we believe that adopting restrictions to prevent organizations that have not achieved certain minimum performance requirements with respect to cost and quality of care, based on their experience to date, from obtaining additional agreement periods under Track 1 can serve as an appropriate program safeguard against entities remaining in the program that are not fully committed to improving the quality and efficiency of health care service delivery.
b. Proposals Related to Transition From the One-Sided to Two-Sided Model
We considered several options to better balance both our intent to encourage continued participation by ACOs that entered the program under the one-sided model but that are not ready to accept performance-based risk after 3 years of program participation with our concern that allowing a shared savings only option will discourage ACOs capable of taking risk from moving to a two-sided model. We considered the following options: (1) Revising the regulations to allow ACOs that enter the program under the one-sided model to continue participation in Track 1 for more than one agreement period; (2) extending the initial 3-year agreement period for an additional 2 years for ACOs that enter the program under Track 1, but that do not believe that they are ready to advance to a risk-based track; and (3) allowing ACOs to continue participation in Track 1 for more than one agreement period, but revising the one-sided model to decrease the financial attractiveness of the model, so as to encourage ACOs ready to accept performance-based risk to transition to a two-sided model.
Among these options, we believe the third option offers a good balance of encouraging continued participation in addition to encouraging progression along the on-ramp to performance-based risk. Therefore, we propose to remove the requirement at § 425.600(b) that ACOs that enter the program under Track 1 (one-sided model) must transition to Track 2 (two-sided model) after one agreement period, if they wish Start Printed Page 72805to continue participating in the Shared Savings Program. Instead, we propose to revise the regulation to permit ACOs that have completed a 3-year agreement under Track 1 to enter into one additional 3-year agreement under Track 1. We believe that continued participation in the Shared Savings Program, generally, should be made available to ACOs that demonstrate they have been compliant with the program requirements, or are working through corrective action plans to CMS' satisfaction, with safeguards in place to ensure they will meet program requirements in the future. In section II.C.3. of this proposed rule, we proposed criteria for determining whether to allow ACOs that are currently participating in the program to renew their participation agreements for subsequent agreement periods. We seek to encourage the continued participation of ACOs that are successful and have the potential to move toward accepting greater responsibility for the care of their beneficiaries, but also encourage their progression along the risk continuum. Thus, we propose to make the option of participating in Track 1 for a second agreement period available to only those Track 1 ACOs that—(1) meet the criteria established for ACOs seeking to renew their agreements (as proposed in section II.C.3 of this proposed rule, including demonstrating to CMS that they satisfied the quality performance requirements under Subpart F such that they were eligible to share in savings in at least one of the first two performance years of the previous agreement period) and (2) in at least one of the first two performance years of the previous agreement period, they did not generate losses in excess of the negative MSR. For example, assume a Track 1 ACO has 15,000 assigned beneficiaries with an MSR of 2.7 percent. If we calculate that this ACO's expenditures exceeded the ACO's benchmark by 2.7 percent or more in both of the first two performance years, then CMS would not accept this ACO's request to renew its agreement under the one-sided model. If the ACO's financial performance results in expenditures in excess of the negative MSR in only one of the first two performance years, then we would accept this ACO's request to renew its participation agreement under the one-sided model, provided all other requirements for renewal were satisfied.
We believe that requiring ACOs to meet these requirements in order to remain in Track 1 will prevent consistently poor performers from being able to seamlessly continue in program participation under the one-sided model while permitting some leeway for ACOs that are new to the program and may have had some difficulty in cost or quality performance in one of the two first performance years. We also believe that these additional eligibility criteria serve as an important safeguard to reduce the potential for ACOs to participate in the program for reasons other than a commitment to improving the value of health care services. We recognize that because our assessment would be based on only 2 years of data, we would not have a complete picture of the ACO's performance during the agreement period. That is, an ACO may financially perform very poorly, exceeding the negative MSR in its first and second performance years, but demonstrate a trend in a direction that could ultimately lead to better performance in the third year. Under our proposal this ACO would not be permitted to renew its agreement under Track 1 for a second agreement period. However, an argument could be made that this ACO simply needed the additional time under a one-sided model to gain experience and start improving. We therefore seek comment on whether we should also consider the direction the ACO's performance is trending when determining whether to permit renewal of an ACO's participation agreement under Track 1. We also seek comment on whether other options for such ACOs, short of refusing their participation in a second agreement period under Track 1, would better serve program goals. We note that such ACOs would not be precluded from renewing their participation agreement in order to participate under a two-sided risk track, consistent with § 425.600(c). We also emphasize that in addition to meeting the specific criteria to be eligible to continue in Track 1, the ACO must also demonstrate that it meets the requirements to renew its agreement under proposed § 425.224, which would include the requirement that the ACO establish that it is in compliance with the eligibility and other requirements of the Shared Savings Program.
In addition, as part of our proposal to allow ACOs to participate in a second agreement period under the one-sided model, we propose to reduce the sharing rate by 10 percentage points for ACOs in a second agreement period under Track 1 to make staying in the one-sided model less attractive than moving forward along the risk continuum. As a result, the maximum sharing rate for an ACO in a second agreement period under Track 1 would be 40 percent.
Accordingly, in addition to our proposed change to § 425.600(b) to allow ACOs to participate under Track 1 for a second agreement period, we propose to modify § 425.604(d) to provide that the maximum sharing rate during a second agreement period under Track 1 will be 40 percent. As a result, ACOs that continue to participate under the one-sided model and are eligible for shared savings will receive a smaller share of those savings compared to ACOs participating under the one-sided model in their first agreement period and ACOs participating under a two-sided model. We believe permitting one additional agreement period under Track 1, but at a reduced sharing rate, will encourage the continued participation of ACOs that are successful and have the potential to move toward accepting greater responsibility for the care of their beneficiaries, but also encourage their progression along the risk continuum. However, as discussed later in this section, we also recognize that limiting ACOs to only two agreement periods under Track 1 may encourage ACOs to progress along the on-ramp to risk earlier than they otherwise might if they were permitted to remain under the one-sided model for several agreement periods.
We further note that this option to participate under the one-sided model agreement in a subsequent agreement period is only available to ACOs that have completed or are in the process of completing an agreement under the one-sided model. That is, we will not permit an ACO under a two-sided model to subsequently participate under a one-sided model.
We seek comment on this proposal. In particular, we request input on whether a 40 percent sharing rate in a second agreement period under the one-sided model is sufficient to incentivize an ACO that may need more time to prepare to take on two-sided performance-based risk while also encouraging ACOs that are ready to take on performance-based risk to choose to continue participation in the Shared Savings Program under a two-sided model.
We also considered other variations and options for allowing ACOs additional time in the one-sided model. For example, we considered allowing ACOs to continue under Track 1 for a second agreement period without any changes to the sharing rate (that is, retaining the 50 percent sharing rate in the second agreement period); however, we do not believe this approach would provide sufficient incentive for ACOs to be moving in the direction of adopting Start Printed Page 72806performance-based risk. We continue to believe that participating in a model with two-sided risk offers stronger incentives for ACOs to improve the quality of care and reduce costs. Currently, ACOs in their first agreement period under Track 1 may share in up to 50 percent of the savings generated for the Medicare program. We are concerned that if ACOs are able to continue to receive up to 50 percent of savings in a second agreement period there may be insufficient incentive for many ACOs that may be ready to take on two-sided risk to move to a track with two-sided risk after their first agreement period. As a result, under our proposal we would reduce the sharing rate for ACOs participating in Track 1 for a second agreement period in order to discourage prolonged participation under Track 1 and encourage progression along the on ramp to risk where an ACO may qualify for a higher sharing rate.
We also considered permitting ACOs to participate in multiple agreement periods under Track 1 and reducing the maximum sharing rate by 10 percentage points for each subsequent agreement. Such a policy may encourage more ACOs to continue to participate in the program, but also may reduce the urgency for ACOs to progress quickly along the on-ramp to risk if they are permitted to remain under the one-sided model for several agreement periods.
We also considered offering the opportunity to ACOs participating under Track 1 to extend their initial 3-year participation agreement under Track 1 by an additional 2 years. However, we note that under this option, we would not be able to rebase the benchmark, making it more likely that organizations would achieve savings without further improvements in care redesign; yet at the same time, it would be more difficult for ACOs with losses to turn around their performance. Moreover, we are concerned that limiting ACOs to only 2 additional years under Track 1 may not be sufficient for all ACOs to take the steps necessary to prepare to move to performance-based risk.
We seek comment on our proposal to permit ACOs to participate under Track 1 for a second agreement period and to reduce the maximum sharing rate to 40 percent for ACOs participating under Track 1 for a second agreement period. We also specifically seek comments on the other options we considered, including extending an ACO's Track 1 agreement period for an additional 2-years rather than permitting two 3-year agreement periods under Track 1, permitting ACOs to participate in a second agreement period under Track 1 with no change to the sharing rate, and offering multiple agreement periods under Track 1 while reducing the sharing rate by 10 percentage points for each subsequent agreement.
In the November 2011 final rule, we also addressed the possibility that an ACO may terminate or be terminated from participation in the Shared Savings Program, and the consequences for the ACO's choice of tracks in the event it reapplies to the program. We finalized a policy that would permit such ACOs to reapply to participate in the program again only after the date on which the term of their original participation agreement would have expired if the ACO had not been terminated (§ 425.222(a)). Under § 425.222(b), to be eligible to participate in the Shared Savings Program after a previous termination, the ACO must demonstrate in its application that it has corrected the deficiencies that caused it to be terminated and that it has processes in place to ensure it will remain in compliance with the terms of the new participation agreement. We note that, all applicants undergo screening with regard to their program integrity history that may result in denial of the application (§ 425.304(b)). We also provided that an ACO under the one-sided model whose participation agreement was previously terminated may reenter the program only under the two-sided model, unless it was terminated less than half-way through its agreement period under the one-sided model, in which case the ACO would be allowed to reenter the one-sided model (§ 425.222(c)). An ACO under Track 2 whose agreement was terminated may only re-apply to participate in Track 2 (§ 425.222(c)).
In light of our proposed revisions to § 425.600 to permit an ACO to participate under Track 1 for a second agreement period, we are proposing to make conforming changes to § 425.222(c) to permit previously terminated Track 1 ACOs to reapply under the one-sided model. We propose that, consistent with our existing policy under § 425.222(c), an ACO whose agreement was terminated less than half way through the term of its participation agreement under Track 1 would be permitted to reapply to the one-sided model as if it were applying for its first agreement period. If the ACO is accepted to reenter the program, the maximum sharing rate would be 50 percent. However, in the case of an ACO that was terminated more than half way through its initial agreement under the one-sided model, we propose to revise § 425.222(c) to permit this ACO to reapply for participation under the one-sided model, but to provide that the ACO would be treated as if it were applying for a second agreement period under Track 1. Thus, if the ACO is approved to participate in the program again, the reduced sharing rate of 40 percent would apply. An ACO whose prior agreement under Track 2 was terminated would still be precluded from applying to participate under Track 1.
We seek comment on this proposal.
c. Proposals for Modifications to the Track 2 Financial Model
To complement the proposals to smooth the on ramp to risk, we are also proposing to modify the financial model under Track 2 for ACOs choosing this two-sided option to further encourage ACOs to accept increased performance-based risk. Specifically, we are proposing to modify the threshold that Track 2 ACOs must meet or exceed in order to share in savings (minimum savings rate (MSR)) or losses (minimum loss rate (MLR)). We believe this modification would improve the track's attractiveness for ACOs, particularly for ACOs that may be cautious about entering a performance-based payment arrangement such as some ACOs with smaller assigned beneficiary populations or those with less experience with managing the health of populations across sites of care.
Track 2 was designed to allow more advanced ACOs the opportunity to take on greater performance-based risk in exchange for greater reward immediately, as early as their first agreement period. In the November 2011 final rule (76 FR 67904 through 67905), we discussed concerns that had been raised about allowing ACOs to participate immediately in a risk-based arrangement. Specifically, ACOs might try to avoid at-risk beneficiaries in order to minimize the possibility of realizing losses against their benchmarks or might be unable to repay the Medicare program if they have losses. We explained our belief that the use of retrospective beneficiary assignment for financial reconciliation and the program's beneficiary notification requirements would be sufficient safeguards against the prospect that ACOs participating in the two-sided model might try to avoid at-risk beneficiaries (76 FR 67904). Further, the requirement that ACOs participating in Track 2 establish an adequate repayment mechanism provides further assurance about their ability to repay shared losses to the Medicare program.
Currently, ACOs participating in Track 2 are eligible to share in a greater Start Printed Page 72807percentage of savings than ACOs participating in Track 1, but are also accountable for a share of losses compared to their benchmark. ACOs may elect to enter Track 2 in their first 3-year agreement period, or after completing one agreement period under Track 1. Under the Track 2 financial model, an ACO must have savings that meet or exceed a 2 percent threshold to be eligible to share in savings or additional expenditures that meet or exceed a 2 percent threshold to be held accountable for sharing in losses (§ 425.606(b)). As compared to the MSR used for Track 1, this fixed percentage generally offers a lower savings threshold for Track 2 ACOs to meet in order to share in savings, and was established in recognition of the Track 2 ACOs' willingness to assume the risk of incurring shared losses (76 FR 67929). In contrast, although organizations participating under the Track 1 financial model must also meet or exceed a MSR in order to be eligible to share in savings (§ 425.604(b)), the MSR under the one-sided model is established for each ACO using increasing nominal confidence intervals (CI) based on the size of the beneficiary population assigned to the ACO. Thus, an ACO with the minimum 5,000 assigned beneficiaries would have a MSR based on a 90 percent CI; an ACO with 20,000 assigned beneficiaries would have a MSR based on a 95 percent CI and an ACO with 50,000 assigned beneficiaries would have an MSR based on a 99 percent CI. In addition, the MSR under the one-sided model is not allowed to fall under 2 percent for larger ACOs. Table 5 displays the MSR an ACO participating under Track 1 would have to achieve before savings could be shared based on its number of assigned beneficiaries.
Table 5—Minimum Savings Rate for Track 1
Number of beneficiaries MSR (low end of assigned beneficiaries) (percent) MSR (high end of assigned beneficiaries) (percent) 5,000-5,999 3.9 3.6 6,000-6,999 3.6 3.4 7,000-7,999 3.4 3.2 8,000-8,999 3.2 3.1 9,000-9,999 3.1 3.0 10,000-14,999 3.0 2.7 15,000-19,999 2.7 2.5 20,000-49,999 2.5 2.2 50,000-59,999 2.2 2.0 60,000 + 2.0 As we described in the rulemaking establishing the Shared Savings Program (76 FR 67927), the MSR thresholds that apply under Track 1 were established on the basis of standard inferential statistics and provide confidence that, once the savings achieved by the ACO meet or exceed the MSR, the change in expenditures represents actual performance improvements by the ACO as opposed to normal variations.
Our experience with the program suggests that some ACOs, particularly ACOs with small assigned populations or those with less experience, are hesitant to elect Track 2 given the risk of losses and their inexperience with population management. Therefore, we have explored ways to reduce financial risk for ACOs participating under Track 2. One way to reduce financial risk under Track 2 would be to modify the current MSR and MLR under this track. By increasing the MSR and MLR thresholds beyond the current 2 percent, financial risk would be reduced for Track 2 ACOs because they would have to incur higher losses in order to be held accountable for shared losses. However, an ACO would also have to achieve a greater level of savings under a higher MSR in order to share in savings. In exploring potential modifications to the MSR and MLR under Track 2, we also considered increasing them using a fixed percent. For example, we considered using an MSR and MLR threshold of 3 or 4 percent that would apply to all ACOs participating in Track 2.
After considering these options, we concluded that using the same methodology currently used to establish the MSR under the one-sided model, which is based upon the size of the beneficiary population assigned to the ACO, to establish both the MSR and MLR under Track 2, would serve two purposes. Specifically, in comparison with the existing fixed 2 percent MSR and MLR that currently apply to ACOs in Track 2, it would further protect ACOs against the risk of losses likely due to normal variation while offering further protection to the Medicare program from paying for shared savings likely due to normal variation. The methodology that we used to establish the MSRs for Track 1 based upon the size of the assigned beneficiary population was intended to provide confidence that shared savings would not be earned by random chance alone (76 FR 67928). Similarly, basing the MLR under Track 2 on the size of an ACO's assigned beneficiary population would serve to statistically protect ACOs with smaller assigned populations from losses that result from normal variation, and we believe this change would make it more likely that such ACOs will be willing to take on performance-based risk under Track 2.
Therefore, we are proposing to retain the existing features of Track 2 with the exception of revising § 425.606(b) to allow the MSR and MLR to vary based on the ACO's number of assigned beneficiaries according to the methodology outlined for setting the MSR under the one-sided model in § 425.604(b) as shown in Table 6. We believe that by building in greater downside protection, this proposal may help smooth the on-ramp to performance-based risk for ACOs, particularly ACOs with smaller assigned populations, making the transition to a two-sided model more attractive.Start Printed Page 72808
Table 6—Proposed Minimum Savings Rate and Minimum Loss Rate for Track 2
Number of beneficiaries MSR/MLR (low end of assigned beneficiaries) (percent) MSR/MLR (high end of assigned beneficiaries) (percent) 5,000-5,999 3.9 3.6 6,000-6,999 3.6 3.4 7,000-7,999 3.4 3.2 8,000-8,999 3.2 3.1 9,000-9,999 3.1 3.0 10,000-14,999 3.0 2.7 15,000-19,999 2.7 2.5 20,000-49,999 2.5 2.2 50,000-59,999 2.2 2.0 60,000 + 2.0 With the proposed addition of Track 3 to the program, discussed later in this section, Track 2 can be viewed as a first step for some organizations to accepting performance-based risk. As such, providing an MLR that is more protective of ACOs may attract greater participation in performance-based risk under Track 2, particularly by ACOs with smaller assigned populations or those with less experience managing populations.
We seek comments on this proposal as well as other options that could potentially make Track 2 more financially attractive to ACOs. We request that commenters indicate why they believe an alternative option would be more attractive to ACOs than the one proposed and the specific reason why the option would be beneficial. We also request that commenters consider whether additional safeguards should be implemented to appropriately protect the Medicare Trust Fund, if an alternative approach were to be adopted. We also seek comment on whether we should consider implementing the prospective assignment approach proposed for Track 3 under Track 2 and whether doing so would enhance or erode the incentives for organizations to take on risk.
3. Creating Options for ACOs That Participate in Risk-Based Arrangements
a. Overview
As noted previously, we are pleased with the overall interest in the Shared Savings Program. However, we would also like to increase interest in the program by expanding the range of opportunities and models for organizations to improve the cost and quality of care delivered to Medicare FFS beneficiaries by assuming greater financial risk for their assigned beneficiaries.
In January 2012, the Innovation Center began testing the Pioneer ACO Model. The Shared Savings Program and the Pioneer ACO Model incorporate the same fundamental structure with a group of healthcare providers and suppliers coming together to form an ACO that agrees to be accountable for the care provided to a population of Medicare FFS beneficiaries. The quality reporting requirements are the same for Shared Savings Program ACOs and Pioneer ACOs. However, the Pioneer ACO Model and Shared Savings Program differ on several key elements, including the methodologies used for benchmarking, payment reconciliation, and assignment. For instance, the Pioneer ACO Model offers ACOs a greater sharing rate (up to 70 percent based on quality performance in performance year 2 of the model) compared to the Shared Savings Program, which currently offers a maximum sharing rate of 60 percent for ACOs choosing Track 2. Under the Pioneer ACO Model, beneficiaries are aligned to a Pioneer ACO prospectively at the start of each performance year and can only be removed from the list of aligned beneficiaries retrospectively based on certain exclusion criteria. In contrast, under the Shared Savings Program, beneficiaries are assigned to an ACO under Track 1 or Track 2 based upon a preliminary prospective assignment methodology with retrospective reconciliation after the end of the performance year that ultimately assigns a beneficiary to the ACO based on whether ACO professionals provided the plurality of primary care services to that beneficiary during the performance year. All Pioneer ACOs must agree to accept performance-based risk, and the financial risk increases over the course of their agreement period, whereas ACOs participating in the Shared Savings Program have an option to participate in a shared savings only model (Track 1) and for those ACOs that choose to accept performance-based risk (Track 2), the shared loss rate for which the ACO is at risk remains same throughout the agreement period. There are also a number of other differences between the two initiatives. Key features of the Pioneer ACO Model are explained in the Request for Application available online at http://innovation.cms.gov/Files/x/Pioneer-ACO-Model-Request-For-Applications-document.pdf,, and an updated table on payment arrangements is available online at http://innovation.cms.gov/Files/x/Pioneer-ACO-Model-Alternative-Payment-Arrangements-document.pdf.
In the November 2011 final rule (76 FR 67907), we expressed our intent to gain experience with alternative payment models through the Innovation Center before potentially adopting them more widely in the Shared Savings Program. Currently, testing of the Pioneer ACO Model is still underway, and we do not yet have a completed evaluation of that test. However, we have heard from stakeholders that there are certain aspects of the Pioneer ACO Model that may be appealing to some organizations and that we might consider incorporating into the Shared Savings Program. Therefore, in light of our experience with the Shared Savings Program, comments from stakeholders, and early responses to the Pioneer ACO Model, we have considered certain modifications to the financial models and arrangements available under the Shared Savings Program that might encourage organizations to take on increasing financial risk in order to motivate even greater improvements in care, and also minimize the barriers faced by some ACOs that limit their willingness to accept performance-based risk.
In evaluating what features might encourage ACOs to take on increasing financial risk, we considered several Start Printed Page 72809options, including modifying Track 1, modifying or eliminating Track 2, adding a Track 3 to supplement the existing ones, or a combination of these options. After reviewing these options, we are proposing to use our authority under section 1899(i)(3) of the Act to create an additional risk-based option for ACOs ready to take on increased performance-based risk.
To exercise our authority under section 1899(i)(3) of the Act, we must demonstrate that this policy; (1) “ . . . does not result in spending more for such ACO for such beneficiaries than would otherwise be expended . . . if the model were not implemented . . . .” and (2) “will improve the quality and efficiency of items and services furnished under this title.” We applied this authority when proposing a two-sided risk-based model in our April 2011 proposed rule (76 FR 19603), which was modified and made final in in our November 2011 final rule (76 FR 67909). As discussed in our final rule (76 FR 67904), we believed that Track 2 would provide an opportunity for organizations more experienced with care coordination and risk models that are ready to accept performance-based risk to enter a sharing arrangement that provides greater reward for greater responsibility. We believe that proposed Track 3 would offer an additional opportunity for ACOs to accept greater responsibility for beneficiary care in exchange for the possibility of greater reward. Moreover, we do not believe that adding a second two-sided risk model would result in an increase in spending beyond what would otherwise occur. To the contrary, as discussed later in our Regulatory Impact Analysis, our initial estimates suggest that the inclusion of Track 3 along with the other proposals made in this rule would improve savings for the Trust Funds resulting from this program. Further, we believe that adding Track 3 would improve the quality of care furnished to Medicare FFS beneficiaries because ACOs participating under Track 3 would have an even greater incentive to perform well on the quality measures in order to maximize the percentage of savings they may receive, while limiting their liability for any losses that might be incurred.
Hence, we are proposing to develop a new risk-based Track 3 under § 425.610, which would be based on the current payment methodology under Track 2, but would also incorporate some different elements that may make it more attractive for entities to accept increased performance-based risk.
In general, unless otherwise stated, we are proposing to model Track 3 off the current provisions governing Track 2, which in turn are modeled on Track 1, to have the same general eligibility requirements, quality performance standards, data sharing requirements, monitoring rules, and transparency requirements. However, as we discuss later in this section, we are proposing certain discrete features for Track 3 that will differentiate it from Track 2. Specifically, we propose to make modifications to the beneficiary assignment methodology, sharing rate, MSR and MLR, and performance payment and loss sharing limits. These proposals are discussed in detail in the following sections.
b. Proposals for Assignment of Beneficiaries Under Track 3
(1) Background
Currently, beneficiaries are assigned to Shared Savings Program ACOs participating under Track 1 and Track 2 based on the assignment methodology that is described in detail in the November 2011 final rule and in section II.E. of this proposed rule. Beneficiary assignment is based on the certified ACO participant list and drives a variety of program operations described in more detail in section II.B. of this proposed rule. An assigned beneficiary population is determined for each of the benchmark years as well as each performance year and used to determine the average per capita costs of the ACO's assigned FFS population in each of those years. Additionally, when an ACO enters the program, and on a quarterly basis thereafter, we perform a preliminary prospective assignment, based on the most recent 12 months of available claims data, to provide the ACO with information about the FFS population it has served in the past and that is likely to be assigned to the ACO at the end of the performance year. After the end of each performance year, we perform a final retrospective reconciliation to generate the final list of beneficiaries that chose to receive the plurality of their primary care services from ACO professionals applying the assignment methodology established under Subpart E of the regulations. Under this methodology, in developing the final list of assigned beneficiaries for the performance year, beneficiaries are both added to and removed from the preliminary prospectively assigned beneficiary lists provided to ACOs. This final list of assigned beneficiaries becomes the basis for calculating the average per capita expenditures for the performance year, and is used for financial reconciliation.
In this section, we discuss our proposals to apply a methodology to assign beneficiaries prospectively to Track 3 ACOs. However, since the program's operations currently center on retrospective assignment, we also considered a number of issues important to implementing prospective assignment for Track 3 ACOs. Specifically, we discuss our proposals for: (1) A prospective assignment methodology; (2) the timing for performing prospective assignment; (3) exclusion criteria to be applied to the prospective list at the end of the benchmark or performance year; and (4) addressing overlap and interactions between prospective assignment for Track 3 ACOs and the preliminary prospective assignment and retrospective reconciliation for Track 1 and Track 2 ACOs.
(2) Proposal for prospective assignment under Track 3
In the November 2011 final rule that established the Shared Savings Program, we adopted a preliminary prospective assignment model with retrospective reconciliation because we believed it would provide ACOs with adequate information to redesign their care processes while also encouraging ACOs to standardize these care processes for all Medicare FFS beneficiaries instead of focusing care management activities on a small subset of their FFS population. Further, we expressed our view that this approach would provide sufficient incentives for each ACO to provide quality care to its entire beneficiary population (76 FR 67864).
We continue to believe that the current Shared Savings Program assignment methodology offers strong incentives for health system redesign to impact the care for all FFS beneficiaries that receive care from ACO professionals. As a result, we believe the assignment methodology currently used for the Shared Savings Program limits the potential for gaming and reduces the motivation to target beneficiaries for avoidance. This methodology may also improve care for beneficiaries who are newly diagnosed with high cost health problems during a performance year. For example, a FFS beneficiary diagnosed with cancer during a performance year would benefit from interacting with ACO providers/suppliers that have incentives to be vigilant for beneficiaries who are likely to be assigned to their ACO retrospectively. Intervening early in the care of such patients may improve the quality and coordination of their care and reduce the cost of that care compared to what it might have been Start Printed Page 72810without the early intervention by the ACO and its ACO providers/suppliers.
On the other hand, while many beneficiaries routinely see the same providers and suppliers from year to year, FFS beneficiaries that are assigned to an ACO have freedom to choose their healthcare providers and, unlike patients enrolled in many managed care plans, are not locked into seeing only ACO providers/suppliers. As a result, there is no absolute certainty that preliminarily prospectively assigned beneficiaries will continue to receive the plurality of their primary care services from ACO professionals during the performance year. Thus, there can potentially be differences between the preliminary assigned beneficiary list that the ACO receives at the start of the performance year, and every quarter thereafter, and the final assigned beneficiary list that is generated at the time of retrospective reconciliation, which is based on the actual utilization of primary care services by beneficiaries during the performance year. Given our experience with the Shared Savings Program and Physician Group Practice Demonstration before it, this is not an unexpected or unanticipated result of the methodology used to assign FFS beneficiaries who retain their freedom to choose providers under traditional FFS Medicare. That being said, the need to account for both the ebb and flow of assigned beneficiaries under the preliminary prospective assignment methodology with retrospective reconciliation used in the Shared Savings Program may discourage participation in risk-based arrangements by ACOs that seek greater certainty about the population on whom they will be assessed.
As an alternative, beneficiaries could be prospectively assigned to an ACO prior to the start of the performance year. An example of prospective alignment can be found in the Pioneer ACO Model, where beneficiaries are aligned to Pioneer ACOs prior to the start of each performance year. Under the Pioneer ACO Model, the list of prospectively aligned beneficiaries is reconciled at the end of the year to exclude certain beneficiaries from the list, for example, beneficiaries who were not eligible for alignment during the performance year; however, no new beneficiaries are added to the list. This alternative assignment methodology arguably provides Pioneer ACOs with a more targeted set of FFS beneficiaries on whom to focus their care redesign efforts during the performance year. The beneficiary alignment methodology used under the Pioneer Model can be reviewed in more detail on the Innovation Center Web site: http://innovation.cms.gov/initiatives/Pioneer-ACO-Model/
A prospective assignment methodology may offer ACOs a more narrowly defined target population and greater certainty about where to focus their care redesign processes. This improved certainty may be an important factor in an ACO's willingness to take on greater performance-based risk because the ACO may be better positioned to make decisions regarding where to make investments in infrastructure to deliver enhanced services. Given the higher levels of performance-based risk associated with the Pioneer ACO Model, the Innovation Center elected to use a prospective assignment methodology specifically to provide participating ACOs with greater certainty regarding their assigned beneficiary populations in order to allow them to better target their care coordination efforts to those patients.
Potential disadvantages of a prospective assignment methodology, such as the one used under the Pioneer ACO Model, are that it may encourage ACOs to narrowly focus on a subset of FFS beneficiaries in the care of their ACO providers/suppliers while not doing as much to incentivize organizations to broadly redesign care processes to improve the care for all FFS beneficiaries under the care of providers and suppliers participating in the ACO. These incentives arise because ACOs know in advance the subset of their patients for which their performance will be measured.
However, despite these concerns, we acknowledge that a prospective assignment methodology may offer greater certainty and a more narrowly defined target population for some ACOs, and these may be important factors in an ACO's willingness to take on greater performance-based risk where the ACO must make decisions regarding where to make investments in infrastructure to deliver enhanced services. We further believe that ACOs will have strong incentives to provide their prospectively assigned beneficiaries high-quality, low-cost care in order to discourage them from seeking care outside of the ACO and that beneficiaries that are prospectively assigned to an ACO will continue to be protected from concerns related to inappropriate limitations on care under traditional FFS Medicare because of their ability to choose their providers. Under the Shared Savings Program, there is no lock in for beneficiaries, therefore, we believe a prospective assignment methodology under the Shared Savings Program presents limited risks to FFS beneficiaries. Thus, having considered the relative advantages and disadvantages of prospective and retrospective assignment methodologies for FFS beneficiaries, we are proposing to implement a prospective assignment methodology for Track 3 ACOs. This prospective assignment methodology would use the same stepwise assignment methodology under § 425.402 to assign beneficiaries to ACOs in Track 3 as is currently used to assign beneficiaries to ACOs participating under Track 1 and Track 2. The major difference would be that beneficiaries would be assigned to Track 3 ACOs prospectively, at the start of the performance year, and there would be no retrospective reconciliation resulting in the addition of new beneficiaries at the end of the performance year. The only adjustments that would be made at the end of the performance year would be to exclude beneficiaries that appeared on the prospective assignment list provided to the ACO at the start of the performance year that no longer meet eligibility criteria. For the reasons discussed in the November 2011 final rule (76 FR 67851), we believe that this proposed prospective assignment methodology meets the requirement under section 1899(c) of the Act that assignment be based on the “utilization of primary care services” provided by physicians that are ACO professionals. We propose to codify this methodology in the regulations at § 425.400(a)(3).
In summary, while we have concerns that prospective assignment may inadvertently increase incentives for gaming and avoidance of at-risk beneficiaries, we have taken steps to minimize these incentives by retaining other Shared Savings Program policies and procedures such as risk-adjusting expenditures and monitoring ACOs to ensure they are not engaging in gaming or avoidance of at-risk beneficiaries. Moreover, our proposal to exclude only those beneficiaries that no longer meet the eligibility criteria for assignment to an ACO should reduce the probability that attempts by the ACO to “cherry pick” or avoid at-risk beneficiaries during the performance year would succeed. Therefore, we believe the concerns associated with a prospective assignment methodology are balanced by the potential that establishing a new Track 3 has to encourage ACOs to accept greater responsibility and financial risk for the care provided to their patients in return for the possibility of achieving greater rewards. We seek comment on these proposals. In particular, we seek comment on ways to Start Printed Page 72811mitigate concerns regarding gaming and avoidance of at-risk beneficiaries under a prospective assignment methodology, whether implementing a prospective approach to assignment will dilute the program goals of delivery system redesign, and whether there are additional programmatic considerations that should be taken into account as a result of our proposal to apply a prospective assignment methodology in Track 3.
Because of the differences between the Shared Savings Program and the Pioneer ACO Model, we emphasize that the proposed prospective assignment methodology under Track 3 is not identical to the methodology used under the Pioneer ACO Model, but is tailored to the Shared Savings Program. Specifically, we propose to assign beneficiaries to an ACO participating under Track 3 using the assignment algorithm that is specified in Subpart E of the Shared Savings Program regulations, and described in more detail in section II.E. of this proposed rule.
c. Proposed Exclusion Criteria for Prospectively Assigned Beneficiaries
Next we considered how to reconcile the prospective beneficiary assignment list at the conclusion of the performance year. We recognize that changes in circumstances may cause prospectively assigned beneficiaries to no longer be eligible for assignment to an ACO at the end of a performance year. For instance, during the course of a benchmark or performance year a beneficiary may fall under one of the assignment exclusion criteria specified in proposed § 425.401(b). The proposed exclusion criteria, found at § 425.401(b), mirror the proposed eligibility criteria under § 425.401(a) with the exception of assignment to another Medicare initiative involving shared savings. This is because we believe it is appropriate to exclude only those prospectively assigned beneficiaries that are no longer eligible to be assigned to an ACO. We do not believe, however, that it will be necessary to exclude beneficiaries that are assigned to another shared savings initiative because we intend to adopt procedures to ensure that a beneficiary who is prospectively assigned to an ACO participating under Track 3 would not be assigned to another Medicare initiative involving shared savings. Therefore, we propose to perform a limited reconciliation where beneficiaries would only be removed from the prospective assignment list at the end of the year if they were not eligible for assignment at that time under the criteria in proposed § 425.401(b). For example, if a prospectively assigned beneficiary chose to enroll in Medicare Advantage (MA) at the beginning of the performance year, that beneficiary would be removed from the beneficiary assignment list at the end of the year and the beneficiary's expenditures would not be used in determining the ACO's financial performance for that year. We note that under this proposal, beneficiaries would be removed from the prospective list, but would not be added as they are in the retrospective reconciliation used under Tracks 1 and 2. Additionally, unlike the preliminary prospective assignment methodology with retrospective reconciliation used in Tracks 1 and 2, we note that under this proposal, similar to the methodology used under the Pioneer ACO Model, beneficiaries would not be removed from the prospective beneficiary assignment list because the beneficiary chose to receive primary care services during the performance year from practitioners other than those participating in the ACO. In other words, the ACO will be held accountable for all beneficiaries that appear on the prospective assignment list, with the narrow exception of those beneficiaries who are not eligible for assignment at the time of reconciliation based on the limited set of proposed exclusion criteria under proposed § 425.401(b). We believe that this methodology will help to mitigate concerns that ACOs may attempt to avoid caring for high risk beneficiaries that appear on their prospective beneficiary assignment list because the ACO will continue to be held accountable for the quality and cost of the care furnished to these beneficiaries even if the ACO providers/suppliers are not directly involved in their care. However, we note that this may mean that ACOs will be held accountable for beneficiaries with whom their ACO providers/suppliers have had little contact during the year, and therefore may have limited opportunity to affect their care. We seek comment on our proposal to assign FFS beneficiaries prospectively to ACOs and to apply limited exclusion criteria to reconcile the beneficiary assignment list at the end of the performance year.
d. Proposed Timing of Prospective Assignment
We believe it is important to provide Track 3 ACOs with their lists of prospectively assigned beneficiaries close to the start of each performance year so that these ACOs may begin to target their care coordination processes and to support ACO operations. Ideally, the prospective list of assigned beneficiaries would be generated based on the 12 months immediately preceding the performance year. However, we need a certain amount of time to generate and validate assignment lists and provide the information to the ACOs. Therefore, we must find a balance between allowing time to produce and deliver prospective assignment lists to Track 3 ACOs as near as possible to the start of each performance year with our desire to base prospective assignment on the most recent available data. For Tracks 1 and 2, we assign beneficiaries based on a 12 month period. We similarly propose to use a 12-month assignment period for Track 3. Under Tracks 1 and 2, we use the most recent available 12 months of data to determine the list of preliminarily prospectively assigned beneficiaries and data from the 12 months of the performance year to determine final assignment at the time of reconciliation. Ideally, under Track 3, we would determine prospective assignment for an ACO's performance year based on complete data for the most recent prior calendar year, for example, the third benchmark year or the previous performance year. For instance, in prospectively assigning beneficiaries to a Track 3 ACO for the performance year that begins in January 1, 2016, we would ideally have complete claims data for 2015. However, if we were to wait to obtain complete claims data for the prior calendar year, we would not be able to produce and deliver lists of prospectively assigned beneficiaries to Track 3 ACOs before the start of the performance year. In performing beneficiary assignment, we determine whether ACO professionals participating in an ACO have provided the plurality of a beneficiary's primary care services as compared to ACO professionals in all other ACOs and individual practitioners or groups of practitioners identified by TINs that are not participating in an ACO. We treat ACOs as a collection of TINs for the purpose of determining whether the ACO provided the plurality of the beneficiary's primary care services. Further, we accept new ACOs into the Shared Savings Program annually, with a participation agreement start date of January 1 of the following year. To most accurately and fairly prospectively assign beneficiaries, it is important to perform assignment by taking into consideration existing ACOs as well as new entrants to the program. Therefore, to assure that we can accurately prospectively assign beneficiaries to Start Printed Page 72812ACOs under Track 3, our timeline for producing the prospective assignment lists for Track 3 ACOs must factor in the time frames associated with the program's application cycle (which typically concludes in late November/early December of each calendar year).
We considered several options for establishing the 12-month period for prospective assignment under Track 3. One option would be to use the most recent 12-month period prior to the relevant performance year for which data are available. That is, we would use a 12-month assignment window that is offset from the calendar year. For instance, to establish the assignment list for the performance year beginning January 1, 2016, we could use an assignment window from October 1, 2014 through September 30, 2015. We also considered the option of using complete claims data for the calendar year prior to the performance year (this would synchronize with the timing of the financial calculations for setting the ACO's benchmark, as discussed in more detail in II.F.3.f. of this section); however, under these parameters Track 3 ACOs would receive their prospective assignment lists well into the first quarter of each performance year. We believe Track 3 ACOs would find such a delay in their receipt of their prospective assignment list burdensome for carrying out the ACO's health care operations, including care coordination processes and data analysis. We believe the first option best balances the availability of claims data with our belief that it is important to produce and deliver these prospective beneficiary assignment lists near the start of each performance year. Therefore, we are proposing to base prospective assignment on a 12-month assignment window (off-set from the calendar year) prior to the start of the performance year. We further propose to define an “assignment window” at § 425.20 as the 12-month period used to assign beneficiaries to an ACO. The assignment window for Tracks 1 and 2 would be based on a calendar year while the assignment window for Track 3 would be based on the most recent 12 months for which data are available, and which would be off-set from the calendar year. We propose to make conforming changes to the regulations to refer to the assignment window where appropriate.
e. Proposals for Addressing Interactions Between Prospective and Retrospective Assignment Models
Because there are markets in which there are multiple ACOs, we anticipate that there will be interactions between prospective assignment for Track 3 ACOs and preliminary prospective assignment with retrospective reconciliation for Track 1 and Track 2 ACOs. Under the Shared Savings Program, a beneficiary may only be assigned to a single ACO for purposes of determining the ACO's financial and quality performance during a performance year. Accordingly, a beneficiary that is prospectively assigned to a Track 3 ACO would remain assigned to the Track 3 ACO for the performance year even if the beneficiary chose to receive a plurality of his or her care outside the ACO. Furthermore, we propose that the beneficiary would remain assigned to the Track 3 ACO even if we determine as part of the retrospective reconciliation for Track 1 and Track 2 ACOs that the beneficiary actually received the plurality of his or her care from ACO professionals in another ACO. Similarly, a beneficiary prospectively assigned to a Track 3 ACO would remain assigned to that ACO even if we subsequently determine the beneficiary actually received the plurality of his or her primary care from ACO professionals participating in another Track 3 ACO. In other words, we propose that once a beneficiary is prospectively assigned to a Track 3 ACO, the beneficiary will not be eligible for assignment to a different ACO, even if the beneficiary chose to receive a plurality of his or her primary care services from ACO professionals in that ACO during the relevant performance year. As an aside, we note that it is unlikely that such a beneficiary would be assigned prospectively to that same Track 3 ACO for the next performance year.
f. Proposals for Determining Benchmark and Performance Year Expenditures Under Track 3
As specified in the November 2011 final rule, we establish the historical benchmark for ACOs in Tracks 1 and 2 by determining the per capita Parts A and B fee-for-service expenditures for beneficiaries that would have been assigned to the ACO in any of the 3 most recent years prior to the start of the agreement period using the ACO participant TINs identified at the start of the agreement period (§ 425.602(a)). For each benchmark year that corresponds to a calendar year, this includes calculating the payment amounts included in Parts A and B fee-for-service claims using claims received within 3 months following the end of the calendar year (referred to as a “3 month claims run out”) with a completion factor, excluding IME and DSH payments and considering individually beneficiary-identifiable payments made under a demonstration, pilot or time limited program (§ 425.602(a)(1)). Similarly in determining shared savings and losses for Tracks 1 and 2 (under § 425.604 and § 425.606), we use a 3-month claims run out with a completion factor to calculate an ACO's per capita expenditures for each performance year. Calculations of the ACO's performance year expenditures include the payment amounts of Part A and B fee-for-service claims. These calculations similarly exclude IME and DSH payments, and take into consideration individually beneficiary identifiable payments made under a demonstration, pilot or time limited program. We believe this approach is well accepted and therefore propose to use the same general methodology for determining benchmark and performance year expenditures under Track 3. We also propose to add a new regulation at § 425.610 to address the calculation of shared savings and losses under Track 3.
In establishing the historical benchmark for Track 3 ACOs, we propose to determine the beneficiaries that would have been prospectively assigned to the ACO during each of the 3 most recent years prior to the start of the agreement period; basing benchmark year assignment on a 12-month assignment window offset from the calendar year prior to the start of each benchmark year. However, we propose that we would still determine the Parts A and B fee-for-service expenditures for each calendar year, whether it is a benchmark year or a performance year, using a 3-month claims run out with a completion factor for these prospectively assigned beneficiaries. We would exclude IME and DSH payments and account for individually beneficiary-identifiable payments made under a demonstration, pilot or time limited program during the calendar year that corresponds to the benchmark or performance year. For example, for an ACO entering Track 3 beginning January 1, 2016, we would determine the benchmark based on CYs 2013, 2014, and 2015. We would determine a prospective list of beneficiaries using the assignment window for each year (based on an off-set 12 month period such as October 1, 2011 through September 30, 2012 for BY1) as discussed previously. However, the claims used to determine the per capita expenditures for BY1 would be based on claims submitted during the calendar year from January 1, 2013 through December 31, 2013. The same pattern would be used to determine the Start Printed Page 72813assignment and per capita expenditures for BY2 and BY3. We would apply the same pattern going forward to calculate per capita expenditures for the performance years.
We believe this methodology is advantageous for several reasons. First, this methodology would remove actuarial bias between the benchmarking and performance years for assignment and financial calculations, since the same method would be used to determine the assignment and financial calculations for each benchmark and performance year. Second, basing the financial calculations on the calendar year is necessary to align with actuarial analyses with respect to risk score calculations and data inputs based on national FFS expenditures used in program financial calculations that depend on the calendar year (for example, national FFS trend factors for the historical benchmark, national FFS growth factors used in creating the updated benchmark, and truncation points).
We note that the timing of the generation of historical benchmark reports for Track 3 ACOs would also be consistent with the current schedule for generating these reports for ACOs in Tracks 1 and 2. That is, for an ACO that begins Track 3 in 2016, the prospective beneficiary assignment list would be available immediately at the beginning of the performance year and the historical benchmark report would be available following the 3 month claims run out, sometime after the first quarter of 2016.
g. Proposals for Risk Adjusting the Updated Benchmark for Track 3 ACOs
Another aspect of the financial models used under the Shared Savings Program that we considered when developing Track 3 is our methodology for risk adjusting an ACO's updated benchmark expenditures to account for changes in severity and case mix for beneficiaries assigned in the current performance year. Currently, under Track 1 and Track 2, the risk adjustment methodology differentiates between newly and continuously assigned beneficiaries, as defined under § 425.20. A newly assigned beneficiary is a beneficiary assigned in the current performance year who was neither assigned to nor received a primary care service from any of the ACO participants during the most recent prior calendar year. A continuously assigned beneficiary is a beneficiary assigned to the ACO in the current performance year who was either assigned to or received a primary care service from any of the ACO participants during the most recent prior calendar year. As specified under § 425.604(a), and § 425.606(a), we use updated CMS-HCC prospective risk scores to account for changes in severity and case mix for newly-assigned beneficiaries. We use demographic factors to adjust for these changes in severity and case mix for continuously assigned beneficiaries. However, if the CMS-HCC prospective risk scores for the continuously assigned population show a decline, we use the lower risk score to adjust for changes in severity and case mix for this population. As we explained in the November 2011 final rule (76 FR 67918), we believe that this approach to risk adjustment strikes a fair balance between accounting for changes in the health status of an ACO's population while not encouraging changes in coding practices for care provided to beneficiaries who remain continuously assigned to the ACO or avoidance of high risk beneficiaries. We believe that the existing risk adjustment methodology has been effective in achieving this balance under Tracks 1 and 2, which use a retrospective assignment methodology for purposes of financial reconciliation, and that it would be appropriate to apply a similar approach to risk adjusting the updated benchmark for Track 3 ACOs, even though we are proposing a prospective beneficiary assignment methodology. We believe that this risk adjustment methodology is relevant to updating ACO benchmarks under both a retrospective assignment model and a prospective assignment model. We believe that as in the existing Tracks, it is important to ensure that ACOs participating under the proposed Track 3 are not encouraged to modify their coding practices in order to increase the likelihood of earning shared savings; rather, shared savings should result from actual reductions in Medicare expenditures for assigned beneficiaries.
Therefore, we carefully considered the risk adjustment methodology in the context of our proposal to use a prospective assignment methodology under Track 3. We determined that while the same general risk adjustment methodology could be used, there are certain minor modifications that must be made to accommodate the prospective assignment approach. Specifically, we determined that the existing definitions of newly and continuously assigned beneficiaries must be adjusted for Track 3 ACOs.
Both definitions refer to determining whether the beneficiary was assigned to the ACO or received primary care services from an ACO participant in the “prior calendar year”. However, our proposal for Track 3 assignment does not correspond to the 12 months in a calendar year. Instead, as proposed in the section, we would use an off-set 12-month period prior to the relevant performance or benchmark year to prospectively assign beneficiaries. If we continue to use a calendar year as the basis for determining continuously and newly assigned beneficiaries, very few beneficiaries would be designated as newly assigned for each performance year and we would expect that the majority of assigned beneficiaries would be designated as continuously assigned. As a consequence, the major risk adjustment applied under Track 3 would be based on demographic factors only. We do not believe this policy would strike the same balance achieved when applied under a model with retrospective assignment (Track 1 and Track 2).
Therefore, we propose refining our definitions of newly and continuously assigned beneficiaries at § 425.20 to also be consistent with our proposed prospective assignment approach for Track 3. Specifically, we propose to replace the reference to “most recent prior calendar year” with a reference to “the assignment window for the most recent prior benchmark or performance year.” Thus, for Track 3 the reference period for determining whether a beneficiary is newly or continuously assigned will be most recent prior prospective assignment window (the off-set 12 months) before the assignment window for the current performance year and the reference period for determining whether a Track 1 or 2 beneficiary is newly or continuously assigned will continue to be the most recent prior assignment window (the most recent calendar year). Our proposed risk adjustment methodology for Track 3 is reflected in the proposed new regulation at § 425.610(a).
h. Proposals for Final Sharing/Loss Rate and Performance Payment/Loss Recoupment Limit under Track 3
Currently, an ACO that meets all the requirements for receiving shared savings payments under the one-sided (Track 1) model can qualify to receive a shared savings payment of up to 50 percent of all savings under its updated benchmark, not to exceed 10 percent of its updated benchmark, as determined on the basis of its quality performance. Likewise, a Track 2 ACO can potentially receive a shared savings payment of up to 60 percent of all savings under its updated benchmark, not to exceed 15 percent of its updated benchmark. The higher sharing rate and performance Start Printed Page 72814payment limit under Track 2 were established as incentives for ACOs to accept greater financial risk for their assigned beneficiaries in exchange for potentially higher financial rewards. Additionally, a Track 2 ACO is accountable for between 40 to 60 percent of all losses under its updated benchmark, depending on the ACO's quality performance. The amount of shared losses for which an ACO is liable, however, may not exceed 5 percent of its updated benchmark in the first performance year, 7.5 percent in the second performance year, and 10 percent in the third performance year and any subsequent performance year (§ 425.606(g)). In the November 2011 final rule (76 FR 67937), we stated that we believe these progressively higher caps on losses “achieve an appropriate balance between providing ACOs with security about the limit of their accountability for losses while encouraging ACOs to take increasing responsibility for their costs and protecting the Medicare Trust Funds.” We note that under one of the payment arrangements available under the Pioneer ACO Model, a Pioneer ACO can qualify to receive up to 75 percent of shared savings, not to exceed 15 percent of its benchmark. Under this payment arrangement, Pioneer ACOs may also be responsible for shared losses of up to 15 percent of their benchmark.
Currently, only five of the ACOs participating in the Medicare Shared Savings Program are participating under Track 2. Given this level of ACO participation under this model, we considered options for improving the attractiveness of the final sharing rate and performance payment limit in a risk model. For example, we considered whether the current sharing rate under Track 2 is insufficient to encourage ACO participation under a risk-based model and whether increasing the sharing rate would better attract organizations to take on performance-based risk. We also observed that the higher sharing rates available under the Pioneer ACO model have appeared to be helpful in encouraging ACO participation. Further, we believe it is important to draw a distinction between the sharing rates available under Track 2 and the proposed Track 3. As discussed later in this section, we are proposing that ACOs participating in Track 3 would be subject to a fixed 2 percent MLR (compared to the proposed revisions that would allow the MSR and MLR under Track 2 to vary between 2.0 percent and 3.9 percent). Thus, we believe it is important to reward Track 3 ACOs with a greater level of savings for taking on this greater level of risk. Accordingly, we are proposing to set the sharing rate under Track 3 at 75 percent. Likewise, we considered whether the current 15 percent performance payment limit for Track 2 ACOs may discourage participation under a risk-based model. In our November 2011 final rule (76 FR 67935 through 67936), we noted a range of commenters had urged us either to eliminate the limits on shared savings or to apply higher payment limits for both models, with limits as high as 25 percent. We explained that retaining the performance payment limits is necessary to comply with the statute and important for ensuring against providing an overly large incentive that may encourage ACOs to generate savings through inappropriate limits on necessary care. As was the case when we issued that rule, we continue to believe that retaining a performance payment limit is necessary. However, we believe that a modest increase in the performance payment limit for ACOs willing to take on the greater level of risk under Track 3 may balance our concerns while increasing the attractiveness of the model. Accordingly, for Track 3 ACOs, we are proposing a performance payment limit not to exceed 20 percent of the ACO's updated benchmark. We note that the shared loss rate would similarly increase to a maximum of 75 percent to retain symmetry within the model which is comparable to the approach we used to establish the shared loss rate for Track 2 ACOs.
To establish even stronger incentives for encouraging ACOs to assume greater responsibility for the quality and cost of the care furnished to their assigned beneficiaries, we are also considering variations on the previous proposals. Currently, under the two-sided model, an ACO's quality score is taken into account when calculating the ACO's final sharing rate. Under Track 2, an ACO with poor quality performance may be responsible for repaying Medicare up to 60 percent of losses while an ACO with very high quality performance may be responsible for repaying Medicare only 40 percent of the losses incurred (see § 425.606(f)). If we retain symmetry between the shared savings and shared losses methodologies under Track 3, an ACO with very low quality performance could be responsible for repaying Medicare up to 75 percent of losses while a Track 3 ACO with very high quality performance would only be responsible for 25 percent of losses.
However, it may not be desirable under Track 3 to allow such a broad range for shared losses, which could be viewed as increasing the potential reward without similarly increasing risk. Therefore, we considered other options for increasing potential shared savings while also increasing risk, or holding risk constant compared to Track 2. Under one option we considered, Track 3 ACOs would be responsible for the maximum percentage of losses, that is, 75 percent, but quality performance would only protect them to the same extent it protects Track 2 ACOs, such that ACOs with very high quality scores would limit their percentage of losses to 40 percent. Alternatively, we could retain the minimum and maximum shared loss rates found under Track 2 (that is, the range of 40 percent to 60 percent, depending on quality performance) but the maximum shared savings rate would be increased to 75 percent in order to encourage participation in a model with increased risk.
After considering these options, in § 425.610(d) and (f) we are proposing to increase the sharing rate for Track 3 ACOs so that they may qualify for up to 75 percent of all savings under their updated benchmark in conjunction with accepting risk for up to 75 percent of all losses, depending on the quality performance of the organization for the reasons articulated previously. We are also proposing under new § 425.610(e)(2) to increase the performance payment limit to 20 percent of an ACO's updated benchmark. Additionally, rather than gradually increasing the cap on shared losses for Track 3 ACOs (as is done under Track 2), in § 425.610(g), we are proposing that the amount of shared losses for which an ACO may be liable may not exceed 15 percent of its updated benchmark in each year of the ACO's 3-year agreement period. We believe that capping losses at 15 percent would provide adequate protection to the Medicare Trust Funds while limiting risk to ACOs, thereby encouraging them to progress along the risk continuum. We also propose that ACOs with high quality performance would not be permitted to reduce the percentage of shared losses for which they would be responsible for each year of the agreement period below 40 percent. We believe it is important for Track 3 ACOs to be held responsible for at least the same amount of downside risk as Track 2 ACOs. We seek comment on whether this percentage is high enough to protect the Trust Funds or whether it should be increased, for example, to 50 percent or 60 percent. We also seek comment on whether our Start Printed Page 72815proposal to establish a range of 40 percent to 75 percent for shared losses should, in turn, impact the amount of shared savings available to Track 3 ACOs. For example, should we permit Track 3 ACOs to earn a parallel range of 40 percent to 75 percent of shared savings. In other words, once the ACO has met criteria for sharing in savings, the minimum guaranteed amount of shared savings would be 40 percent with a maximum of 75 percent.
We seek comments on these proposals and the proposed new regulation at § 425.610. In particular, we request comment on the appropriate minimum percentage of shared losses under Track 3. We also seek comment on the appropriate percentage for the performance payment limit and loss recoupment limit and whether there are reasons to set these at 15 percent and 10 percent respectively, rather than our proposal of 20 percent and 15 percent respectively.
Finally, we are also proposing to make certain technical, conforming changes to § 425.606, which governs the calculation of shared savings and losses under Track 2, to reflect our proposal to incorporate a second two-sided risk model into the Shared Savings Program. We seek comments on these proposed changes and on any other technical changes to our regulations that may be necessary in order to reflect the proposal to add a new Track 3.
i. Proposals for Minimum Savings Rate and Minimum Loss Rate in Track 3
In this proposed rule, we are proposing to replace the current fixed 2 percent minimum savings rate (MSR) and minimum loss rate (MLR) under Track 2 with a MSR and MLR that will vary based on the number of beneficiaries assigned to the ACO, mirroring the methodology currently used to determine the MSR under Track 1. We proposed this change as a way to reduce financial risk and thereby increase the attractiveness of Track 2 to prospective ACOs and ACOs continuing in the program for a second or subsequent agreement period. Specifically, we believe it is important to offer a risk-based option attractive to smaller ACOs that may be hesitant to take on performance-based risk. Under the proposed modifications to Track 2, smaller ACOs would have an MLR greater than 2 percent, which would provide additional protection to these ACOs against incurring losses as a result of normal variations in expenditures. Moreover, while reducing financial risk for Track 2 ACOs, the proposal would also offer greater protection to the Medicare program by raising the savings threshold that must be achieved before an ACO would be eligible to share in savings for all but the largest ACOs.
As discussed previously in this section, we are proposing to establish a new Track 3 as an additional option for participation in the Shared Savings Program with stronger incentives to encourage ACOs to accept greater responsibility and risk for their beneficiaries. Hence, for Track 3 ACOs, we are proposing to apply the same fixed 2 percent MSR and MLR that currently apply to Track 2 ACOs. As we discussed in the November 2011 final rule (76 FR 67929), establishing the Shared Savings Program, the use of an MSR and MLR remains important under a two-sided risk model to guard against normal variations in costs, so that ACOs share savings or losses with the program only under those circumstances in which we can be confident that those savings and losses are the result of the ACOs' actions rather than normal variation. As we noted in that final rule, it is more appropriate to employ a fixed MSR under a two-sided model than under the one-sided model. First, given the potential for shared loss, the greater predictability of a fixed MSR is more likely to attract organizations to participate under the model. Second, there is greater protection for the Medicare Trust Fund from normal variation under a two-sided model because ACOs accept the risk of repaying the Medicare program for shared losses. Therefore, in the November 2011 final rule (76 FR 67929), we adopted a fixed 2 percent MSR and MLR for ACOs participating under Track 2. We selected 2 percent because this is the lowest MSR under the one-side model and was also the MSR that was used in the PGP demonstration. As discussed previously in this section, we are now proposing to modify the MSR and MLR under Track 2 to vary based upon the size of the ACO. We believe this change would improve the attractiveness of Track 2 by offering ACOs that may be less experienced with performance-based risk greater protection against shared losses. However, because Track 3 is intended for ACOs that are willing to accept a greater degree of risk in exchange for the opportunity to share in a greater percentage of shared savings, we believe it is appropriate to use a fixed 2 percent MSR and MLR under this track. We believe that setting the MSR and MLR at this level would offer greater predictability, which may attract more ACOs to participate in Track 3. In addition, as we discussed in the November 2011 final rule (76 FR 67929), the requirement that ACOs repay shared losses offers additional protection to the Medicare Trust Funds, which allows for the application of a lower, fixed MSR. Accordingly, we propose to apply the same fixed 2 percent MSR and MLR that currently apply to Track 2 ACOs to ACOs that elect to participate in Track 3. This proposal is reflected in paragraph (b) of the proposed new regulation at § 425.610. We seek comments on this proposal.
Although we are proposing to apply a fixed MSR and MLR of 2 percent under Track 3, we also considered other options for establishing the MSR and MLR for Track 3 ACOs, including an option that would remove the MSR and MLR entirely. Under this option, ACOs would be subject to normal variation around their benchmark so that they would be held responsible for all losses when performance year expenditures were above the benchmark in addition to sharing in any savings if performance year expenditures fell below the benchmark. Another option could be to set both the MSR and MLR to 1 percent instead of 2 percent. This would serve to increase both risk of sharing losses and savings, but not as much as doing away with the MSR and MLR entirely. We specifically seek comment on whether it would be desirable to remove the MSR and MLR entirely under Track 3 as well as alternative levels at which to set the MSR and MLR for ACOs participating under Track 3. We will consider comments that are received regarding these alternatives in determining the final MSR and MLR that would apply under Track 3.
4. Seeking Comment on Ways To Encourage ACO Participation in Performance-Based Risk Arrangements
We are encouraged by stakeholder interest in the Shared Savings Program. Since implementation of the Shared Savings Program in 2012, there are now more than 330 organizations participating. Based on the initial experience we have gained with the Shared Savings Program, however, we believe ACOs are very reluctant to accept two-sided performance-based risk arrangements in which ACOs would share in both Medicare savings and losses because only a small number of ACOs have agreed to participate in the Shared Savings Program under Track 2, which provides for two-sided performance-based risk. Ninety-eight percent of the ACOs participating in the Shared Savings Program have elected to participate under Track 1 (shared savings only). We believe that under a two-sided performance-based risk model, ACOs have much stronger Start Printed Page 72816incentives to achieve high quality and to avoid unnecessary costs, which is why we are proposing Track 3 as a possibly more attractive alternative to Track 2. The incentive for ACOs to achieve high quality and avoid unnecessary costs under a two-sided performance-based risk model is supported by the impact analyses performed by the CMS actuary provided in section V. of this proposed rule. Accordingly, in order for the Shared Savings Program to be effective and sustainable over the long term, we believe we may need to further strengthen our efforts to transition the Shared Savings Program to a two-sided performance-based risk program in which ACOs would share in both Medicare savings and losses.
We received a wide range of suggestions from ACOs, the Brookings Institution, MedPAC, and other stakeholders of ways to improve the Shared Savings Program and to address ACO concerns that they believe are essential to the longer term success of the program. The Brookings Institution has identified a number of critical issues that warrant further discussion and consideration for ensuring the continued success of ACOs in the Medicare Program. See “Issue Brief: How to Improve the Medicare Accountable Care Organization (ACO) Program” at: http://www.brookings.edu/~/media/research/files/papers/2014/06/16%20medicare%20aco%20challenges%20and%20alternatives/2%20mcclellan%20et%20al%20%20medicare%20aco%20program%2062014.pdf.
In a June 16, 2014 letter to CMS (http://www.medpac.gov/documents/06162014_ACO_issue_letter_2014_COMMENT.pdf), MedPAC raises several issues for consideration in connection with CMS ACO models in the short and long term. MedPAC indicates that ACOs represent an opportunity to transform the delivery system, but MedPAC believes that realizing that opportunity would require providers to change their practices and take a risk on this new payment system, and that we would need to be flexible and responsive as the program evolves. MedPAC's recommendations are based on discussions with representatives from many ACOs, structured interviews and case studies with Pioneer ACOs, analysis of early data on ACO performance, and reviewing progress with CMS staff. MedPAC reports that many ACO providers/suppliers who they have spoken with have patients in both MA plans and FFS Medicare. Under MA, providers can furnish services and use techniques that are not available under FFS Medicare or, by extension, under the current rules governing the Shared Savings Program. For example, pursuant to section 1861(i) of the Act, FFS Medicare requires a 3-day inpatient hospital stay before a SNF services will be covered under Medicare Part A, but MA plans can offer a waiver of the 3 day prior inpatient hospitalization requirement as a supplemental benefit. ACOs have indicated that they like the flexibility that capitated payments would give them to redesign care and benefits to meet the needs of their patient populations.
Under the current Medicare FFS system, providers have a financial incentive to increase their volume of services. As a result, many current Medicare regulations are designed to prevent overuse of services and the resulting increase in Medicare spending in this context. In brief, MedPAC believes that moving to two-sided performance-based risk under the Shared Savings Program would provide strong incentives for organizations to control costs, which should, in turn, open up the opportunity for regulatory relief across a broad range of issues. Removing certain regulatory requirements may provide ACOs with additional flexibility to innovate further, which could in turn lead to even greater cost savings. These views are supported by analyses performed by CMS actuaries that suggest two-sided performance-based risk provides stronger incentives for ACOs to achieve savings. Thus, ACOs and MedPAC have encouraged us to consider relaxing certain specific FFS Medicare payment and other rules under two-sided performance-based risk models in the Shared Savings Program.
In the sections that follow, we solicit comment on several options that are currently under consideration for inclusion in the Shared Savings Program. We first consider options that would implicate the waiver authority under section 1899(f) of the Act and then consider other options that could be implemented independent of waiver authority. Although we are not specifically proposing these options at this time, we will consider the comments that are received regarding these options during the development of the final rule, and may consider adopting one or more of these options in the final rule.
a. Payment Requirements and Other Program Requirements That May Need To Be Waived in Order To Carry Out the Shared Savings Program
As noted previously, few organizations have chosen to participate in the Shared Savings Program under two-sided performance-based risk. In addition to the elements designed to enhance participation in a two-sided performance-based risk track under the proposed new Track 3, we believe it may be necessary and appropriate to provide for additional program flexibilities to increase ACOs' willingness to participate in the Shared Savings Program under two-sided performance-based risk arrangements to increase quality and decrease cost growth. These possible additional flexibilities could include use of our waiver authority to waive certain Medicare Program rules under section 1899(f) of the Act, which provides authority for the Secretary to waive “such requirements of . . . title XVIII of this Act as may be necessary to carry out the provisions of this section.” This provision affords broad authority for the Secretary to waive statutory program requirements as necessary to carry out the provisions of section 1899 of the Act. In order to waive FFS payment or other program rules, the waiver must be determined to be necessary for CMS to carry out the provisions of section 1899 of the Act, which govern the Shared Savings Program. (The authority at section 1899(f) of the Act has been used by the Office of Inspector General and CMS to issue an interim final rule with comment period setting forth waivers of certain fraud and abuse authorities (76 FR 67992), which was published concurrently with the November 2011 final rule establishing the Shared Savings Program. This rulemaking does not address fraud and abuse waivers, and we are not soliciting comment on such waivers.)
As noted previously, we are encouraged by the robust participation of organizations under the one-sided model of the Shared Savings Program. However, we continue to believe that the long term effectiveness and sustainability of the program depend on encouraging ACOs to progress along the performance-based risk continuum. Given the very limited ACO interest thus far in two-sided performance-based risk, and the comments and suggestions by stakeholders, we now believe that the authority under section 1899(f) of the Act to waive certain payment or other program requirements may be necessary to carry out the provisions of the Shared Savings Program and to permit effective implementation of two-sided performance-based risk tracks under the program. As discussed previously, on the April 2011 proposed rule, both we and many commenters believe that models where ACOs bear a degree of financial risk hold the potential to Start Printed Page 72817induce more meaningful systematic change than one-sided models. We believe that ACOs that bear financial risk would have a heightened incentive to restrain wasteful spending by their ACO participants and ACO providers/suppliers. This, in turn, may reduce the likelihood of over-utilization. In these circumstances, waiver of certain payment and other programmatic rules for ACOs with two-sided risk may be appropriate to give providers more flexibility under FFS Medicare to provide appropriate care for beneficiaries.
We would point out that while we are considering these waiver issues under the Shared Savings Program, we are also actively moving forward with testing certain payment rule and other waivers as part of models tested by the Innovation Center under section 1115A of the Act, including the Pioneer ACO Model. For example, as explained below, we already have a few months of data from our initial test of the waiver of the SNF 3-day rule under the Pioneer ACO Model, and we are in the process of testing beneficiary attestation under the Pioneer ACO Model. In addition, under the demonstration authority in section 402 of Public Law 90-248, as amended (42 U.S.C. 1395b-1), we granted Massachusetts General Hospital (MGH) the ability to admit certain patients enrolled in its Care Management for High Cost Beneficiaries Demonstration directly into a SNF without a 3-day prior inpatient hospitalization, and we intend to release a report evaluating this waiver later this year. Based on our experience with the waiver of the SNF 3-day rule in the MA program, and an initial, limited assessment of the MGH waiver performed by CMS actuaries, we expect that the waiver of the SNF 3-day rule under the Pioneer ACO Model will result in savings for the Medicare Trust Funds.
We are learning from these tests and would seek to refine our policies as we move forward. Through such testing we frequently identify issues that neither we nor stakeholders had previously identified. Developing and implementing such policies in a test environment provides an opportunity for us to better understand the effects on providers, beneficiaries, and Medicare as well as to further fine tune the operations.
We welcome comments on possible waivers under section 1899(f) of the Act of certain Medicare payment or other program requirements suggested by stakeholders that might be necessary to permit effective implementation of two-sided performance-based risk in the Shared Savings Program. As noted previously, we will consider the comments that are received during the development of the final rule, and in the final rule may consider waiving certain requirements if we conclude that such a waiver is necessary in order to carry out the Shared Savings Program. We are especially interested in comments explaining how such waivers may be necessary to encourage ACOs to accept performance-based risk arrangements under the Shared Savings Program, and how such waivers could provide ACOs with additional ways to increase quality of care and reduce unnecessary costs that are not permitted under FFS Medicare, but that could be appropriately used in the context of an ACO model that incorporates two-sided performance-based risk. What program integrity and beneficiary protection risks could be introduced by waivers of the payment and program rules described later in this section of this proposed rule and how could we mitigate those risks? Would a waiver of these requirements impact notification to beneficiaries of participation in the Shared Savings Program as required under § 425.312? What operational issues do ACOs and CMS need to consider and what processes would ACOs need to have in place to implement these alternative payment and other program policies? What implications would there be for ACO infrastructure including IT and other systems and processes? What provider education would be needed? What other issues should be considered when making use of waiver authority with respect to payment and program rules? Should any waivers apply to all two-sided performance-based risk tracks or should they be limited to a specific two-sided risk track? Should waivers be available only for those organizations willing to take on the greatest performance-based risk under the Shared Savings Program? For example, should waivers be limited to the use of organizations participating in Track 3 because participants in Track 3 would agree to be held accountable for up to 75 percent of shared losses compared to participants in Track 2 who would agree to be held accountable for up to 60 percent of shared losses? Should the waivers be made available to all organizations participating in the applicable risk tracks or only to those ACOs that have successfully participated in the Shared Savings Program or another ACO model previously?
We also note that the ability to implement any waivers of payment or program rules may vary for ACOs participating under Track 2 and Track 3 because of the differences in how beneficiaries are assigned to ACOs under those Tracks. We are considering whether a waiver that applies only to beneficiaries assigned to the ACO would perhaps be more appropriately implemented under a model in which there is prospective assignment of beneficiaries, such as proposed Track 3. Under prospective assignment, beneficiaries would be assigned to the ACO for the entire performance year, and it would thus be clear as to which beneficiaries the waiver applied. Having clarity as to the beneficiary to which a waiver applies may be important for the ACO to comply with the conditions of the waiver and could also improve CMS' ability to monitor waivers for misuse. Another option would be to apply the waivers to any FFS beneficiary cared for by an eligible ACO. Then the waiver could be available to all ACOs participating in a two-sided risk track, regardless of whether the assignment is prospective or retrospective. Another option would be to apply such waivers to beneficiaries that appear on the quarterly lists of preliminarily prospectively assigned beneficiaries. Under this approach, the population for whom the waiver is available would likely change from quarter to quarter. We seek comment on whether any waivers of payment or program rules would be more viable under proposed Track 3, which includes prospective beneficiary assignment, versus Track 2 in which beneficiaries are assigned using a preliminary prospective assignment methodology with final retrospective reconciliation. Specifically, would a waiver require a fully prospective list of assigned beneficiaries for the performance year or would it be feasible to use a preliminary prospective list of beneficiaries that is likely to change at the end of the performance year? What are the other operational issues we should consider?
Specific payment and program rules for which we believe waivers could be necessary under the Shared Savings Program to support ACO efforts to increase quality and decrease costs under two-sided performance-based risk arrangements and for which we invite comments are as follows:
(1) SNF 3-Day Rule
The Medicare SNF benefit is for beneficiaries who require a short-term intensive stay in a SNF, requiring skilled nursing and/or skilled rehabilitation care. Pursuant to section 1861(i) of the Act, beneficiaries must have a prior inpatient hospital stay of no Start Printed Page 72818fewer than 3 consecutive days in order to be eligible for Medicare coverage of inpatient SNF care. We refer to this as the SNF 3-day rule. As discussed previously, we believe that the long term effectiveness and sustainability of the Shared Savings Program depend on encouraging ACOs to progress along the performance-based risk continuum. Given the very limited ACO interest thus far in two-sided performance-based risk, and the comments and suggestions by stakeholders, we now believe that the authority under section 1899(f) of the Act to waive certain payment or other program requirements may be necessary to carry out the provisions of the Shared Savings Program and to permit effective implementation of two-sided performance-based risk tracks under the program. Models where ACOs bear a degree of financial risk hold the potential to induce more meaningful systematic change. We believe that under a two-sided performance-based risk ACO model it could be medically appropriate and more efficient for some patients to receive skilled nursing care and or skilled rehabilitation services provided at SNFs without a prior inpatient hospitalization or with an inpatient hospital length of stay of less than 3 days. A waiver of this requirement could allow ACOs to realize cost savings and improve care coordination, such that they could be more willing to accept two-sided risk, which we believe is required to promote the long term effectiveness and sustainability of the Shared Savings Program.
We note that the SNF 3-day rule has been waived or is not a requirement for Medicare SNF coverage under a few CMS models or programs. For instance, the Pioneer ACO Model has recently started testing whether a tailored waiver of the SNF 3-day rule will enable the Pioneer ACOs to improve quality of care for a subset of beneficiaries requiring skilled nursing and/or skilled rehabilitation care while also reducing expenditures. ACOs under the Pioneer Model are accountable for the total costs of care furnished to their assigned beneficiary population, and must accept performance-based risk in the event that costs exceed their benchmark. This type of performance-based risk arrangement has the potential to mitigate the incentive to overuse SNF benefits. MA plans already have the flexibility not to apply the SNF 3-day rule, and we believe this flexibility is appropriate because of the financial incentives for MA plans, which operate under a capitated payment arrangement, to control total cost of patient care. As in the case of the MA program, the Pioneer ACO Model's use of shared risk arrangements is expected to deter unnecessary referral of patients to SNFs, as Pioneer ACOs are accountable for the total cost of care furnished to their assigned beneficiaries. While the financial incentive to control total cost of care in a shared savings model is not as great as in a capitated model, all Pioneer ACOs are at significant performance-based risk for exceeding their expenditure benchmarks and are clearly focused on reducing total cost of care.
The waiver of the SNF 3-day rule under the Pioneer ACO Model went into effect on April 7, 2014, for Pioneer ACOs that demonstrate through an application process that they have the capacity and infrastructure to identify and manage clinically eligible beneficiaries prospectively assigned to Pioneer ACOs who may be admitted to a SNF without the required 3-day inpatient hospital stay. All other requirements for coverage of the Medicare SNF benefit remain unchanged under the Pioneer ACO Model. Only beneficiaries that require skilled nursing and/or skilled rehabilitation care are eligible for SNF coverage without a prior 3-day inpatient hospitalization under the Pioneer ACO Model waiver. All Pioneer ACOs are eligible to apply for a waiver of the SNF 3-day rule for their prospectively assigned beneficiaries, but must demonstrate that they have the capacity to identify and manage patients who would be either directly admitted to a SNF or admitted to a SNF after an inpatient hospitalization of fewer than 3 days, by describing the staff and processes involved in the clinical management of these beneficiaries.
Further, patients eligible for coverage of SNF admissions under the terms of the waiver include only FFS Medicare beneficiaries prospectively aligned to a Pioneer ACO who do not reside in nursing homes for long-term custodial care at the time of the decision to admit to a SNF. Patients must be medically stable, have certain and confirmed diagnoses and thus not require additional diagnostic testing, not require an inpatient evaluation or treatment, and have a skilled nursing or rehabilitation need that could not be provided as an outpatient. Eligible beneficiaries must be admitted to SNFs at the direction of admitting Pioneer providers/suppliers and not at the direction of SNFs or non-Pioneer providers/suppliers. Pioneer ACOs are required to submit to CMS for approval a SNF or group of SNFs with which they wish to partner for purposes of this waiver. The designated SNFs must have the appropriate staff capacity and necessary infrastructure to carry out the activities proposed in the Pioneer ACO's application. The SNF may be, but is not required to be, a Pioneer provider/supplier. The SNF must also have, at the time of application submission, a quality rating of 3 or more stars under the CMS 5-Star Quality Rating System as reported on the Nursing Home Compare Web site. Commenters suggest that a similar waiver of the SNF 3-day rule would be appropriate for certain ACOs under the Shared Savings Program. When Congress enacted the original Medicare legislation in 1965, it created SNF coverage as a less expensive alternative to what would otherwise be the final, convalescent portion of a beneficiary's inpatient hospital stay. Accordingly, the Medicare SNF benefit was narrowly focused on “post-hospital extended care” to serve as a relatively brief and skilled “extension” of an acute care stay in a hospital. Thus, the requirement for a prior 3-day qualifying stay in an inpatient hospital was included to effectively target the limited population that the SNF benefit was designed to cover: Beneficiaries who require a short-term, intensive stay in a SNF, requiring skilled care.
Because of changes in medical care over the half century since enactment of the original Medicare legislation, it may now be medically appropriate for some patients to receive skilled nursing care and or rehabilitation services provided by SNFs without a prior inpatient hospitalization, or with an inpatient hospital length of stay of less than 3 days. It may be medically appropriate for patients to go to SNFs earlier, due to changes in medical care, given that hospital lengths of stay are shorter than they were decades ago, and the types of patients that were staying 3 days in an inpatient hospital in 1965 are no longer staying 3 days in an inpatient hospital now. Because of this, over time, we have repeatedly expressed interest in testing alternatives to the SNF 3-day rule. We have found that financial incentives need to properly align so that the appropriate patients receive SNF care. That is, we believe care must be coordinated in a manner that allows for control of total patient cost and mitigates the incentive to overutilize the SNF benefit. If alternatives to the SNF 3-day rule were to be implemented, we believe that most treatment would continue to be appropriately furnished in a hospital, either on an inpatient or outpatient basis, rather than furnished at a SNF. Therefore, we do not believe Start Printed Page 72819that application of such a waiver should result in overutilization of SNF care at the expense of appropriate acute hospital care. We would also note that under a model of accountability for total costs of care for assigned beneficiaries such as the Pioneer ACO Model or a two-sided risk track under the Shared Savings Program, the greatest savings would most likely be achieved by permitting the elimination, where appropriate, of the entire prior hospital stay (and therefore the hospital DRG payment) and improving quality of care for patients who can instead receive appropriate care through direct admission to a SNF. Permitting a shortened (less than 3 days) inpatient hospital stay prior to SNF admission would not necessarily produce significant savings to the Medicare Trust Funds, as Medicare would still pay the applicable MS-DRG amount to the hospital. Commenters, however, suggested that allowing ACOs to carefully identify beneficiaries with a prior hospital stay of less than 3 days, for whom SNF care would be clinically appropriate, could still produce cost savings for hospitals that improve their financial performance, and could contribute to ACOs' success and continued participation in the Shared Savings Program.
We believe it could be necessary to waive the SNF 3-day rule for ACOs participating under a two-sided risk track in the Shared Savings Program because the financial incentives for such ACOs to control total patient costs for their prospectively assigned beneficiaries are arguably similar to certain incentives that currently exist for MA plans and Pioneer ACOs. If we were to conclude that a waiver of the requirement for a prior 3-day qualifying stay in an inpatient hospital under waiver authority in section 1899(f) of the Act is necessary for purposes of implementing two-sided performance-based risk models under the Shared Savings Program, we would likely initially limit this waiver to ACO participants and ACO providers/suppliers under proposed Track 3. Under Track 3 beneficiaries would be prospectively assigned to the ACO for the entire year and it would thus be clear as to which beneficiaries the waiver applied. In addition, under Track 3 as proposed, organizations would agree to be held accountable for up to 75 percent of any losses compared to organizations participating under Track 2 who agree to be held accountable for up to 60 percent of any losses. Since a few organizations have been willing to participant under Track 2 without waivers, this may represent the limit of risk organizations are willing to take on without waiving the SNF 3-day rule. As mentioned previously, we believe a prospective assignment approach creates a potential pathway for improving the appropriate use of waivers by ACOs and a method for CMS to monitor its use, in addition to offering a higher sharing rate. For these reasons, we believe Track 3 may make it a better candidate for these waivers than Track 2. However, we seek comment on whether such a waiver should apply to all performance-based risk tracks. Another option would be to allow the waiver to apply to any FFS beneficiary cared for by the ACO and then the waiver could be available to all ACOs participating in a two-sided risk track, regardless of whether assignment is prospective or retrospective. Another option would be to apply any waiver to beneficiaries that appear on the quarterly lists of preliminarily prospectively assigned beneficiaries. In this case, the beneficiaries to whom the waiver applies would likely change from quarter to quarter. We anticipate that we would offer the opportunity to apply for such a waiver to ACOs using a framework similar to the one currently being tested under the Pioneer ACO Model, with appropriate revisions as necessary to accommodate the differences in beneficiary assignment methodology, as needed.
Under such a waiver, ACOs would be required to submit to CMS for approval of a SNF or group of SNFs with which they wish to partner. The designated SNFs must have the appropriate staff capacity and necessary infrastructure to carry out the activities described in the ACO's application for the waiver. The SNF would likely be required to be an ACO participant or ACO provider/supplier. We believe it would be appropriate to limit such a waiver to SNFs that are ACO participants or ACO providers/suppliers, because we believe these entities would have incentives that are most directly aligned with those of the ACO. ACOs also have stronger control and oversight over such entities because such entities are subject to Shared Savings Program requirements.
Under such a waiver, we would anticipate establishing additional requirements to ensure program transparency and help reduce the possibility for abuse of the waiver. For example, we would anticipate requiring ACOs to indicate their intent to use the waiver as part of their applications or requests for renewal of their participation agreement, and remain in compliance with program rules. To further substantiate an ACO's intent to use the waiver, we anticipate requiring that the ACO submits as part of its application documentation showing that its governing body has made and duly authorized a bona fide determination that the ACO will use the waiver (if approved by CMS) and will comply with all requirements of the waiver. As part of its application for the waiver, we would require the ACO to submit a written plan describing how it would use the waiver to meet the clinical needs of its assigned beneficiaries. We would reserve the right to deny or revoke a waiver to an ACO if it is not in compliance with requirements under the Shared Savings Program, if it does not use the waiver as described in its application, or if it does not successfully meet the quality reporting standard. ACOs with approved waivers would be required to post their use of the waivers as part of public reporting (see § 425.308) on the dedicated ACO Web page. Use of the waiver and its authorization by the governing body would be required to be documented and the documentation retained, consistent with § 425.314. We would anticipate that any waiver would be effective on the start date of the ACO's participation agreement and would not extend beyond the end of the ACO's participation in the Shared Savings Program. However, if CMS terminates the participation agreement, then the waiver would end on the date of the termination notice. We also reserve the authority to withdraw the waiver in the event we determine that there has been an abuse of the waiver. The proposed payment waivers would not protect financial arrangements between ACOs, ACO participants, ACOs providers/suppliers, or other individuals or entities providing services to ACO patients from liability under the fraud and abuse laws or any other applicable laws.
We note that we would retain the right to monitor and audit the use of such waivers. We would anticipate implementing heightened monitoring of entities that bill under payment waivers to help reduce the possibility for abuse of the waiver. We seek comment on what specific activities should be monitored to ensure that items and services are properly delivered to eligible patients, that patients are not being discharged prematurely to SNFs, and that patients are able to exercise freedom of choice and are not being steered inappropriately. We would also likely consider monitoring ACOs' marketing of services subject to payment waivers to prevent coercive or Start Printed Page 72820misleading marketing and to assess the effect on the delivery of care.
We invite comments on whether it is necessary to provide for a waiver of the SNF 3-day rule using our authority under Section 1899(f) of the Act for ACOs that choose to participate in the Shared Savings Program under two-sided performance-based risk financial arrangements. If so, what criteria would be appropriate to determine waiver eligibility under the Shared Savings Program? We note that any waiver under the Shared Savings Program for this purpose would have to be implemented consistently across all eligible ACOs. In other words, application of the waiver would be uniformly applied, and there would not be customization of the waiver or conditions for the waiver for particular eligible ACOs. With this in mind, would it be appropriate to apply the same criteria discussed earlier that are currently being used under the Pioneer ACO Model? If not, how would the criteria have to be modified? What assurances should ACOs have to make in order to be eligible to use the waiver? Are there current Shared Savings Program rules and requirements that would have to be modified to permit this waiver? Should we require that a beneficiary be admitted to a SNF that is an ACO participant or ACO provider/supplier in order for the waiver to apply? We invite comment on whether or not the SNF should be required to be an ACO provider/supplier. Would a waiver under certain conditions create any unexpected concerns about access to SNF services for the patients who need them most (that is, those beneficiaries admitted following a 3-day or longer hospital stay). Would a waiver of the SNF 3-day rule align with our policy of including primary care services furnished in SNFs in the beneficiary assignment process? Would the ACO quality measures such as the new Skilled Nursing Facility 30-Day All-Cause Readmission Measure (79 FR 67910) and the other measures used in establishing the quality performance standards that ACOs must meet in order to be eligible for shared savings provide sufficient beneficiary protections from inappropriate care or withheld care? Are there other quality standards that should apply to ACOs or post-acute care facilities that use this waiver? What other monitoring activities should be considered to guard against unintended consequences of a waiver of the SNF 3-day rule? What other criteria, operational issues or other concerns should we consider? We invite comment on these issues.
(2) Billing and Payment for Telehealth Services
Under section 1834(m) of the Act, Medicare pays for telehealth services furnished by a physician or practitioner under certain conditions even though the physician or practitioner is not in the same location as the beneficiary. The telehealth services must be furnished to a beneficiary located in one of the eight types of originating sites specified in section 1834(m)(4)(C)(ii) of the Act and the site must satisfy at least one of the requirements of section 1834(m)(4)(C)(i)(I) through (III) of the Act. Generally, for Medicare payment to be made for telehealth services under the Physician Fee Schedule several conditions must be met (§ 410.78(b)). Specifically, the service must be on the Medicare list of telehealth services and meet all of the following other requirements for payment:
- The service must be furnished via an interactive telecommunications system.
- The service must be furnished to an eligible telehealth individual.
- The individual receiving the services must be in an eligible originating site.
When all of these conditions are met, Medicare pays a facility fee to the originating site and provides separate payment to the distant site practitioner for the service.
Section 1834(m)(4)(F)(i) of the Act defines Medicare telehealth services to include professional consultations, office visits, office psychiatry services, and any additional service specified by the Secretary, when furnished via a telecommunications system. For the list of Medicare telehealth services, see the CMS Web site at www.cms.gov/teleheath/. Under section 1834(m)(4)(F)(ii) of the Act, CMS has an annual process to consider additions to and deletions from the list of telehealth services. CMS does not include any services as telehealth services when Medicare does not otherwise make a separate payment for them.
We also note that a number of CMS demonstrations include or have included testing of interventions that use electronic health records, remote monitoring, and mobile diagnostic technology as part of strategies to increase quality of care and decrease costs. For example, for the Medicare Health Support Programs (see https://www.cms.gov/Medicare/Medicare-General-Information/CCIP/index.html), participants utilized a variety of telephonic care management services and related interventions. These services included nurse-based health advice for the management and monitoring of symptoms, health education (via health information, videos, online information), health coaching to encourage self-care and self-management of chronic health conditions and medications, and health promotion and disease prevention coaching. Likewise, under the Independence at Home Demonstration, physician and nurse practitioner directed home-based primary care teams use electronic health records, remote monitoring, and mobile diagnostic technology to help reduce expenditures and improve health outcomes for Medicare beneficiaries with multiple chronic conditions (see CMS Web site at http://www.cms.gov/Medicare/Demonstration-Projects/DemoProjectsEvalRpts/Medicare-Demonstrations-Items/CMS1240082.html).
As discussed previously in section II.B.8.a of this proposed rule, section 1899(b)(2)(G) of the Act requires a Shared Savings Program ACO to “define processes to . . . coordinate care, such as through the use of telehealth, remote patient monitoring, and other such enabling technologies.” Commenters suggest that technologies that enable health care providers to deliver care to patients in locations remote from providers are being increasingly used to complement face-to-face patient-provider encounters in both urban and rural areas. In these cases, the use of remote access technologies may improve the accessibility and timeliness of needed care, increase communication between providers and patients, enhance care coordination, and improve the efficiency of care. ACOs and other commenters have suggested that a waiver of certain Medicare telemedicine payment requirements would help encourage a broader range of ACOs to more fully utilize telehealth, remote patient monitoring, and other such enabling technologies.
We note that certain professional services that are commonly furnished remotely using telecommunications technology are paid under the same conditions as in-person physicians' services, and thus do not require a waiver. Such services that do not require the patient to be present in person with the practitioner when they are furnished are covered and paid in the same way as services delivered without the use of telecommunications technology when the practitioner is in-person at the medical facility furnishing care to the patient. Such services typically involve circumstances where a practitioner is able to visualize some aspect of the patient's condition without Start Printed Page 72821the patient being present and without the interposition of a third person's judgment. Visualization by the practitioner can be possible by means of x-rays, electrocardiogram or electroencephalogram tracings, tissue samples, etc. For example, the interpretation by a physician of an actual electrocardiogram or electroencephalogram tracing that has been transmitted via telephone (that is, electronically, rather than by means of a verbal description) is a covered physician's service. These remote services are not Medicare telehealth services as defined under section 1834(m)(4)(F)(i) of the Act. Rather, these remote services that utilize telecommunications technology are considered physicians' services in the same way as services that are furnished in person without the use of telecommunications technology, and they are paid under the same conditions as in-person physicians' services, with no requirements regarding permissible originating sites.
A waiver of certain Medicare telehealth requirements could be supported by section 1899(b)(2)(G) of the Act in that it gives the use of enabling technologies, such as telehealth, as an example of a process to coordinate care, and the statute does not limit ACOs to being in rural or shortage areas where Medicare payment is available for telehealth services. As we indicated in section II.B.8.a. of this proposed rule, we welcome information from ACOs and other stakeholders about the use of such technologies to coordinate care for assigned beneficiaries. If we conclude that a waiver of certain telehealth requirements under section 1899(f) of the Act is necessary in order to carry out the Shared Savings Program, we would likely provide for a waiver of the originating site requirements of section 1834(m)(4)(C)(i)(I) through (III) of the Act that limit telehealth payment to services furnished within specific types of geographic areas or in an entity participating in a Federal telemedicine demonstration project approved as of December 31, 2000, and would also likely provide for a waiver of the originating site requirements of section 1834(m)(4)(C)(ii)(I) through (VIII) of the Act that specify the particular sites at which the eligible telehealth individual must be located at the time the service is furnished via a telecommunications system. Waiver of this requirement could allow ACOs to realize cost savings and improve care coordination, such that they would more willing to take on two-sided risk which we believe is required to promote the long term effectiveness and sustainability of the Shared Savings Program.
If we were to implement a waiver then we believe it would be appropriate to limit the use of such waivers to beneficiaries that are assigned to the ACO during the applicable performance year. We believe this would be best accomplished by permitting ACOs to use these waivers when they have a prospectively assigned population. In other words, the waivers would be limited to ACOs participating in Track 3. Prospectively assigned beneficiaries under Track 3 would be assigned to the ACO for the entire year and it would thus be clear to ACOs and CMS as to the beneficiaries for which a waiver applied. As mentioned previously, we believe a prospective assignment approach creates a potential pathway for improving the appropriate use of waivers by ACOs and a method for CMS to monitor its use. In addition, under Track 3 there would be greater opportunity for risk. For these reasons, we believe that Track 3 is potentially a better candidate for such a waiver than Track 2. However, we seek comment on whether these waivers should apply to all two-sided performance-based risk tracks. Another option would be for the waivers would apply to any FFS beneficiary cared for by an ACO and then the waiver could be available to ACOs participating in any two-sided risk track, regardless of whether the assignment is prospective or retrospective. Another option would be to apply such waivers to beneficiaries that appear on the quarterly lists of preliminarily prospectively assigned beneficiaries. Under this approach, the population for whom the waiver is available would likely change from quarter to quarter.
Under a waiver of the telehealth requirements, we would anticipate establishing additional requirements to ensure program transparency and help reduce the possibility for abuse of the waiver. For example, we would anticipate requiring ACOs to indicate their intent to use the waiver in a form and manner specified by CMS, as part of either their applications or requests for renewal of their participation agreement, and to remain in compliance with program rules. To further substantiate an ACO's intent to use the waiver, we anticipate requiring that the ACO submit as part of its application documentation showing that its governing body has made and duly authorized a bona fide determination that the ACO will use the waiver (if approved by CMS) and will comply with all requirements of the waiver. As part of its application for the waiver, we would require the ACO to submit a written plan describing how it would use the waiver to meet the clinical needs of its assigned beneficiaries. We would reserve the right to deny or revoke a waiver to an ACO if it is not in compliance with requirements under the Shared Savings Program, if it does not use the waiver as described in its application, or if it does not successfully meet the quality reporting standard. ACOs with approved waivers would be required to post their use of the waivers as part of public reporting (see § 425.308) on the dedicated ACO Web page. Use of the waiver and its authorization by the governing body would be required to be documented, and the documentation retained, consistent with § 425.314. We would anticipate that any waiver would be effective on the start date of the ACO's participation agreement and would not extend beyond the end of the ACO's participation in the Shared Savings Program. However, if CMS terminates the participation agreement, then the waiver would end on the date of the termination notice. We also reserve the authority to withdraw the waiver in the event we determine that there has been an abuse of the waiver. The proposed payment waivers would not protect financial arrangements between ACOs, ACO participants, ACOs providers/suppliers, or other individuals or entities providing services to ACO patients from liability under the fraud and abuse laws or any other applicable laws.
We note that we would retain the right to monitor and audit the use of such waivers. We would anticipate implementing heightened monitoring of entities that bill under payment waivers to help reduce the possibility for abuse of the waiver. We seek comment on what specific activities should be monitored to ensure that items and services are properly delivered to eligible patients. We would also likely consider monitoring ACOs' marketing of services subject to payment waivers to prevent coercive or misleading marketing and to assess the effect on the delivery of care.
In addition to welcoming comments related to the questions we raised in section II.B.8.a of this proposed rule, we also welcome specific comments on whether it is necessary to use our authority under Section 1899(f) of the Act to provide for a waiver for ACOs participating in the Shared Savings Program of any Medicare telehealth rules, especially for those ACOs that have elected to participate under a two-sided performance-based risk Start Printed Page 72822arrangement. We seek comment on the telehealth rules that would require a waiver and the circumstances under which a waiver would be necessary. Specifically, what aspects of current Medicare telehealth payment and other rules would it be necessary to waive in order to effectively incorporate two-sided performance-based risk into the Shared Savings Program? What factors should CMS consider if it were to provide for such a waiver to allow ACOs additional flexibility to provide a broader range of telehealth services or services in a broader range of geographic areas? Also, how should telehealth be defined? While “telehealth” is not consistently defined across payers, “telehealth” typically refers to a broader set of services, including “store and forward” services, which are not currently covered by Medicare outside of demonstration projects. Under what circumstances should payment for telehealth and related services be made? What types of services should be included—remote monitoring, remote visits and/or e-consults? What capabilities or additional criteria should ACOs meet in order to qualify for payments for telehealth services under such a waiver? In your comments, please consider quality and outcomes metrics, other requirements to ensure protection of beneficiaries and the Medicare Trust Funds, and any other design factors you think may be important.
(3) Homebound Requirement Under the Home Health Benefit
In order for Medicare to pay for home health services, a beneficiary must be determined to be “home-bound.” Specifically, sections 1835(a) and 1814(a) of the Act require that a physician certify (and recertify) that in the case of home health services under the Medicare home health benefit, such services are or were required because the individual is or was “confined to the home” and needs or needed skilled nursing care on an intermittent basis, or physical or speech therapy or has or had a continuing need for occupational therapy. A beneficiary is considered to be confined to the home if the beneficiary has a condition, due to an illness or injury, that restricts his or her ability to leave home except with the assistance of another individual or the aid of a supportive device (such as crutches, a cane, a wheelchair, or a walker), or if the beneficiary has a condition such that leaving his or her home is medically contraindicated. While a beneficiary does not have to be bedridden to be considered confined to the home, the condition of the beneficiary must be such that there exists a normal inability to leave home and leaving home requires a considerable and taxing effort by the beneficiary. Absent this condition, it would be expected that the beneficiary could typically get the same services in an outpatient or other setting. Thus, the homebound requirement provides a way to help differentiate between patients that require medical care at home versus patients who could more appropriately receive care in a less costly outpatient setting. Additional information regarding the homebound requirement is available in the Medicare Benefit Manual (Pub 100-02); Chapter 7, “Home Health Services”, Section 30.1.1, “Patient Confined to the Home”.
Some ACOs and other commenters have suggested that a waiver of this requirement would be appropriate under the Shared Savings Program, especially for ACOs that have elected to participate under a two-sided performance-based risk arrangement. They suggest that home health care would be appropriate for additional beneficiaries and could result in lower overall costs of care in some instances. For example, commenters suggest, based on their experiences outside of the Medicare FFS program, that if a beneficiary is allowed to have home health care visits, even if the beneficiary is not considered home-bound, the beneficiary may avoid a hospital admission.
If we conclude that a waiver of the homebound requirement under section 1899(f) of the Act is necessary in order to carry out the Shared Savings Program, we would expect to offer the opportunity to provide home health services to additional beneficiaries to ACOs participating under Track 3 using a process similar to the approach we discussed above for a waiver of the SNF 3-day rule for ACOs in Track 3. Specifically, ACOs participating under Track 3 have a significant financial incentive to control total patient costs. In addition, under Track 3 beneficiaries would be prospectively assigned to the ACO for the entire year, and it would thus be clear as to which beneficiaries the waiver applied. As mentioned previously, we believe a prospective assignment approach creates a potential pathway for improving the appropriate use of waivers by ACOs and a method for CMS to monitor its use. In addition, under Track 3 there would be greater opportunity for risk. For these reasons, we believe that Track 3 is potentially making a better candidate for such a waiver than Track 2. All ACOs participating under Track 3 would be eligible to apply for a waiver of the home-bound requirement for their prospectively assigned beneficiaries; however, we seek comment on whether these waivers should apply to all performance-based risk tracks. Another option would be that the waivers would apply to any FFS beneficiary cared for by the ACO and then the waiver could be available to all ACOs participating in a two-sided risk track, regardless of whether assignment is prospective or retrospective. Another option would be to apply any waiver to beneficiaries that appear on the quarterly lists of preliminarily prospectively assigned beneficiaries. In this case, the beneficiaries to whom the waiver applies would likely change from quarter to quarter. We believe we could authorize waiver of the homebound requirement under the home health benefit for those ACOs that demonstrate through the application process or in a request for renewal of their participation agreement that they have the capacity and infrastructure to identify and manage clinically beneficiaries who are not homebound, but are otherwise eligible for services under the home health benefit, and would benefit from receiving these services. As part of the application for the waiver, we would expect to require ACOs to describe the staff and processes that would be involved in the clinical management of beneficiaries receiving services pursuant to the waiver. All other requirements for the Medicare home health benefit would remain unchanged. Thus, under such a waiver, only beneficiaries that otherwise meet all program requirements to receive home health services would be eligible for coverage of home health services without being homebound.
In addition, we would require that home health services provide pursuant to the waiver at the direction of an ACO provider/supplier that is not a home health agency, to help ensure that the waiver is used appropriately. The home health agency would also likely be required to be an ACO provider/supplier. We believe it would be appropriate to limit such a waiver to home health agencies that are ACO participants or ACO providers/suppliers, because we believe these entities would have incentives that are most directly aligned with those of the ACO. ACOs also have stronger control and oversight over such entities and such entities are subject to Shared Savings Program requirements. We invite comment on whether or not the home health agency should be required to be an ACO provider/supplier. In either case, an ACO would be required to submit to CMS for approval the home Start Printed Page 72823health agency or group of home health agencies with which it wishes to partner in providing services pursuant to this waiver. The designated home health agency or agencies would be required to have the appropriate staff capacity and necessary infrastructure to carry out the processes described in the ACO's application for the waiver. In addition, a designated home health agency would be required to have, at the time of application submission, a quality rating of 3 or more stars under the CMS 5-Star Quality Rating System as reported on the Home Health Compare Web site. (For detailed information, see http://blog.cms.gov/2014/06/18/star-quality-ratings-coming-soon-to-compare-sites-on-medicare-gov/.)
Under such a waiver, we would anticipate establishing additional requirements to ensure program transparency and help reduce the possibility for abuse of the waiver. For example, we would anticipate requiring ACOs to indicate their intent to use the waiver in a form and manner specified by CMS, as part of either their applications or requests for renewal of their participation agreement, and to remain in compliance with program rules. To further substantiate an ACO's intent to use the waiver, we anticipate requiring that the ACO submit as part of its application documentation showing that its governing body has made and duly authorized a bona fide determination that the ACO will use the waiver (if approved by CMS) and will comply with all requirements of the waiver. As part of its application for the waiver, we would require the ACO to submit a written plan describing how it would use the waiver to meet the clinical needs of its assigned beneficiaries. We would reserve the right to deny or revoke a waiver to an ACO if it is not in compliance with requirements under the Shared Savings Program or if it does not successfully meet the quality reporting standard. ACOs with approved waivers would be required to post their use of the waivers as part of public reporting (see § 425.308) on the dedicated ACO Web page. Use of the waiver and its authorization by the governing body would be required to be documented, and documentation retained, consistent with § 425.314. We would anticipate that any waiver would be effective on the start date of the ACO's participation agreement and would not extend beyond the end of the ACO's participation in the Shared Savings Program. However, if CMS terminates the participation agreement, then the waiver would end on the date of the termination notice. We would also reserve the authority to withdraw the waiver in the event we determine that there has been an abuse of the waiver. The proposed payment waivers would not protect financial arrangements between ACOs, ACO participants, ACOs providers/suppliers, or other individuals or entities providing services to ACO patients from liability under the fraud and abuse laws or any other applicable laws.
We note that we would retain the right to monitor and audit the use of such waivers. We would anticipate implementing heightened monitoring of entities that bill under payment waivers to help reduce the possibility for abuse of the waiver. We seek comment on what specific activities should be monitored to ensure that items and services are properly delivered to eligible patients, and that patients are able to exercise freedom of choice and are not being steered inappropriately. We would also likely consider monitoring ACOs' marketing of services subject to payment waivers to prevent coercive or misleading marketing and to assess the effect on the delivery of care.
We invite comments on whether it is necessary to waive the homebound requirement under the home health benefit using our authority under Section 1899(f) of the Act for ACOs that choose to participate in the Shared Savings Program under two-sided performance risk financial arrangements. We also welcome comments on the potential waiver requirements discussed previously. For example, what criteria would be appropriate to determine eligibility for such a waiver under the Shared Savings Program? Are there specific categories of providers or beneficiaries to whom the waiver should (or should not) apply? If implemented under a two-sided performance-based risk model, are there additional protections for the Medicare Trust Funds or for beneficiaries that should be considered? How would a waiver complement Medicare payment for physician home visits for medically complex patients? What considerations, if any, should we take into account when adapting current 60-day episode payment amounts that require patients to be homebound in applying them to services furnished to a non-homebound population? What quality metrics should be incorporated into the quality measure framework for ACOs and our monitoring program to measure the quality of care for non-homebound home health recipients? When should the waiver be applied? Would there be specific circumstances when home health services should be available at any point without first being triggered by some health event? If so, what criteria would be necessary to differentiate these circumstances from non-covered custodial care? What other criteria or operational issues or other concerns should we also consider? We are also concerned that under a homebound waiver, beneficiaries may, in effect, be steered toward those agencies that can provide enhanced home health services to patients who are not homebound. Any such homebound waiver would not override Medicare patients' freedom of choice and that beneficiaries would remain free to select any eligible home health agency. We seek comments on ways to ensure that beneficiaries retain their freedom of choice in practice under a waiver.
We would also note that the Independence at Home (IAH) Demonstration builds on existing Medicare benefits by providing chronically ill patients with a complete range of primary care services in the home setting. Medical practices led by physicians or nurse practitioners provide primary care home visits tailored to the needs of beneficiaries with multiple chronic conditions and functional limitations. See the CMS Web site at http://innovation.cms.gov/initiatives/independence-at-home/. How could the findings from Independence at Home demonstration apply to the population of beneficiaries assigned to ACOs or receiving care furnished by ACO providers/suppliers?
(4) Waivers for Referrals to Postacute Care Settings
As a condition of participation (CoP) in Medicare, a hospital must have in effect a discharge planning process that applies to all patients, as required under § 482.43. The Interpretative Guidelines for this requirement found in the State Operations Manual, Publication 100-07, Appendix A—Survey Protocol, Regulations and Interpretive Guidelines for Hospitals, section A-0799, define hospital discharge planning as a process that involves determining the appropriate post-hospital discharge destination for a patient; identifying what the patient requires for a smooth and safe transition from the hospital to his or her discharge destination; and beginning the process of meeting the patient's identified postdischarge needs. Alternative terminology, such as “transition planning” or “community care transitions” is preferred by some, since it moves away from a focus primarily on a patient's hospital stay to consideration of transitions among the multiple types of patient care settings Start Printed Page 72824that may be involved at various points in the treatment of a given patient. This approach recognizes the shared responsibility of health care professionals and facilities as well as patients and their support persons throughout the continuum of care, and the need to foster better communication among the various groups. At the same time, the term “discharge planning” is used both in section 1861(ee) of the Act as well as in § 482.43.
The discharge planning CoP specifically addresses the role of the patient, or the patient's representative, by requiring the hospital to develop a discharge planning evaluation at the patient's request and to discuss the evaluation and plan with the patient. This is consistent with the hospital patient's rights CoP regulations at § 482.13(b)(1) and (2), which provide that the patient has the right to participate in the development and implementation of his or her plan of care, and to make informed decisions regarding his or her care. Accordingly, hospitals must actively involve patients or their representatives throughout the discharge planning process. Further, the specific discharge planning evaluation requirement to assess a patient's capability for post-discharge self-care requires the hospital, as needed, to actively solicit information not only from the patient or the patient's representative, but also from family, friends, or other support persons. The hospital must include in the discharge plan, when applicable in terms of the types of post-discharge care needs identified, a list of home health agencies (HHAs) or SNFs that are available to the patient, that are participating in the Medicare program and that serve the geographic area (as defined by the HHA) in which the patient resides, or in the case of a SNF, in the geographic area requested by the patient. HHAs must request to be listed by the hospital as available (see § 482.43(c)(6)) for further details). Further, under the CoP regulations at § 482.43(c)(7), a hospital, as part of the discharge planning process, must inform the patient or the patient's family of their freedom to choose among participating Medicare providers of post-hospital care services and must, when possible, respect patient and family preferences when they are expressed. The hospital must not specify or otherwise limit the qualified providers that are available to the patient. The discharge plan must identify any HHA or SNF to which the patient is referred in which the hospital has a disclosable financial interest, as specified by the Secretary, and any HHA or SNF that has a disclosable financial interest in a hospital under Medicare (See § 482.43(c)(8)).
The State Operations Manual (SOM), Appendix A at Section A-0823, provides additional guidance for these requirements. During the discharge planning process the hospital must inform the patient of his or her freedom to choose among Medicare-participating post-hospital providers and must not direct the patient to specific provider(s) or otherwise limit which qualified providers the patient may choose among. Hospitals have the flexibility either to develop their own lists or to print a list of skilled nursing facilities and home health agencies in the applicable geographic areas from the CMS Web sites, Nursing Home Compare (www.medicare.gov/NHcompare) and Home Health Compare (www.medicare.gov/homehealthcompare). If hospitals develop their own lists, they are expected to update them at least annually (69 FR 49226). Hospitals may also refer patients and their families to the Nursing Home Compare and Home Health Compare Web sites for additional information regarding Medicare-certified SNFs and HHAs, as well as Medicaid-participating nursing facilities. The data on the Nursing Home Compare Web site include an overall performance rating, nursing home characteristics, performance on quality measures, inspection results, and nursing staff information.
Home Health Compare provides details about every Medicare-certified home health agency in the country. Included on the Web site are quality indicators such as managing daily activities, managing pain and treating symptoms, treating wounds and preventing pressure sores, preventing harm, and preventing unplanned hospital admissions. The hospital might also refer the patient and his or her representatives to individual State agency Web sites, the Long-Term Care Ombudsman Program, Protection and Advocacy Organizations, Citizen Advocacy Groups, Area Agencies on Aging, Centers for Independent Living, and Aging and Disability Resource Centers for additional information on long term care facilities and other types of providers of post-hospital care. Having access to the information found at these sources may assist beneficiaries and their families and other caregivers in the decision making process regarding post-hospital care options. When the patient or the patient's family has expressed a preference, the hospital must attempt to arrange post-hospital care with an HHA or SNF, as applicable, consistent with that preference. If the hospital is unable to make the preferred arrangement, (for example, if there is no bed available in the preferred SNF), it must document the reason the patient's preference could not be fulfilled and explain that reason to the patient.
ACOs and MedPAC have indicated that as ACOs have started to analyze claims data on their beneficiaries, they are recognizing that certain providers may deliver higher-quality and lower-cost care than others. For example, some SNFs may deliver higher-quality care and thus appropriately lower rates of readmissions to hospitals. ACOs have indicated that they would like to have the ability to recommend high-quality SNF and HHA providers with whom they have established relationships, rather than presenting all options equally. In particular, ACOs and their ACO providers/suppliers would like to have the ability to clearly state to beneficiaries which providers they believe are best and why. However, it is not clear to them that they have the authority to do so, especially for referrals to post-acute care. ACOs suggest that the ability to make more specific recommendations would enable them to build robust networks across the continuum of care, and thus help them to give beneficiaries as much continuity as possible as they move across sites of care. Therefore, ACOs have asked that we provide clear direction on how preferred providers can be presented to beneficiaries and what represents clear notification of the beneficiary's freedom to choose among participating Medicare providers.
Based on these comments from ACOs and MedPAC, we have reviewed the relevant statutory provisions, regulations, and guidance. While we believe these materials make clear the requirements regarding how preferred providers can be represented to beneficiaries and what represents clear notification of beneficiary freedom of choice of providers, we believe we have identified one requirement that might be need to be waived. Specifically, we are considering whether it might be necessary to waive the requirement under section 1861(ee)(2)(H) of the Act that a hospital “not specify or otherwise limit the qualified provider which may provide post-hospital home services” and the portions of the hospital discharge planning CoP at § 482.43 that implement this requirement, using our waiver authority under Section 1899(f) of the Act for ACOs participating in two-sided risk tracks under the Shared Savings Program. If we were to implement such a waiver, we would anticipate making it a very narrow Start Printed Page 72825waiver. In addition, we are considering whether such a waiver would be most appropriately implemented under Track 3 in which there is prospective assignment of beneficiaries. Under Track 3 beneficiaries would be prospectively assigned to the ACO for the entire year and it would thus be clear as to which beneficiaries the waiver applied. As mentioned previously, we believe a prospective assignment approach creates a potential pathway for improving the appropriate use of waivers by ACOs and a method for CMS to monitor its use. In addition, under Track 3 there would be greater opportunity for risk. For these reasons, we believe that Track 3 is potentially a better candidate for such a waiver than Track 2. Another option is that the waiver would apply to any FFS beneficiary cared for by the ACO and then the waiver could be available to all ACOs participating in a two-sided risk track, regardless of whether the assignment is prospective or retrospective. Another option would be to apply any waiver to beneficiaries that appear on the quarterly lists of preliminarily prospectively assigned beneficiaries. In this case, the beneficiaries to whom the waiver applies would likely change from quarter to quarter. We would also anticipate imposing additional documentation requirements upon those ACOs that seek to use the waiver. Specifically, because the Shared Savings Program is built on FFS Medicare, and because we continue to support and protect beneficiaries' right to choose their providers under FFS Medicare, we are not considering a complete waiver of the requirement that a hospital, as part of the discharge planning process, not specify or otherwise limit the qualified providers that are available to the patient. This requirement is reflected in the hospital CoPs at § 482.43(c)(7). In other words, under the terms of any waiver, hospitals still would be required to inform the patient or the patient's family of their freedom to choose among participating Medicare providers of post-hospital care services and must, when possible, respect patient and family preferences when they are expressed. In addition, the hospital must also present a complete list and may not limit the qualified providers that are available to the patient. However, under a waiver of the prohibition on the specification of qualified providers, discharge planners in hospitals that are ACO participants or ACO providers/suppliers would have the flexibility to recommend high quality post-acute providers with whom they have relationships (either financial and/or clinical) for the purpose of improving continuity of care across sites of care. Such a waiver would not cover a situation in which a post-acute provider paid the ACO participant or ACO provider/supplier to be included as a recommended post-acute provider. We believe it would be appropriate to limit such a waiver to hospitals that are ACO participants or ACO providers/suppliers because we believe these entities would have incentives that are most directly aligned with those of the ACO. ACOs also have stronger control and oversight over such entities and such entities are subject to Shared Savings Program requirements. We anticipate that under a such waiver discharge planners would be required to document that the patient or the patient's family was informed of their freedom to choose a provider of post-hospital services and presented with a complete list of participating Medicare providers of post-hospital care services as well as information regarding the Medicare provider of post-hospital care services recommended by the discharge planner. We also anticipate that under such a waiver discharge planners would be required to document the data and the rationale they used as the basis for recommending any specific provider of post-hospital services. If implemented across all risk tracks, we anticipate it would apply to all FFS beneficiaries receiving services from hospitals participating in the ACO. We would additionally anticipate requiring the use of certain quality criteria for recommended providers (such as requiring that SNFs meet a minimum Star rating of 3 or more stars under the CMS 5-Star Quality Rating System as reported on the Home Health Compare Web site. For detailed information, see http://blog.cms.gov/2014/06/18/star-quality-ratings-coming-soon-to-compare-sites-on-medicare-gov/.) and documentation that the patient or the patient's family was informed of the recommended provider's quality of care, the clinical and/or financial relationship that the ACO has with the recommended provider, and any other reasons why the provider is being recommended. Furthermore, we would continue to require that the ACO respect the patient or the patient's family's preference regarding the choice of post-acute provider. Under such a waiver, we would anticipate establishing additional requirements to ensure program transparency and help reduce the possibility for abuse of the waiver. For example, we would anticipate requiring ACOs to indicate their intent to use the waiver in a form and manner specified by CMS, as part of either their applications or requests for renewal of their participation agreement, and to remain in compliance with program rules. To further substantiate an ACO's intent to use the waiver, we anticipate requiring that the ACO submit as part of its application documentation showing that its governing body has made and duly authorized a bona fide determination that the ACO will use the waiver (if approved by CMS) and will comply with all requirements of the waiver. As part of its application for the waiver, we would require the ACO to submit a written plan describing how it would use the waiver to meet the clinical needs of its assigned beneficiaries. We would reserve the right to deny or revoke a waiver to an ACO if it is not in compliance with other requirements under the Shared Savings Program, if it does not use the waiver as described in its application, or if it does not successfully meet the quality reporting standard. ACOs with approved waivers would be required to post their use of the waivers as part of public reporting (see § 425.308) on the dedicated ACO Web page. Use of the waiver and its authorization by the governing body would be required to be documented, and the documentation retained, consistent with § 425.314. We would anticipate that any waiver would be effective on the start date of the ACO's participation agreement and would not extend beyond the end of the ACO's participation in the Shared Savings Program. However, if CMS terminates the participation agreement, then the waiver would end on the date of the termination notice. We also reserve the authority to withdraw the waiver in the event we determine that there has been an abuse of the waiver. The proposed payment waivers would not protect financial arrangements between ACOs, ACO participants, ACOs providers/suppliers, or other individuals or entities providing services to ACO patients from liability under the fraud and abuse laws or any other applicable laws.
We would retain the right to monitor and audit the use of such waivers. We would implement heightened monitoring of entities that bill under payment waivers to help reduce the possibility for abuse of the waiver. We seek comment on what specific activities should be monitored to ensure that items and services are properly delivered to eligible patients, and that patients are able to exercise freedom of choice and are not being steered inappropriately. We would also likely Start Printed Page 72826consider monitoring ACOs' marketing of services subject to payment waivers to prevent coercive or misleading marketing and to assess the effect on the delivery of care.
We seek comment on this potential approach to using our waiver authority to permit ACOs flexibility in specifying certain Medicare providers of post-hospital care services to patients and their families. We further seek comment on the criteria discussed above. Are there other cost and quality criteria that should be considered? Specifically to what hospitals and post-hospital providers should the waiver apply? For example, as discussed above, should the ability to recommend a post-hospital provider be available only to those hospitals that are ACO participants or ACO provider/suppliers, since these entities would have incentives that are most directly aligned with those of the ACO? Should a hospital be permitted to recommend any post-hospital provider or only post-hospital providers that are ACO participants or ACO provider/suppliers? We anticipate that if a waiver is found to be necessary, we would establish a waiver that would apply to all hospitals that are ACO participants or ACO providers/suppliers and that these hospitals would have the ability to recommend any post-hospital provider; however, we would be interested to receive comments on alternative approaches.
Overall, we are supportive of hospitals recommending certain post-hospital providers based on quality and a beneficiary's specific needs, as long as the beneficiaries understand their other options and retain their freedom of choice. In the event a waiver is found to be necessary, are there other parameters that should be established around how hospitals formulate their lists of post-acute providers and what information would be shared with beneficiaries? Under such a waiver would it be appropriate for hospitals to share only information on quality that is publically reported, such as on Home Health Compare, or would it be appropriate for hospitals to also share information that they have generated internally? We would be concerned if hospitals might steer beneficiaries to providers based on quality information that has not been properly vetted. Also, we would be concerned if hospitals recommended only their partnering providers, when there may be other providers of equal or better quality. Since the CoP requirements apply to all patients of a participating hospital regardless of their insurer or insured status, we are also seeking comment on whether it would be feasible to implement a system where the CoP requirement to not make recommendations is waived for the ACO participating hospitals only in the case of certain Medicare FFS beneficiaries. We are further seeking comments on whether it might be necessary for purposes of carrying out the Shared Savings Program and what benefits and risks might arise for non-Medicare inpatients if we were to waive this portion of the regulation for ACO participating hospitals with respect to all of their patients. We welcome comments on whether it would be appropriate to limit any such a waiver to ACOs participating under two-sided risk financial arrangements, or whether such a waiver should be available more broadly to all ACOs participating in the Shared Savings Program. Alternatively, should the waiver apply only to beneficiaries that are prospectively assigned to ACOs participating in Track 3? What operational considerations/concerns would implementation of such a waiver raise? What additional beneficiary protections and safeguards should be considered and put in place to prevent abuse of such a waiver?
(5) Waiver of Other Payment Rules
We welcome suggestions on whether there are any additional Medicare FFS payment rules that it may be necessary to waive using our authority under section 1899(f) of the Act in order to effectively implement two-sided risk financial arrangements under the Shared Savings Program by providing additional mechanisms for ACOs to increase quality and decrease costs. We would establish any such waivers through the rulemaking process. As a result, any suggestions submitted by commenters would be helpful to CMS in developing future proposals regarding the waiver of any Medicare FFS rules that might be necessary to carry out the provisions of the Shared Savings Program, and in particular to implement two-sided risk models under the program.
b. Other Options for Improving the Transition to Two-Sided Performance-Based Risk Arrangements
(1) Beneficiary Attestation
Under 1899(c) of the Act, beneficiaries are required to be assigned to an ACO participating in the Shared Savings Program based on the beneficiary's utilization of primary care services rendered by physicians. Thus, beneficiary choice, as indicated by their utilization of primary care service furnished by physicians, must determine beneficiary assignment to an ACO under the Shared Savings Program. Therefore, we developed a methodology for assigning beneficiaries based on whether the ACO provided the plurality of the beneficiary's primary care during a particular performance year. In the November 2011 final rule (76 FR 67851 through 67870), we outlined the major considerations in beneficiary assignment to an ACO.
First, we emphasized that unlike managed care programs, Medicare FFS beneficiaries do not enroll in the Shared Savings Program, and they retain the right to seek treatment from any Medicare-enrolled provider of their choosing. Thus, the “assignment” methodology in no way implies a lock-in or enrollment process. To the contrary, the statutory term “assignment” in this context refers only to an operational process by which we determine whether a beneficiary has chosen to receive a sufficient level of the requisite primary care services from a specific ACO so that the ACO may be appropriately designated as being accountable for that beneficiary's care, and we can measure its quality and financial performance on patients for whom it is in the best position to direct and influence their care. No exclusions or restrictions based on health conditions or similar factors are applied in the assignment of Medicare FFS beneficiaries.
Additionally, we noted that the statute requires that assignment be based on beneficiary utilization of primary care services furnished by physicians. We explored several options for assigning beneficiaries to an ACO based on whether the beneficiary received the plurality of primary care services from providers and suppliers participating in the ACO. The primary options we considered were whether to assign beneficiaries to an ACO prospectively, at the beginning of the performance year, or whether to assign beneficiaries to an ACO retrospectively, at the end of the performance year.
Under the retrospective approach, the ACO would be held accountable for beneficiaries that chose to receive the plurality of their primary care services from practitioners in the ACO during the course of the performance year. These beneficiaries necessarily would be identified at the end of the performance year. The advantage of this approach is that the ACO is assessed based on beneficiaries with whom its providers and suppliers had visits with during the performance year and had the greatest opportunity to impact care. Another advantage is that this methodology encourages organizations to improve care for all Medicare FFS Start Printed Page 72827patients seen by ACO professionals during a performance year. The disadvantage that some ACOs have articulated is that retrospective assignment can pose challenges when an organization has limited resources. Such organizations may prefer to target specific FFS beneficiaries for enhanced care improvement activities, and be confident that those specific beneficiaries will be the population used to determine the ACO's performance on cost and quality at the end of the year.
Under a prospective assignment approach, a beneficiary's utilization of primary care services during a timeframe prior to the start of the performance year would be used to assign a list of beneficiaries to the ACO at the beginning of a particular performance year (as we have proposed under Track 3). The total cost and quality of the care furnished to beneficiaries on the prospective assignment list would be used at the end of the performance year to determine the ACO's performance. As some ACOs have articulated, an advantage to this approach is that the organization can target its resources and care coordination activities to the specific FFS beneficiaries that appear on the prospective assignment list, confident that these are the beneficiaries that will determine the ACO's quality and efficiency performance at the end of the year. However, in the November 2011 final rule, we discussed several disadvantages to this approach. First, we believed that such an approach would erode the incentive for ACOs to improve their care processes to benefit the broader Medicare FFS population served by the ACO and its ACO participants and ACO providers/suppliers. We stated that since the goal of the Shared Savings Program is to change the care experience for all FFS beneficiaries, ACO participants and ACO provider/suppliers should have incentives to treat all patients equally; using standardized evidence-based care processes, to improve the quality and efficiency of the care they provide to all FFS beneficiaries (76 FR 67861). Second, we noted that since FFS beneficiaries retain the freedom to choose their providers, it was likely that some prospectively assigned beneficiaries would choose not to obtain the plurality of their primary care services from ACO professionals during the performance year; however, the ACO would still be held accountable for the total cost and quality of the care furnished to those beneficiaries.
After considering stakeholder comments on these main approaches, we finalized a hybrid policy that provided for a preliminary prospective assignment methodology with final retrospective reconciliation (76 FR 67867). We finalized this hybrid approach in an effort to realize the most positive aspects of both prospective and retrospective assignment and avoid, to the extent possible, the major disadvantages of each. Therefore, we finalized a policy in which we prospectively assign beneficiaries to ACOs in a preliminary manner at the beginning of a performance year based on most recent 12 months of data. We then update this information quarterly, based on a rolling 12 months of data. Final assignment is determined after the end of each performance year based on the 12 months of data from the performance year. This policy determines assignment to an ACO under the Shared Savings Program based on a statistical determination of a beneficiary's utilization of primary care services, rather than on a process of enrollment or “voluntary selection” by beneficiaries. Beneficiaries are assigned to no more than one ACO, and the specific methodology (the “step-wise” approach) is described in § 425.402. We finalized this policy because we believed that the methodology would balance beneficiary freedom to choose providers under FFS Medicare with the ACO's desire to have information about the FFS beneficiaries that were likely to be assigned at the end of the performance year. We also felt this approach would provide adequate incentives for each ACO to redesign care processes for and provide high quality care to its entire FFS beneficiary population instead of just focusing on a subset of patients. Finally, the ACO's performance would be assessed on the basis of the care furnished to those beneficiaries that chose to receive the plurality of primary care services from ACO professionals during the performance year, and for whom the ACO had the greatest opportunity to impact care.
A retrospective claims-based assignment methodology necessarily creates more year-to-year variability or “churn” in the list of assigned beneficiaries compared to managed care programs where patients enroll in and are locked in at the beginning of the year. Based on our experience and the data generated from the Physician Group Practice Demonstration (which used a similar retrospective assignment methodology), approximately 75 percent of beneficiaries assigned at the end of one performance year remained assigned at the end of the next performance year. The other 25 percent of beneficiaries were no longer assigned to the PGP site because they either were no longer eligible to be assigned or chose not to receive the plurality of their primary care services from the PGP practitioners. This statistic was recently confirmed when evaluating “churn” in the Shared Savings Program context. On average, 76 percent (range = 58 percent to 88 percent) of beneficiaries assigned to a Shared Savings Program ACO at the end of one year are assigned to the same ACO at the end of the subsequent performance year. In other words, ACOs experience a “churn rate” of 24 percent on average. However, when combined with the information provided on quarterly updates to the assigned beneficiary list, “churn” from quarter to quarter decreases to an average of 10 percent. In other words, on average, 91 percent of the beneficiaries assigned in one quarter appear on the next quarter's assignment list (range = 77 percent to 95 percent). These data indicate that “churn” varies from ACO to ACO, and that our hybrid assignment methodology performed according to expectations, that is, the quarterly assignment reports provide the ACO with relevant information during the performance year about its patient population for purposes of more effectively planning and coordinating care.
As in the PGP demonstration, the 24 percent “churn rate” found in the Shared Savings Program reflects beneficiaries that either became ineligible to be assigned or chose not to receive the plurality of their primary care services from ACO professionals. Beneficiaries who were assigned in one performance year, but fall off the assignment list at the end of the subsequent performance year may do so for a variety of reasons including:
- Beneficiary did not seek primary care services from any Medicare-enrolled physicians during the subsequent performance year.
- Beneficiary chose to receive all primary care services or the plurality of his or her primary care services from providers outside the ACO during the subsequent performance year. Reasons for this could include:
++ The beneficiary received short term care (for example, referral care, SNF care) from ACO professionals during the earlier performance year but did not continue the relationships in the subsequent year.
++ Beneficiary moved his/her residence and now seeks care from practitioners unaffiliated with the ACO.
- Beneficiary chose to enroll in MA or is otherwise no longer a FFS Medicare beneficiary in the subsequent Start Printed Page 72828performance year (that is, the beneficiary is no longer eligible for assignment).
- A new ACO entered the market in the subsequent performance year and its ACO professionals furnish the plurality of primary care services to the beneficiary compared to the established ACO.
We estimate that on average, 76 percent of beneficiaries assigned to a Shared Savings Program ACO remain assigned from one year to the next. However, the retention rate varies from 58 percent to 88 percent across ACOs, and correspondingly, the turnover varies from 12 percent to 42 percent. On average, 7 percent of previously assigned beneficiaries are no longer eligible for assignment to an ACO and 17 percent of previously assigned beneficiaries remain eligible to be assigned, but do not receive the plurality of their primary care services from ACO professionals the ACO during the subsequent performance year. Of the 17 percent of previously assigned beneficiaries who remain eligible for assignment—
- Six percent had at least one primary care physician visit with a physician who is an ACO professional, but the plurality of their primary care services were rendered outside the ACO;
- Three percent had no physician or non-physician primary care visits during the subsequent year;
- Seven percent had at least one physician or non-physician primary care visit, but none with ACO professionals;
- One percent had at least one non-physician primary care visit with an ACO professional, but had no primary care visits with physicians who are ACO professionals in the ACO; and
- Seven percent had at least one primary care visit with a physician in the ACO, but did not receive the plurality of their primary care services from ACO professionals.
As suggested by these statistics, some percentage of beneficiaries may believe a certain primary care practitioner affiliated with an ACO has ultimate responsibility for coordinating their care, even when it is necessary for them to receive primary care services from other practitioners, including practitioners who are not participating in the same ACO with which the practitioner is affiliated. Such a beneficiary could become unassigned if his or her primary care service utilization shifted away from practitioners in the ACO in a year. For example, a beneficiary living in a small town may have had a primary care service visit during a performance year with a primary care provider who is an ACO professional with whom the beneficiary has a long-standing relationship and the beneficiary believes this ACO professional is responsible for coordinating his/her care. If this beneficiary chooses to go to a large health system in the next town for primary care services and receives primary care services from practitioners that are unaffiliated with the ACO during the performance year, at the end of the performance year it may be determined that ACO professionals did not render the plurality of the primary care services for that beneficiary and therefore the ACO would not be held accountable for the total quality and cost of the beneficiary's care for that performance year. However, commenters have suggested that beneficiaries should have the ability to designate which providers (and by extension, the ACOs with which they are affiliated) are responsible for overseeing their overall care, regardless of where the beneficiary received the plurality of his or her primary care services. These commenters argue that creating a methodology that takes into account what provider a beneficiary believes has ultimate responsibility for his or her care could reduce “churn” from year to year, and increase the chances that an ACO would see a return on the investments it makes in the care of specific beneficiaries. Commenters argue this is particularly important in two-sided models where ACOs face amplified levels of performance-based risk.
Patient advocacy groups and ACOs have expressed interest in and support for enhancing claims-based assignment of beneficiaries to ACOs by taking into account beneficiary attestation regarding the provider that they consider to be responsible for coordinating their overall care. Stakeholders believe that incorporating this information and giving beneficiaries the opportunity to voluntarily “align” with the ACO in which their primary healthcare provider participates will improve the patient-centeredness of the assignment methodology.
To begin to address these concerns, the Pioneer ACO Model is currently conducting a test of beneficiary attestation for the 2015 performance year. Specifically, the Innovation Center has designed a test in which participating ACOs mail cover letters to beneficiaries aligned to the Pioneer ACO in either the 2013 or 2014 performance years, explaining the process by which a beneficiary may indicate whom they consider to be their “main doctor”, each with a form that asks the beneficiary to confirm their “main doctor”. In the form the beneficiary is asked to confirm whether or not the listed provider or supplier is their “main doctor.” Beneficiaries who confirm a care relationship with the provider/supplier listed on the form (who is an ACO participating provider/supplier identified by the Pioneer ACO) and meet all other eligibility criteria for alignment (or example, they did not drop either Part A or B coverage or join a MA plan), would be aligned to the Pioneer ACO for the following performance year, regardless of whether or not the practitioners participating in the Pioneer ACO rendered the plurality of the beneficiary's primary care services during the performance year. The Innovation Center will conduct claims-based attribution using the methodology established for the Pioneer ACO Model, but will include in the Pioneer's aligned beneficiary population not only those beneficiaries aligned through claims, but also those beneficiaries who returned the form confirming that a Pioneer ACO provider/supplier is their main doctor. Beneficiaries who do not return the form or who return the form, but indicate the provider listed is not their main doctor, will not be included in the ACO's assigned beneficiary population unless they are assigned through the existing claims-based attribution methodology. This means that if the beneficiary does not return the form and the beneficiary is not assigned to the Pioneer ACO through the claims-based attribution methodology, then the beneficiary would not be assigned to the Pioneer ACO.
Due to program integrity concerns and the additional administrative burden for ACOs participating in the Pioneer Model, discussions of beneficiary attestation or receipt of confirmation forms at the point of care were precluded under this first test of beneficiary attestation. Rather, in this initial test, the Innovation Center seeks only to evaluate the effectiveness of different types of mailed forms with respect to beneficiary willingness to attest that a particular practitioner has the primary responsibility for their care. Additional testing in the future is planned under the Pioneer ACO Model that will build upon lessons learned from this initial test and in which we would seek to enhance the meaningfulness of dialogue between beneficiaries and their providers regarding the nature of the care relationship.
Although we are not making any specific proposals related to beneficiary attestation, we welcome comments on Start Printed Page 72829whether it would be appropriate to offer a beneficiary attestation process to ACOs that choose to participate in the Shared Savings Program under two-sided risk financial arrangements. We intend to carefully consider any comments on this issue during the development of the final rule, and will make an assessment at that time as to whether any change to our assignment methodology to include beneficiary attestation would be appropriate. We are interested in receiving comments and suggestions on a wide variety of policy and operational issues related to beneficiary attestation. For example, which beneficiaries should be eligible to attest into an ACO? Should this option be available to all beneficiaries or only to currently or previously aligned beneficiaries? What implications would attestation or voluntary alignment have for the assignment of beneficiaries to an ACO under a prospective versus a preliminary prospective method? Which types of care relationships should be considered—those with primary care physicians, specialists or other types of providers? How should beneficiaries receive communications about claims-based and voluntary alignment and who would provide the information? What method or process should be used to obtain beneficiary confirmation and when would this occur? Under what circumstances and how could beneficiaries reverse their decisions? Although we believe the option suggested would protect beneficiary freedom to choose, we seek comment on whether there are additional ways to protect beneficiaries from coercion and ensure proper monitoring and safeguards under the Shared Savings Program. What implications would there be for ACO information or other administrative systems? What provider education would be needed? Should there be additional application or eligibility requirements for ACOs in tracks under which beneficiary attestation is offered? We would note that if we were to offer a beneficiary attestation process for ACOs that choose to participate in the Shared Savings Program under two-sided risk financial arrangements, such beneficiaries would be eligible to be included in the sample for GPRO quality reporting by ACOs participating in the Shared Savings Program (76 FR 67900), even if the beneficiary did not chose to receive care from the ACO professionals during the performance year, as might be the case under Track 3 under the proposed prospective assignment methodology. Also, we are concerned about creating additional administrative burdens for ACOs that might discourage them from accepting two-sided risk arrangements. Are there ways that beneficiary attestation could be operationally implemented to reduce administrative burdens on ACOs and CMS and limit beneficiary confusion? We anticipate that if we were to offer a beneficiary attestation process for ACOs that choose to participate in the Shared Savings Program under two-sided risk financial arrangements, then at least initially we would anticipate implementing this beneficiary attestation in a manner consistent with the current beneficiary attestation under the Pioneer ACO Model. We believe this would be an appropriate starting point for beneficiary attestation under the Shared Savings Program because it allows us to take advantage of the policies and processes that have already been developed for the Pioneer ACO Model. Additionally, we believe it is unlikely that such a policy would impact “churn” for Track 3 ACOs during a performance year, given our proposals for prospectively assigning beneficiaries. However, beneficiary attestation may have a minor impact on “churn” during a performance year related to the preliminary prospective with retrospective reconciliation approach such as the methodology employed under Track 2. This process may also have a minor impact in stabilizing the beneficiary assignment list from one performance year to the next for all ACOs.
In addition, we seek comments on whether a beneficiary attestation process under the Shared Savings Program could bias performance year results compared to the ACO's benchmark. For example, we believe that such biases could occur because the beneficiaries used to establish performance benchmarks would not have had the same opportunity to designate their “main doctor.” Rather, for purposes of the benchmark years, all beneficiaries would be assigned using the established claims-based assignment methodology. Would it be appropriate for us to use our authority to adjust an ACO's benchmark to account for “beneficiary characteristics” to address any such potential biases?
In connection with any implementation of beneficiary attestation, we would revise our regulations as necessary, to protect beneficiaries from undue coercion or influence in connection with whether they choose to attest or not. Beneficiary attestation is not intended to be used as a mechanism for ACOs (or ACO participants, ACO providers/suppliers, ACO professionals, or others) to target potentially lucrative beneficiaries or avoid those less likely to produce savings. To this end, we do not believe ACOs or others should be permitted to offer gifts or other inducements to beneficiaries, nor should they be allowed to withhold or threaten to withhold items or services, for the purpose of coercing or influencing their alignment decisions. The current regulations at § 425.304(a)(1) prohibit ACOs, ACO participants, ACO providers/suppliers, and other individuals or entities performing functions or services related to ACO activities from providing gifts or other remuneration to beneficiaries as inducements for receiving items or services from, or remaining in, an ACO. The regulation at § 425.304(a)(2) permits certain in-kind items or services to be provided to beneficiaries if there is a reasonable connection between the items and services and the medical care of the beneficiary and certain other conditions are met. We would consider any inducement intended to coerce or influence a beneficiary attestation decision to be prohibited under § 425.304(a)(1) and not be considered reasonably connected to medical care under § 425.304(a)(2). We would not, however, prohibit an ACO or its ACO participants and ACO providers/suppliers from providing a beneficiary with accurate descriptive information about the potential patient care benefits of aligning with an ACO. We are also soliciting comments on this issue.
(2) Seeking Comment on a Step-Wise Progression for ACOs To Take on Performance-Based Risk
Under the current Shared Savings Program rules, an ACO may not include an entity on its list of ACO participants unless all ACO providers/suppliers billing through the entity's Medicare-enrolled TIN have agreed to participate in the program and comply with the program rules (see discussion in section II.B. of this proposed rule). Furthermore, it is not possible under our current regulations for some ACO providers/suppliers to participate in Track 1, while other ACO providers/suppliers that may be more ready to accept performance-based risk participate under Track 2. Some stakeholders have commented that requiring all ACO providers/suppliers billing through an ACO participant TIN to participate in the same risk track could deter some ACOs from entering higher risk arrangements (Tracks 2 or 3) if they do not believe that all of the ACO providers/suppliers billing through a given ACO participant TIN are prepared to operate under high levels of risk. Start Printed Page 72830Conversely, we have heard from other stakeholders that requiring all ACO providers/suppliers billing though an ACO participant TIN to enter the same risk track can motivate an organization to work toward a common performance goal and implement uniform care processes that streamline patient care within and between various sites of care. We believe that the program works best when the incentives within an organization are aligned among all providers and suppliers in that organization. Given our policy objectives to encourage ACOs to redesign their care processes and move to increasing levels of financial risk, we are not proposing at this time to change our regulations in order to allow providers and suppliers billing through the same ACO participant TIN to participate in different tracks under the Shared Savings Program. However, we are interested in stakeholder opinion on this issue and seek comment on what options the program might consider in the future to encourage organizations to participate in the program while permitting the providers and suppliers within that organization to accept varying degrees of risk. In particular, we are interested in stakeholders' input on the advantages and disadvantages of allowing Shared Savings Program ACOs that wish to enter a track with increased risk to split their ACO participants into different tracks or split ACO provider/suppliers billing through a given Medicare-enrolled TIN so that a subset participate in a track that offers a higher sharing rate in exchange for taking on a greater degree of performance-based risk, while the remainder participate in a lower risk track. We intend to carefully review any comments that are received on these issues during the development of the final rule and will make an assessment at that time as to whether any change to our current policy is necessary and appropriate.
For reasons already stated in the November 2011 final rule (76 FR 67808 through 67811), we believe it is appropriate to use the Medicare-enrolled TINs that make up each ACO as the basis for a number of operational processes under the Shared Savings Program, including beneficiary assignment, and that, as a result, all providers and suppliers billing through the TIN of an ACO participant must agree to participate in the ACO and comply with program regulations in order for the ACO to include the entity on its ACO participant list. Therefore, we do not believe it would be necessary or ideal to adopt an approach under which ACOs would be permitted to pick and choose ACO provider/suppliers for participation. However, we are considering ways to encourage organizations to move in a step-wise progression to taking on performance-based risk when some entities on its ACO participant list are ready. Therefore, if we were to make modifications to our current policies to permit organizations to split their ACO participant TIN list into different risk tracks, we would anticipate the following:
- The ACO must have completed a full agreement period under Track 1 and meet requirements for renewing its agreement under Track 1 as proposed in this proposed rule.
- The ACO must submit an ACO participant list in the form and manner designated by CMS and by a deadline established by us.
- The ACO must indicate, in the form and manner specified by CMS, which ACO participants would continue under Track 1 and which would participate under a performance-based risk track. We would consider this list to be a “segmented list” of ACO participants.
- The ACO as a whole would be required to meet the eligibility requirements to participate in the program, including the requirement that the ACO have at least 5,000 assigned beneficiaries and the governance requirements.
- Regarding quality measures submission, we considered whether the ACO as a whole would be responsible for submitting quality data in accordance with subpart F of the Shared Savings Program regulations. On the one hand, the ability of the ACO to report quality measures once on behalf of both segmented lists would reduce quality reporting burden with the same aggregate quality score applying to each segment of the ACO participants. On the other hand, if each segmented list was required to report quality separately, we may be able to get a more accurate assessment of the quality of care by each segmented list leading to a more accurate determination of shared savings or losses.
- Regarding benchmarking and assignment of beneficiaries, we considered whether each half of the segmented list of ACO participants would have its own benchmark and list of assigned beneficiaries. Under this option, the two groups of ACO participants would each receive their own performance reports from CMS and be subject to the data sharing rules appropriate for their track, and the determination of shared savings would occur according to the rules of the chosen track. Another option would be to develop one benchmark and list of assigned beneficiaries for the ACO as a whole. This option would require a uniform assignment methodology to be applied, regardless in which track the segmented lists are participating. Alternatively, we could limit segmented lists to participation in only Tracks 1 and 2 because these tracks have an assignment methodology that does not conflict.
- Regarding changes in the ACO participant lists during the agreement period, we considered whether an ACO would be permitted to add or delete ACO participants from the segmented list of ACO participants. One option considered would be to permit an ACO to add or delete ACO participants from the segmented lists pursuant to the proposed regulation at § 425.118(b), but ACO participants would not be permitted to change risk tracks during the agreement period. Another option we considered and seek specific comments on is the option to require such organizations to articulate and carry out the transition of their Track 1 ACO participants to the list of ACO participants that are under a risk-based arrangement during the course of the agreement period. For example, in each year of the agreement period, the ACO would be required to remove ACO participants from the Track 1 list and add them to the list of ACO participants under the two-sided risk model. In this way, the ACO and its ACO participants would be better prepared to reapply to the Shared Savings Program under a two-sided risk model in its third agreement period.
Although we are not specifically proposing to allow for different risk tracks within the same ACO, we seek comments on these options and other considerations for permitting organizations to move forward to performance-based risk in a step-wise manner. We specifically seek comment on ways to mitigate selection bias when considering these options, in other words, we seek comment on whether additional considerations should be made with regards to organizations that may choose to create two different ACO participant lists in an effort to advantage the part of the organization that is participating in the two-sided model at the expense of the part of the organization participating in the one-sided model. We believe the concern is minimized by the option we considered that we would only make this option available under an ACO's second agreement period. Moreover, we note that our proposed criteria for renewal include a review of the ACO's history of program integrity. We intend to Start Printed Page 72831carefully review any comments that are received on these issues during the development of the final rule and will make an assessment at that time as to whether any change to our current policy is necessary and appropriate.
5. Modifications to Repayment Mechanism Requirements
a. Overview
In the November 2011 final rule (76 FR 67937), we discussed the importance of a program requirement that ensures ACOs entering the two-sided model will be capable of repaying Medicare for shared losses. The final rule established a requirement that ACOs applying to participate in the two-sided model must establish a repayment mechanism to assure CMS that they can repay losses for which they may be liable (§ 425.204(f)). For an ACO's first performance year, the repayment mechanism must be equal to at least 1 percent of its total per capita Medicare Parts A and B FFS expenditures for its assigned beneficiaries, as determined based on expenditures used to establish the ACO's benchmark (§ 425.204(f)).
Further, to continue participation in the program, each Track 2 ACO must annually demonstrate the adequacy of its repayment mechanism before the start of each performance year in which it takes risk (§ 425.204(f)(3)). The repayment mechanism for each performance year must be equal to at least 1 percent of the ACO's total per capita Medicare Parts A and B FFS expenditures for its assigned beneficiaries, as determined based on expenditures for the ACO's most recent performance year.
An ACO may demonstrate its ability to repay losses, or other monies determined to be owed upon first year reconciliation, by obtaining reinsurance, placing funds in escrow, obtaining surety bonds, establishing a line of credit (as evidenced by a letter of credit that the Medicare program can draw upon), or establishing another appropriate repayment mechanism that will ensure its ability to repay the Medicare program (§ 425.204(f)(2)). Given our experience in implementing the program, we are proposing to revisit our requirements to simplify them and to address stakeholder concerns regarding the transition to risk, as discussed in the previous sections.
b. Proposals for Amount and Duration of the Repayment Mechanism
As noted previously, under the current regulations, ACOs entering a two-sided risk track must submit an adequate repayment mechanism at the time of application and again at the beginning of each performance year. The amount must be equal to at least 1 percent of the ACO's total per capita Medicare Parts A and B FFS expenditures for its assigned beneficiaries, as determined based either on expenditures used to establish the ACO's benchmark or expenditures for the ACO's most recent performance year. This amount is estimated by CMS and reported to the ACO so that it can set up its required mechanism. We have heard from stakeholders that establishing multiple repayment mechanisms during the agreement period can be very burdensome and ties up capital that could otherwise be used to support ACO operations. Therefore, we have considered whether it would be possible to streamline the repayment mechanism requirements. Specifically, we considered whether it would be feasible for an organization to establish a single repayment mechanism to cover the entire 3-year agreement period. Initially we were concerned that requiring an organization to establish a single repayment mechanism to cover 3 performance years would involve repayment amounts that were excessive and overly burdensome for organizations. However, our actuaries have determined that this may not be the case. We believe that rather than requiring ACOs to create and maintain two separate repayment mechanisms for two consecutive performance years, which would effectively double the amount of the repayment mechanism during the overlapping time period between the start of a new performance year and settlement of the previous performance year, the repayment mechanism that is established for the first performance year of an agreement period under a two-sided risk model can be rolled over for subsequent performance years.
Thus, we propose to require an ACO to demonstrate at the time of its application to the Shared Savings Program or participation agreement renewal for a two-sided risk model and upon request thereafter that it would be able to repay shared losses incurred at any time within the agreement period, that is, upon each performance year reconciliation during the agreement period. Thus, an ACO would be required to establish a repayment mechanism for the required amount as discussed in this section to cover the entire agreement period under a two-sided risk model (that is, under Track 2 or under proposed Track 3) and a reasonable period of time after the end of the agreement period (the “tail period”). The tail period shall be sufficient to permit CMS to calculate the amount of any shared losses that may be owed by the ACO and to collect this amount from the ACO. The length of the tail period shall be established by CMS in guidance.
Under this approach, an ACO would be required to establish a repayment mechanism once at the beginning of a 3-year agreement period. We propose that an ACO must demonstrate the adequacy of its repayment mechanism and maintain the ability to repay 1 percent of the ACO's total per capita Medicare Parts A and B FFS expenditures for its assigned beneficiaries based on the expenditures used to establish the benchmark for the applicable agreement period, as estimated by CMS at the time of application or participation agreement renewal. If the repayment mechanism is used to repay any portion of shared losses owed to CMS, the ACO must promptly replenish the amount of funds available through the repayment mechanism within 60 days. This would ensure continued availability of funds to cover any shared losses generated in subsequent performance years. Given that we propose in section II.B. of this proposed rule to adjust an ACO's benchmark annually to account for changes in the ACO participant list, it is possible that an ACO's benchmark could change such that the repayment mechanism amount established at the beginning of the 3-year agreement period no longer represents one percent of the ACO's benchmark expenditures. Therefore, we are considering whether we should require the ACO to adjust the repayment mechanism to account for this change, or whether a threshold should be established that triggers a requirement for the ACO to add to its repayment mechanism. We seek comment on this issue, including the appropriate threshold that should trigger a requirement that the ACO increase the amount guaranteed by the repayment mechanism.
These proposals are reflected in the proposed modifications to § 425.204(f). We note that the reference to “other monies determined to be owed” in the current provision directly relates to the interim payments that were available in the first performance year only for ACOs that started participating in the program in 2012. Because interim payments are no longer offered to ACOs, we also propose to remove the reference to “other monies determined to be owed” from § 425.204(f).Start Printed Page 72832
c. Proposals Regarding Permissible Repayment Mechanisms
Under our current rules, ACOs may demonstrate their ability to repay shared losses by obtaining reinsurance, placing funds in escrow, obtaining surety bonds, establishing a line of credit (as evidenced by a letter of credit that the Medicare program can draw upon), or establishing another appropriate repayment mechanism that will ensure their ability to repay the Medicare program. Based on our experience with the program, we are proposing to remove the option that permits ACOs to demonstrate their ability to pay using reinsurance or an alternative mechanism. First, no Shared Savings Program ACOs have obtained reinsurance for the purpose of establishing their repayment mechanism. ACOs that have explored this option have told us that it is difficult to obtain reinsurance, in part, because of insurers' lack of experience with the Shared Savings Program and the ACO model, and because Shared Savings Program ACOs take on performance-based risk not insurance risk. Additionally, the terms of reinsurance policies obtained by ACOs could vary greatly and prove difficult for CMS to effectively evaluate. Second, based on our experience to date, a request to use an alternative repayment mechanism increases administrative complexity for both ACOs and CMS during the application process and is more likely to be rejected by CMS than one of the specified repayment mechanisms.
Therefore, we propose to revise § 425.204(f)(2) to limit the types of repayment mechanisms ACOs may use to demonstrate their ability to repay shared losses to the following: Placing funds in escrow; establishing a line of credit; or obtaining a surety bond. Under this proposed revision, ACOs would retain the flexibility to choose a repayment mechanism that best suits their organization. We also believe that CMS would be more readily able to evaluate the adequacy of these three types of arrangements, as compared to reinsurance policies and other alternative repayment mechanisms. For instance, escrow account agreements, letters of credit, and surety bonds typically have standard terms, that CMS can more readily assess as compared to the documentation for alternative repayment mechanisms, which tends to be highly variable.
In addition, we propose to clarify that ACOs may use a combination of the designated repayment mechanisms, if needed, such as placing certain funds in escrow, obtaining a surety bond for a portion of remaining funds, and establishing a line of credit for the remainder. Thus, we are proposing to revise our rule at § 425.204(f)(2) to indicate that an ACO may demonstrate its ability to repay shared losses owed by placing funds in escrow, obtaining surety bonds, establishing a line of credit, or by using a combination of these mechanisms. We seek comment on our proposed modifications to the repayment mechanism requirements and also welcome comments on the availability and adequacy of reinsurance as a repayment mechanism.
6. Seeking Comment on Methodology for Establishing, Updating, and Resetting the Benchmark
a. Background on Establishing, Updating, and Resetting the Benchmark
Section 1899(d)(1)(B)(ii) of the Act addresses how ACO benchmarks are to be established and updated. This provision specifies that the Secretary shall estimate a benchmark for each agreement period for each ACO using the most recent available 3 years of per beneficiary expenditures for parts A and B services for Medicare FFS beneficiaries assigned to the ACO. Such benchmark shall be adjusted for beneficiary characteristics and such other factors as the Secretary determines appropriate and updated by the projected absolute amount of growth in national per capita expenditures for parts A and B services under the original Medicare fee-for-service program, as estimated by the Secretary. Such benchmark shall be reset at the start of each agreement period. Accordingly, through the initial rulemaking establishing the Shared Savings Program, we adopted policies for establishing, updating and resetting ACO benchmarks at § 425.602. As described later in this section, under this methodology, we establish ACO-specific benchmarks that account for national FFS trends.
As the statute requires the use of historical expenditures to establish an ACO's benchmark, the per capita costs for each benchmark year must be trended forward to current year dollars and then a weighted average is used to obtain the ACO's historical benchmark for the first agreement period. The statute further requires that we update the benchmark for each year of the agreement period based on the projected absolute amount of growth in national per capita expenditures for parts A and B services under the FFS program, as estimated by the Secretary. In the April 2011 proposed rule (76 FR 19609 through 19611), we considered a variety of options for establishing the trend factors used in establishing the historical benchmark and for accounting for FFS trends in updating the benchmark during the agreement period.
In addition to the statutory benchmarking methodology established in section 1899(d), section 1899(i)(3) of the Act grants the Secretary the authority to use other payment models, including payment models that would use alternative benchmarking methodologies, if the Secretary determines that doing so would improve the quality and efficiency of items and services furnished under this title and the alternative methodology would result in program expenditures equal to or lower than those that would result under the statutory payment model. As described later in this section, in the November 2011 final rule, we considered whether to invoke this authority to modify certain aspects of the statutory benchmarking methodology, but elected not to do so. We note that we did invoke this authority to help create two-sided risk under Track 2.
(1) Background on Use of National Growth Rate as a Benchmark Trending Factor
The statute does not specify the trending factor to be used in establishing the benchmark. In the April 2011 proposed rule (76 FR 19610), we considered use of either national, or state or local growth factors for trending the benchmark. We explained that using the national growth rate in Medicare A and B FFS expenditures appeared to be more consistent with the statutory methodology for updating an ACO's benchmark. Further, a national growth rate would allow a single growth factor to be applied to all ACOs regardless of their size or geographic area. However, a national rate could also disproportionately encourage the development of ACOs in areas with historical growth rates below the national average that would benefit from having a relatively higher base, which increases the chances for shared savings, while discouraging the development of ACOs in areas with historically higher growth rates above the national average that would have a relatively lower base.
In contrast, we explained in April 2011 proposed rule that trending expenditures based on State or local area growth rates in Medicare A and B expenditures may more accurately reflect the experience in an ACO's area and mitigate differential incentives for Start Printed Page 72833participation based on location. Therefore, we considered an option to trend the benchmark by the lower of the national projected growth rate or the State or the local growth rate. This option balanced providing a more accurate reflection of local experience with not rewarding historical growth higher than the national average. We believed this method would instill strong saving incentives for ACOs in both high-cost growth and low-cost growth areas.
We proposed to employ the national growth rate in Medicare Parts A and B expenditures for FFS beneficiaries for trending forward the most recent 3 years of per beneficiary expenditures for Parts A and B services in order to establish the historical benchmark for each ACO. We believed this approach would help to ensure that ACOs in both high spending, high growth and low spending, low growth areas would have appropriate incentives to participate in the Shared Savings Program. We further indicated that this approach would allow us to move toward establishing a national standard to calculate and measure ACO financial performance. We sought comment on this proposal and on the alternatives to using a national growth rate to establish the benchmark.
Some commenters supported our proposal to employ a national growth rate for setting the benchmark and recognized the importance of using national growth rates for rationalizing overall spending across regions nationwide. Many more favored the use of either local, regional, or State growth rates, and some favored our proposal to use the lower of either the national or State or local growth rates. Commenters also offered a number of alternative approaches for trending benchmark expenditures, including the following:
- Use a blend of national average growth and absolute dollar growth.
- Use the ACO's own percentage growth rate to trend forward the historical benchmark data.
- Account for local variation after analyzing national and local growth rates. (76 FR 67925).
In the end, we finalized our policy under § 425.602 of using the national growth rate in Medicare Parts A and B expenditures for FFS beneficiaries for trending forward the most recent 3 years of per beneficiary expenditures for Parts A and B services in order to establish the benchmark for each ACO. In doing so, we make calculations for separate cost categories for each of the following populations of beneficiaries: ESRD, disabled, aged/dual eligible and aged/non-dual eligible. We stated our belief that implementing a historical benchmark trending factor using the national growth rate for Parts A and B FFS expenditures appropriately balanced commenters' concerns that benchmark trending should encourage participation among providers that are already efficient or operating in low cost regions without unduly rewarding ACOs in high-cost areas. We further stated that we anticipated the net effect of using the same trending factor for all ACOs would be to provide a relatively higher expenditure benchmark for low-growth/low spending ACOs and a relatively lower benchmark for high growth/high spending ACOs. ACOs in high cost, high growth areas would therefore have an incentive to reduce their rate of growth more to bring their costs more in line with the national average; while ACOs in low cost low, growth areas would have an incentive to continue to maintain or improve their overall lower spending levels.
Over 330 ACOs entered the Shared Savings Program between 2012 and 2014 and are located throughout the country—across diverse geographies—in a mix of high-cost/high-growth and low-cost/low-growth areas. Further, within local markets where multiple ACOs have formed, we have observed that ACOs can be a mix of both high- and low-cost and high- and low-growth organizations. We are encouraged by the continued interest in the program: Of the ACOs that entered the program, only two voluntarily terminated at the end of the performance year concluding December 31, 2013. (One was eligible for a performance payment of shared savings and the other merged with another participating ACO.) In addition, we continue to see strong interest in new entrants for the January 2015 start date.
Under the Pioneer ACO model, we adopted a different methodology for establishing an ACO's historical expenditure baseline for its first three performance years. See http://innovation.cms.gov/Files/x/PioneerACOBmarkMethodology.pdf. The Pioneer model benchmarking methodology trends forward baseline years 2009 and 2010 to 2011 by applying the growth in expenditures for the reference population. The reference population is defined as alignment-eligible beneficiaries with the same state of residence, eligibility status, age and sex as the ACO's aligned beneficiaries. The 3 historical baseline years under the Pioneer ACO Model also correspond to the 3 years prior to when ACOs entered the model, specifically 2009, 2010, and 2011. Further, baseline expenditures in 2011 dollars are updated to the appropriate performance year using a 50/50 blend of the national growth rate and the absolute dollar equivalent of that national growth rate. However, the benchmarking methodology used in the Pioneer ACO Model was revised for performance years four and five of the model to be more consistent with the benchmarking approach used in the Shared Savings Program, in part due to stakeholder feedback.
(2) Background on Use of National FFS Growth Factors in Updating the Benchmark During the Agreement Period
Section 1899(d)(1)(B)(ii) of the Act states that the benchmark shall be updated by the projected absolute amount of growth in national per capita expenditures for parts A and B services under the original Medicare fee-for-service program, as estimated by the Secretary.
In the April 2011 proposed rule (76 FR 19610 through 19611), we proposed to use a flat dollar amount equivalent of the absolute amount of growth in the national FFS expenditures to update the benchmark during an agreement period. We explained our view that in enacting section 1899(d)(1)(B)(ii) of the Act, Congress demonstrated interest in mitigating some of the regional differences in Medicare spending among ACOs and that this approach would help to ensure that ACOs in both high spending/high growth and low spending/low growth areas would have appropriate incentives to participate in the Shared Savings Program. We described the effect this update methodology might have in the 2nd and 3rd years of an agreement period: Using a flat dollar increase, which would be the same for all ACOs, provides a relatively higher expenditure benchmark for low growth, low spending ACOs and a relatively lower benchmark for high growth, high spending ACOs. All else being equal, an ACO can more likely share in savings when its actual expenditures are judged against a higher, rather than a lower benchmark. Thus, with a flat dollar increase to the benchmark, ACOs in high cost/high growth areas must reduce their rate of growth more to bring their costs more in line with the national average. We acknowledged that this approach to updating the benchmark could contribute to selective program participation by participants in low growth areas, as well as result in Medicare costs due to an increase in the amount of performance payments for unearned savings.
We also considered and sought comment on a second option, which Start Printed Page 72834would be to use our authority under section 1899(i)(3) of the Act to update the benchmark by the lower of the national projected absolute amount of growth in national per capita expenditures or the local/State projected absolute amount of growth in per capita expenditures. We explained our belief that this option could instill strong saving incentives for ACOs in low-cost areas, as well as for those in high-cost areas. Incorporating more localized growth factors reflects the expenditure and growth patterns within the geographic area served by ACO participants, potentially providing a more accurate estimate of the updated benchmark based on the area from which the ACO derives its patient population. Capping the update at the projected absolute amount of growth in national per capita expenditures, however, can advantage ACOs in low cost/low growth areas that have already achieved greater efficiencies, while still offering a strong incentive for those in high cost/high growth areas to reduce their spending.
Commenters were mixed in their preference for either the proposed policy of updating the benchmark by absolute growth in national FFS expenditures, or use of the lower of the national projected absolute amount or the local/State projected absolute amount. For example, one commenter disagreed with the option to use the lower of the national projected absolute amount or the local/State projected absolute amount, suggesting it negatively prejudges all high growth sectors without regard to the underlying clinical or quality issues. However, another commenter favored this approach because this adjustment would afford ACOs the greatest potential for achieving shared savings and minimize the threat of an ACO being disadvantaged by virtue of pricing within its geographic location. Along these lines, one commenter stated the proposed approach offered insufficient incentives for efficient providers to form an ACO. More generally, many commenters urged CMS to adopt policies to encourage participation by organizations that are already efficient or in low cost areas. Several commenters urged use of regional or market-specific expense data for calculating the benchmark update.
In the November 2011 final rule (76 FR 67926 through 67927), we finalized a policy of using the flat dollar amount equivalent of the projected absolute amount of growth in national per capita FFS expenditures to update the benchmark. We stated our belief that this method for updating the benchmark could best address the program's goals and commenters' overall concerns about the participation of efficient/low cost ACOs. The net effect of using the same update for all ACOs is to provide a relatively higher expenditure benchmark for low growth/low spending ACOs and a relatively lower benchmark for high growth/high spending ACOs. Further, with a flat dollar increase to the benchmark equivalent to the absolute amount of growth in the national FFS expenditures, ACOs in high cost, high growth areas must reduce their rate of growth more (compared to ACOs in low cost, low growth areas) to bring their costs in line with the national average. We stated that in light of the alternatives we considered, we believed that the policy of updating benchmarks by the absolute amount of growth in national FFS expenditures offers sufficient incentives for efficient providers to form ACOs. Thus, under the final update methodology, ACOs in low cost areas would achieve a greater amount of savings, based on the same performance, than a comparable ACO in a higher cost area. Moreover, we stated we believed that a benchmark methodology that encourages providers in higher cost areas to bring their spending more in line with the national average is a desirable outcome in furtherance of the program's goal of lowering Medicare expenditures. Finally, we noted that updating the benchmark during the agreement period using a national growth factor aligns with our approach of using a national growth rate to trend forward base year expenditures when establishing the historical benchmark. We stated that we believed this alignment could facilitate analysis of trends in ACO financial performance relative to national trends in Medicare expenditures. For these reasons, we finalized a policy of using the flat dollar amount equivalent of the projected absolute amount of growth in national FFS expenditures to update the benchmark.
In applying these policies for ACOs that joined the program in 2012 and 2013, we observed that the national growth factors used to trend the historical benchmark were declining, highlighted by negative annual per capita expenditure growth in three of four Medicare eligibility categories in 2012. We also found during the first performance year reconciliation that the national update amounts applied to the historical benchmark continued to reflect historically low growth in cost even after an adjustment to restore the effect of sequestration on 2013 claim payments. These updates reflected the slow or negative FFS growth environment due to a number of factors, including demographic changes in program enrollment, low price updates for physician, skilled nursing, and other services, and a broad decrease in inpatient utilization. This resulted in ACOs having very low or even negative updates to their historical benchmarks. Recent projections estimate total Medicare per capita expenditure trends are likely to remain historically low through 2015 followed by a gradual return to historically-familiar positive trend rates starting in 2016.
(3) Background on Managing Changes to ACOs During the Agreement Period
Section 425.214 of the Shared Savings Program regulations addresses the circumstance under which an ACO adds or removes ACO participants or ACO providers/suppliers (identified by TINs and NPIs, respectively) during the term of the participation agreement. The regulation specifies that the ACO's benchmark, risk scores, and preliminary prospective assignment may be adjusted for this change at CMS' discretion (§ 425.214(a)(3)). Subregulatory guidance further describes our use of this discretion. See “Changes in ACO participants and ACO providers/suppliers during the Agreement Period” available online at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Updating-ACO-Participant-List.html. This guidance explains:
After acceptance into the program and upon execution of the participation agreement with CMS, the ACO must certify the completeness and accuracy of its list of ACO participants. We set the ACO's historical benchmark at the start of the agreement period based on the assigned population in each of the three benchmark years by using the ACO Participant List certified by the ACO. The ACO must submit a new certified ACO Participant List at the start of each new performance year.
CMS will adjust the ACO's historical benchmark at the start of a performance year if the ACO Participant List that the ACO certified at the start of that performance year differs from the one it certified at the start of the prior performance year. CMS will use the updated certified ACO Participant List to assign beneficiaries to the ACO in the benchmark period (the 3 years prior to the start of the ACO's agreement period) in order to determine the ACO's adjusted historical benchmark. As a result of changes to the ACO's certified ACO Participant List, we may adjust the historical benchmark upward or downward. We'll use the new certified list of ACO participants and the adjusted benchmark for the new performance year's assignment, quality measurement and sampling, reports for the new performance Start Printed Page 72835year, and financial reconciliation. We will provide ACOs with the adjusted Historical Benchmark Report.
During the program's first performance years, we experienced a high volume of change requests from ACOs, both adding and removing ACO participants. For example, cumulatively ACOs with 2012 and 2013 start dates requested the addition of over 2,800 ACO participants and removal of over 1,200 ACO participants. The ACO's composition of ACO participant TINs is used to determine the ACO's assigned beneficiary population. Changes to an ACO's participant list will result in changes to the ACO's assigned beneficiary population. As a result, it is necessary to make adjustments to the ACO's historical benchmark to account for these changes. In accordance with our guidance, we adjusted the historical benchmarks for 162 of 220 ACOs with 2012 and 2013 start dates for their second performance year to reflect changes in ACO participants. When an ACO adds new ACO participants or deletes existing ACO participants, the adjustments that are made to its historical benchmark will impact the ACO's performance in subsequent years, and can make forecasting performance more challenging.
As noted in the guidance, when we adjust historical benchmarks during the agreement period to account for changes in beneficiary assignment arising from ACO participant list changes, the benchmark period (the 3 years prior to the start of the ACO's agreement period) remains the same. For instance, if an ACO with an agreement start date of January 1, 2013, added ACO participants for its second performance year, then the adjustments made to the historical benchmark to reflect the ACO's certified ACO participant list for performance year 2 would have been based on the same three benchmark years (2010, 2011, and 2012) originally used to calculate the historical benchmark for the ACO based on its ACO participant list certified when it entered the program (for its first performance year).
Further, changes in the ACO participant TINs that compose ACOs are relevant to determining beneficiary assignment across the program. A beneficiary is assigned to an ACO if the beneficiary received the plurality of his or her primary care services (measured in allowed charges) from ACO professionals billing under the TINs of ACO participants in the ACO rather than outside the ACO (such as from ACO professionals billing under the TINs of ACO participants in other ACOs, individual providers, or provider organizations). We perform the assignment process for ACOs simultaneously, including all eligible organizations. To determine where a beneficiary got the plurality of his or her primary care services, we compare the total allowed charges for each beneficiary for primary care services provided by the ACO (in total for all ACO participants) to the allowed charges for primary care services provided by ACO participants in other ACOs and by non-ACO providers and suppliers. See “Medicare Shared Savings Program: Shared Savings and Losses and Assignment Methodology Specifications” available online at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Financial-and-Assignment-Specifications.html. Therefore, in the case where a beneficiary is receiving primary care services from ACO participants in multiple ACOs or from both ACO participants and non-ACO providers and suppliers, an ACO's participant composition is important in determining whether the beneficiary is assigned to the ACO at all, and in determining to which (among several) ACO the beneficiary may be assigned.
In summary, in making adjustments to the historical benchmarks for ACOs within an agreement period to account for ACO participant list changes: The historical benchmark period remains constant, but beneficiary assignment reflects the influence of ACO participant list changes. Under this methodology, the historical benchmarks for ACOs with participant list changes from one performance year to the next continue to reflect the ACOs' historical costs in relation to their current composition.
(4) Background on Resetting the Benchmark
In the November 2011 final rule (see 76 FR 67915) establishing the Shared Savings Program, some commenters expressed concerns that rebasing the benchmark at the start of each agreement period would make savings more difficult to attain and eventually make savings unattainable by ACOs. Stakeholders have continued to express concerns about this methodology for rebasing the benchmark. They assert that the current methodology may also reduce the incentive for ACOs to achieve savings since any savings achieved during a given agreement period would result in lower future benchmarks, generating an offsetting reduction in the shared savings payments the ACO would receive in those future agreement periods.
During the initial rulemaking, commenters suggested a variety of alternatives to rebasing the benchmark for each agreement period, as well as technical suggestions on how to reset the benchmark (76 FR 67915 through 76 FR 67916). In the November 2011 final rule, we adopted a policy under which an ACO's benchmark would be reset at the start of each agreement period, as required under section 1899(d)(1)(B)(ii) of the Act. In finalizing this policy, we explained our belief that resetting the benchmark at the beginning of each agreement period would most accurately account for changes in an ACO's beneficiary population over time. We explained that because of turnover in an ACO's assigned beneficiary population, by the end of the agreement period, an ACO's assigned population may be significantly different from the historically assigned beneficiary population used to calculate the ACO's initial benchmark. Further, resetting the benchmark at the beginning of subsequent agreement periods would allow the benchmark to more accurately reflect the composition of an ACO's population, and therefore protect both the Trust Funds and ACOs. We acknowledged commenters' concerns that resetting the benchmark after 3 years could ultimately make it more challenging for ACOs to achieve savings, particularly for low-cost ACOs. However, we explained our belief that one of the fundamental purposes of the Shared Savings Program is to provide incentives for ACOs to strive continually to make further advances in the quality and efficiency of the care they provide (76 FR 67916).
Under § 425.602(c) of the rule, an ACO's benchmark would be reset at the start of its second or subsequent agreement period using the same methodology for establishing the historical benchmark under § 425.602(a). The existing regulations do not specify any alternative methodology for rebasing the benchmarks for ACOs that have completed one or more agreement periods in the Shared Savings Program. For example, for an ACO with a January 2013 agreement start date that continues in the program for a second agreement period beginning January 1, 2016, we would establish the ACO's historical benchmark for its second agreement period according to the methodology set forth in § 425.602(a). In particular, we would compute the ACO's benchmark for its second agreement period based on per capita Parts A and B fee-for-service expenditures for beneficiaries that would have been assigned to the ACO Start Printed Page 72836in any of the 3 most recent years prior to the agreement period using the ACO participants' TINs identified at the start of the agreement period (§ 425.602(a)). In the example of an ACO with an initial agreement period beginning January 1, 2013 and a second agreement beginning January 1, 2016: The ACO's historical benchmark for its first agreement period would have been based on the historical years of 2010, 2011 and 2012 and the ACO's historical benchmark for its second agreement period would be based on the historical years of 2013, 2014 and 2015. In resetting the benchmark, the time period for the benchmark shifts forward to capture the ACOs participants' more recent historical spending. As noted previously, we adjust an ACO's benchmark based on the ACO participant list that it certifies at the start of each performance year, which may reflect changes during the course of the prior performance year. Similarly, in resetting the ACO's benchmark at the start of a second agreement period, we would effectively account for any ACO participant list changes between the ACO's third performance year under its first agreement period and its first performance year under its second agreement period.
Early experience for ACOs participating in the Shared Savings Program is limited to financial performance results for the first performance year of ACOs with 2012 and 2013 start dates. However, we anticipate that the trend for ACOs participating in the Shared Savings Program will be similar to the trend for sites in the Physician Group Practice (PGP) demonstration, with more organizations generating savings as they gain experience in a shared savings model. In the initial performance year of the PGP Demonstration, two sites were eligible for shared savings payments. As the demonstration progressed, more PGP sites demonstrated savings. Over the course of the 5-year demonstration, 7 of the 10 PGP sites were eligible for shared savings payments in one or more performance years.
The experience of PGP demonstration sites is also an indication that resetting ACO benchmarks at the start of the second and each subsequent agreement period would not deter ongoing participation in the program by ACOs. We note, however, that unlike the update methodology currently used in the Shared Savings Program, the benchmarks used in the PGP demonstration were updated using regional factors, as opposed to national factors. This approach is similar to some of the alternatives discussed later in this section, on which we are seeking comment. The benchmarks for the PGP sites were reset as they moved from the PGP demonstration to the PGP Transition Demonstration, and again when they transitioned into the Pioneer ACO Model or the Shared Savings Program. We note that most of the organizations participating in the PGP demonstration elected to continue their voluntary participation under these shared savings models, even though their benchmarks would be reset under the applicable benchmarking methodology. Based on this experience, we conclude that these organizations must have believed there was a sufficient opportunity to share in savings as well as other strategic and competitive advantages to warrant their continued participation in a shared savings initiative, even under a rebased benchmark that reflected the cost savings achieved by the site under the PGP demonstration.
However, while the PGP experience establishes that the current approach to rebasing is consistent with continued participation, at least in some cases, it is possible that additional organizations would have continued into the Pioneer ACO Model or the Shared Savings Program under an alternative rebasing methodology. The PGP experience cannot rule out the possibility that an alternative rebasing methodology could induce ACOs to achieve greater savings, particularly as providers gain more familiarity with the payment model, or could prove more sustainable over time.
(5) Background on Stakeholders' Concerns about Benchmarking Methodology
Since the initial rulemaking, stakeholders have continued to express their concern that resetting ACO benchmarks at the start of each agreement period, as required under the existing methodology, may disadvantage ACOs, particularly those that have generated shared savings. A closely related concern is that because savings achieved during one agreement period would lead to a lower benchmark in future agreement periods, achieving savings could hypothetically be financially unattractive for ACOs in some circumstances. Under the existing benchmarking methodology, an ACO that performs well in its first agreement period as a result of its effective strategies for lowering Medicare expenditures may have a significantly lower historical benchmark in its subsequent agreement period. Consequently, some stakeholders believe that achieving savings may sometimes be financially unattractive for ACOs because these savings would reduce their benchmarks for future periods. They are concerned that the value proposition of the program may diminish over time as ACOs become lower-cost entities, and, as a result, face increased difficulty in achieving additional efficiencies (hence savings) when judged against decreasing benchmarks.
Further, some stakeholders have expressed concern that the existing benchmarking methodology does not sufficiently account for the influence of cost trends in the surrounding region or local market on the ACO's financial performance. In particular, some stakeholders voiced concerns about the low or negative update amounts used during first performance year reconciliation under the existing benchmarking methodology, and favor alternative approaches, which they believe are more certain to yield positive updates to ACOs' historical benchmarks. Others have suggested that we move away from an approach for setting ACO-specific benchmarks and toward an approach for setting regionally-specific benchmarks for ACOs. These concerns, as with those raised regarding the methodology for resetting benchmarks in subsequent agreement periods, center on whether the benchmarks are set at a level ACOs perceive to be sufficient to make program participation financially viable.
We believe it is timely to consider these issues in the context of encouraging continued participation by ACOs in the program and continued improvement in ACO performance, particularly as ACOs with 2012 and 2013 start dates begin to contemplate whether to continue in the program for a second agreement period. Further, we believe there may be important interactions between the way in which the benchmarks for ACOs are set in their initial agreement period and reset in their subsequent agreement periods and encouraging participation by ACOs in the program's two-sided models (particularly ACOs that entered the program under Track 1 and are contemplating moving to a risk based track); namely in terms of the value proposition of moving to a performance-based risk track.
b. Factors To Use in Resetting ACO Benchmarks and Alternative Benchmarking Methodologies
We considered whether modifying the methodology used for establishing, updating, and resetting ACO benchmarks to account for factors relevant to ACOs that have participated in the program for 3 or more years Start Printed Page 72837would help ensure that the Shared Savings Program remains attractive to ACOs and continues to encourage ACOs to improve their performance, particularly those that have achieved shared savings. As discussed later in this section, we considered a range of modifications to the benchmarking methodology in order to expand the methodology for resetting benchmarks to account for factors relevant to continued participation by ACOs in subsequent agreement periods and to increase incentives to achieve savings in a current agreement period, specifically: (1) Equally weighting the 3-benchmark years; (2) accounting for shared savings payments in benchmarks; (3) using regional FFS expenditures (as opposed to national FFS expenditures) to trend and update the benchmarks; (4) implementing an alternative methodology for resetting ACO benchmarks that would hold an ACO's historical costs, as determined for purposes of establishing the ACO's initial historical benchmark for its first agreement period, constant relative to costs in its region for all of the ACO's subsequent agreement periods; and (5) implementing an alternative methodology for resetting ACO benchmarks that would transition ACOs to benchmarks based only on regional FFS costs, as opposed to the ACO's own historical costs, over the course of multiple agreement periods. Further, we considered whether to apply these changes broadly to all ACOs or to apply these changes only when resetting benchmarks for ACOs entering their second or subsequent agreement periods. We also considered whether to apply these changes to a subset of ACOs, such as ACOs participating under a two-sided model (Tracks 2 and 3) or Track 3 ACOs only. In considering these potential options for modifying the benchmarking methodology, it is necessary to balance the desire to make the program more financially attractive to ACOs, against the need to protect the Medicare Trust Funds.
Although we are not proposing any changes to our benchmarking methodology at this time, we are seeking comment on these alternatives for how we approach establishing, updating and resetting benchmarks, as well as suggestions regarding alternative approaches not described here. We will carefully consider the comments that are received regarding these options during the development of the final rule, and may consider adopting one or more of these options in the final rule. We note, however, that any option that relies upon the use of the authority under section 1899(i)(3) of the Act to adopt alternate payment models must be determined to improve quality and efficiency and not to increase program spending.
(1) Equally Weighting the 3 Benchmark Years
Pursuant to section 1899(d)(1)(B)(ii) of the Act, in the November 2011 final rule, we adopted a methodology for establishing ACO benchmarks under which we weight benchmark expenditures at 60 percent for Benchmark Year (BY) 3, 30 percent for BY2, and 10 percent for BY1 (§ 425.602(a)(7)). As we explained in the November 2011 final rule (76 FR 67915), this weighting helps ensure that the benchmark reflects more accurately the latest expenditures and health status of the ACO's assigned beneficiary population. We indicated that giving BY3 the greatest weight would most accurately reflect recent cost trends for the Medicare beneficiaries who receive the plurality of their primary care from ACO providers/suppliers, and thus result in a more accurate benchmark.
To establish an ACO's benchmark for an agreement period, we determine the per capita Parts A and B fee-for-service expenditures for beneficiaries that would have been assigned to the ACO in any of the 3 most recent years prior to the agreement period using the ACO participants' TINs identified at the start of the agreement period (§ 425.602(a)). Therefore, an ACO's benchmark under a second or subsequent agreement period will reflect, to some degree, its previous performance under the program. For example, for ACOs with 2013 start dates that continue in the program for a second agreement period beginning January 1, 2016, BY1 will be based on expenditures for beneficiaries who were assigned to the ACO based on CY 2013 (the timeframe corresponding to performance year 1 under the first agreement period). Likewise, BY2 will be based on assignment for CY 2014 (performance year 2) and BY3 will be based on assignment for CY 2015 (performance year 3). We note, however, that a number of factors will affect beneficiary assignment for purposes of establishing ACO benchmarks in subsequent agreement periods, which may cause an ACO's benchmark year assigned population to deviate from its assigned population for the corresponding performance year. For example, an ACO may add or remove ACO participant TINs in its second or subsequent agreement period. Further, participation in the program by other organizations in an ACO's market may also change in the time between when we performed assignment for the performance year under the prior agreement and when we assign beneficiaries for the purpose of resetting the ACO's benchmark for the next agreement period, leading to changes in the ACO's assigned beneficiary population for purposes of establishing its benchmark for the new agreement period. The impact of these kinds of changes in the assigned beneficiary population between the performance year and the time the benchmark is established for a subsequent agreement is uncertain, and could result in either upward or downward adjustments to expenditures for purposes of establishing the benchmark.
Among ACOs whose assigned beneficiary populations for purposes of resetting the benchmark closely match their assigned beneficiary population for the corresponding performance years, those ACOs that generated savings during a prior agreement period will have comparatively lower benchmarks for their next agreement period. This is because the ACOs were effective in lowering expenditures for these assigned beneficiaries. We assume, for example, that if an ACO generates savings in its first agreement period it is likely that the impact on claims would be most significant in the second or third performance year as opposed to being uniformly distributed across all three performance years. This hypothesis is supported by following factors:
- There may be a lag between when an ACO starts care management activities and when these activities have a measurable impact upon expenditures for the ACO's assigned beneficiary population.
- ACOs may improve their effectiveness over time as they gain experience with population management and improve processes.
- There may be higher care costs during the early period of performance to treat or stabilize certain patients, as the ACO's care management activities involving these patients commence. Once stabilized, these patients may show relatively lower care costs over the course of time due to more effective, coordinated and quality care.
Under these circumstances, resetting the benchmark for ACOs starting a second or subsequent agreement period under the Shared Savings Program becomes a trade-off between the accuracy gained by weighting the benchmark years at 60 percent for BY3, 30 percent for BY2 and 10 percent for BY1 and the potential for further reducing the benchmarks for these ACOs by giving greater weight to the Start Printed Page 72838later performance years of the preceding agreement period. Unchanged, the application of this methodology for weighting the benchmark years when resetting benchmarks could reduce the incentive for ACOs that generate savings or that are trending positive in their first agreement period to participate in the program over the longer run, or to reduce incentives for ACOs to achieve savings in their first agreement period. For instance, ACOs that have previously performed well under the program may be discouraged from continuing to participate in the program if their rebased benchmark is so low that they would have difficulty continuing to lower expenditures sufficiently to exceed their MSR in order to be eligible for shared savings during their next agreement period.
We considered an alternative methodology for resetting benchmarks where we would weigh the benchmark years equally (ascribing a weight of one-third to each benchmark year). We believe that equally weighting the benchmark years could more gradually lower the benchmarks of ACOs that perform well in their first agreement period, in contrast to giving the greatest weight to the most recent prior benchmark year, which, for the reasons discussed previously, is likely to be the year in which an ACO would have been most effective in lowering expenditures for its assigned population. This alternative approach would have the most significant impact upon ACOs whose assigned population during the three performance years of the preceding agreement period most closely approximates the assigned population used to determine their benchmark for the subsequent agreement period. This approach may be less accurate, and therefore less protective of the Trust Funds, since it may not sufficiently account for an ACO's most recent historical cost experience, particularly in the case of an ACO whose ACO participant composition (and therefore its assigned beneficiary population) changed over the course of the agreement period, such that its assigned beneficiary population in the subsequent agreement period is significantly different from the beneficiary population in the early years of its prior agreement period; this effect could be counteracted to the extent that this approach encourages greater participation in the Shared Savings Program or encourages ACOs to achieve greater shared savings.
(2) Accounting for Shared Savings Payments in Benchmarks
We also considered revising the methodology for resetting ACO benchmarks to account for shared savings earned by an ACO in its prior agreement period, as a way to encourage ongoing participation by successful ACOs and improve the incentive to achieve savings. Similar to the option of equally weighting the benchmark years discussed above, accounting for an ACO's shared savings during its prior agreement period would more gradually lower the benchmarks of ACOs that perform well in their prior agreement period.
The statute outlines the scope of Medicare expenditures to be used in calculating ACO benchmarks. Section 1899(d)(1)(B)(ii) of the Act specifies that the benchmark is established “. . . using the most recent available 3 years of per-beneficiary expenditures for parts A and B services for Medicare fee-for-service beneficiaries assigned to the ACO.” This provision of the Act further specifies: “Such benchmark shall be adjusted for beneficiary characteristics and such other factors as the Secretary determines appropriate.” In the November 2011 final rule establishing the Shared Savings Program, we explained that in implementing section 1899(d)(1)(B)(ii) of the Act, we would take into account payments made from the Medicare Trust Funds for Parts A and B services, for assigned Medicare fee-for-service beneficiaries, including payments made under a demonstration, pilot or time limited program when computing average per capita Medicare expenditures under the ACO. Our policies for determining per capita expenditures for purposes of establishing the benchmark are specified at § 425.602(a)(1). Shared savings payments are paid from the Medicare Trust Funds for the beneficiary population assigned to an ACO and are intended to recognize the costs incurred by the ACO and its ACO participants and ACO providers/suppliers in coordinating care and improving the quality of care for the assigned beneficiaries. Accordingly, we are considering whether it would be appropriate to revise our methodology under § 425.602(a)(1) for establishing an ACO's benchmark to incorporate the ACO's share of savings for those ACOs that receive shared savings payments under the prior agreement period. We considered how to account for these payments in ACOs' 3-year weighted average per capita benchmarks since ACO shared savings payments are determined at the population-level, reflecting aggregated per capita expenditures that have been truncated and annualized and weighted by the proportion of assigned beneficiaries in each of the four Medicare enrollment types: ESRD, disabled, aged/dual and aged/non-dual. For instance, we could develop a per-beneficiary average based on the shared savings payment for the particular performance year under the prior agreement period and apply this adjustment on a per beneficiary basis to the assigned population for the corresponding benchmark year. We also considered whether to make a symmetric adjustment in benchmarks for ACOs that owed losses in a previous agreement period.
We believe there are merits to upwardly adjusting benchmarks for ACOs in a second or subsequent agreement period to reflect any shared savings payments in the most recent prior agreement period. An adjustment that reflects the ACO's share of savings—based on its final sharing rate, which is a function of its quality performance—in the computation of the benchmark would increase the ACO's benchmark for the subsequent agreement period. This increase in the benchmark, relative to the ACO's prior success in the program, may address concerns expressed by some stakeholders (described previously) that under the existing benchmarking methodology achieving savings may sometimes be financially unattractive for ACOs because of the potential impact on their benchmarks in future agreement periods.
There are clear advantages of this adjustment for ACOs and the Medicare program. In particular, ACOs would have an increased incentive to continue to generate shared savings and improve quality because of the prospect of having a higher benchmark in future agreement periods. Consequently, ACOs may demonstrate improved performance over longer term participation in the program. Further, ACOs may be encouraged to enter the program's two-sided models (such as the proposed Track 3), which offer higher final sharing rates because making an adjustment to the benchmark for these ACOs to reflect successful participation during one agreement period may improve their potential to receive shared savings in the next agreement period. Other implications of this adjustment for consideration include the following:
- Not all ACOs would benefit. By making the adjustment only for ACOs that receive shared savings payments in their prior agreement period, some ACOs that reduce expenditures would Start Printed Page 72839not receive the benefit of this adjustment. Specifically, ACOs whose performance year expenditures are lower than their benchmark expenditures by an amount that did not meet or exceed their MSR, and ACOs that generated savings outside their MSRs, but that failed to satisfy the quality reporting standard, would not receive the adjustment.
- Availability of performance data relative to timely creation of benchmarks. We anticipate completing financial reconciliation for an ACO's most recent prior performance year (for example, PY3 under the first agreement period which corresponds to BY3 for the second agreement period) mid-way through its current performance year (for example, PY1 under the second agreement period). As a result, one downside of relying on the availability of performance data from the most recent prior performance year is that it would delay the finalization of an ACO's historical benchmark for its first performance year during its subsequent agreement period.
(3) Use of Regional Factors (as Opposed to National Factors) in Establishing and Updating Benchmarks
Some stakeholders have expressed concern that the existing benchmarking methodology does not sufficiently account for the influence of cost trends in the surrounding region or local market on the ACO's financial performance. We considered addressing these concerns by using regional FFS expenditures, instead of national FFS expenditures, to trend forward the most recent 3 years of per beneficiary expenditures for Parts A and B services in order to establish the historical benchmark for each ACO under section 1899(d)(1)(B)(ii) of the Act. In addition, we considered making this modification in combination with an alternative payment model under section 1899(i)(3) of the Act under which we would use regional FFS expenditures, instead of national FFS expenditures, to update the benchmark for each performance year during an agreement period. We also considered other approaches to address this concern, as discussed later in this section describing alternative benchmarking methodologies.
In considering how to establish and update benchmarks based on regional factors, we favor use of an approach similar to the method for updating benchmarks used under the PGP demonstration, which has been tested and validated with physician groups across the country, including groups in rural, urban and suburban areas. Under this approach, much of the Shared Savings Program's existing benchmarking methodology would remain the same. Instead of using national Medicare FFS expenditure data to trend expenditures in establishing the historical benchmark (§ 425.602(a)(5)) and to update the benchmark for each performance year (§ 425.602(b)(1)), we would use regional FFS expenditure data to make these adjustments. We would calculate the ACO's regional expenditure trend and update factors according to the cost experience of a reference population. Specifically, in establishing benchmarks under the PGP demonstration, a comparison group was created using the PGP's service area. The growth rate of the comparison group expenditures was calculated and used as the growth rate for updating the PGP's benchmark. Specifically, we used each PGP's annual assigned beneficiary population to determine the PGP's service area. A PGP's service area was defined as all counties where one percent or more of assigned PGP beneficiaries reside. We identified which beneficiaries residing in each service area met the comparison group assignment criteria and assigned them to the PGP comparison group. The service area and comparison group for the PGP were re-determined each year to account for changes in the PGP's assigned beneficiaries. The expenditure growth rate for the PGP's comparison group was calculated and used to update the PGP's historical benchmark for purposes of determining each PGP's performance under the shared savings calculation methodology used in the demonstration. This benchmarking methodology was used over the course of the 5-year PGP demonstration. Given that we have already tested and refined this methodology, we believe that a similar approach could be implemented within the Shared Savings Program. As noted previously, over the course of the PGP demonstration, 7 of 10 sites were eligible for shared savings payments in one or more performance years. Taking these factors into consideration, we believe stakeholders may welcome this approach to revising the program's benchmarking methodology.
However, we have also identified a number of additional factors that must be considered in using this approach in the Shared Savings Program:
- Whether the comparison group counties should be weighted by the percent of assigned beneficiaries in the county out of all assigned beneficiaries in all comparison group counties. For example, for an ACO in a rural or suburban county near a large metropolitan area: On a weighted basis, the large metropolitan area would contribute less to the comparison group than on an unweighted basis. Alternatively, an ACO with high penetration in a specific county would have its regional factors significantly influenced by that county.
- Whether to establish a minimum sample size for the comparison group, such as equal to or greater than 25,000. Smaller comparison groups are more likely to demonstrate idiosyncratic expenditure trends, for instance, if an ACO has a high penetration in its service area, the remaining population may be non-representative compared to the ACO's patient population. These factors would seem to support the use of a minimum sample size threshold. Based on statistical modeling for an effective sample size, we anticipate that the minimum sample size threshold would be set not lower than 25,000 beneficiaries. In turn, a minimum sample size raises a question of what criteria should be used to ensure the ACO's comparison group is large enough. For instance, in markets where the ACO's assigned beneficiaries represent a substantial share (for example, more than 40 percent) of Medicare FFS beneficiaries, should the region be expanded—perhaps to include the entire corresponding metropolitan statistical area (MSA), hospital referral region (HRR), or another regional grouping approach? Similarly, in markets where multiple ACOs represent a substantial share (for example, more than 50 percent) of Medicare FFS beneficiaries, should the region be similarly expanded as described previously? We also considered whether to lock-in the counties composing the comparison group at the start of the agreement period, since over the course of the agreement the counties where one percent or more of assigned ACO beneficiaries reside may fluctuate (for example, just above or just below 1 percent).
(4) Alternative Benchmark Resetting Methodology: Holding the ACO's Historical Costs Constant Relative to its Region
Some stakeholders have also expressed a preference for further changes in the methodology used to reset ACO benchmarks to address the concerns described previously. For example, some stakeholders have suggested that ACOs would have stronger incentives to achieve shared savings during a given agreement period and to continue to participate in the program in subsequent agreement periods if we used a methodology for resetting benchmarks that held the ACO's historical per assigned Start Printed Page 72840beneficiary spending constant relative to its local market so that improvements in efficiency that the ACO achieved during an agreement period would not lower its benchmark for a subsequent agreement period.
Accordingly, we considered using the authority under section 1899(i)(3) of the Act to establish an approach to resetting an ACO's benchmark at the start of a new agreement period under which the ACO's benchmark from the prior agreement period would be updated according to trends in FFS costs in the ACO's region, effectively holding a portion of the ACO's benchmark constant relative to its region. Under this approach, an ACO's benchmark for its initial agreement period would be set according to an approach similar to the existing methodology. For subsequent agreement periods, the trend in regional costs would be calculated using an approach based on the PGP demonstration, described previously, and the historical benchmark would be updated by increasing it by a percentage equal to the percentage increase in regional costs. This approach would prevent an ACO's improved efficiency during an agreement period from lowering its benchmark in a future agreement period.
We also considered a similar approach that would use information regarding the ACO's historical costs under its first agreement period to adjust regional FFS benchmarks developed for future agreement periods by developing a scaling factor. The scaling factor could be calculated as the ratio of—(1) an ACO's historical benchmark under its first agreement period (computed using an approach similar to the existing methodology) divided by; (2) the regional FFS benchmark that would have been calculated for the ACO for the third benchmark year of its first agreement period. We would compute an ACO's benchmark for each subsequent performance year by multiplying this scaling factor by the ACO's regional FFS benchmark for that performance year to account for the difference originally exhibited between the ACO expenditures and the regional FFS benchmark expenditures in the year prior to the beginning of the ACO's first agreement period. The regional FFS benchmark for an ACO in a given performance year would be computed using an approach based on the PGP demonstration described above. For example, if the ACO's assigned beneficiaries expenditures were 10 percent higher than what its regional FFS benchmark would have been in its most recent base year of its initial agreement period, the ACO's future benchmark based on regional FFS expenditures would be adjusted by 10 percent to account for this baseline difference. This approach would likely generate benchmarks very similar to those described in the previous paragraph and thus have a similar effect on an ACO's incentives to improve efficiency.
Under both of these approaches, we considered whether to adjust the benchmark or scaling factor to reflect changes in the list of ACO participant TINs over time, as we do now based on our authority under § 425.602((a)(8). We considered two approaches to making such adjustments, each of which could be used with either of the basic approaches to holding benchmarks constant relative to an ACO's region that were previously described. Under the first approach, we considered basing such adjustments off our current method of adjusting the benchmark on an annual basis to reflect ACO participant changes. Under the second approach, we considered an adjustment method to reflect the historical cost experience of any ACO participant TINs that are added to the ACO and to remove the influence of the cost experience of those ACO participant TINs that leave the ACO, but not incorporate updated cost information for ACO participants that have continued in the ACO.
First, we considered using an approach similar to our existing method for adjusting the ACO's benchmark during the course of its agreement period to account for changes in its ACO participant list as described previously.
Under this approach, each performance year that the ACO's participant list changed, we would recompute its initial historical benchmark or scaling factor using cost information from the benchmark period corresponding to the ACO's initial agreement period. This approach has the advantage that it is similar to the approach we have used successfully to adjust ACO benchmarks within an agreement period in response to changes in ACO participant lists. However, we recognize that not all ACO participants joining the ACO in subsequent agreement periods may have historical claims data during the 3 years prior to the start of the ACO's first agreement period. Therefore, we considered the need to expand this approach to include adjustments to the benchmark or scaling factor to account for ACO participant list changes.
Second, we considered an approach that would adjust an ACO's benchmark (or scaling factor) after each annual change in the ACO participant list based on the relative cost experience of patient populations associated with the new performance year's set of TINs relative to the prior performance year's set of TINs, as measured during a period immediately preceding the change in the ACO participant list. We note that under our current benchmarking methodology, assigned beneficiaries and benchmark expenditures are determined in aggregate at the ACO level rather than at the individual ACO participant TIN level. Therefore, under this alternative approach, we would develop a methodology for associating assigned beneficiary costs to individual ACO participant TINs that continue in the program so as not to incorporate updated cost information for the patient populations associated with the continuing ACO participants, as well as to incorporate updated cost information for the patient populations associated with new ACO participants or remove the influence of cost information for patient populations associated with departing ACO participants.
The advantage of this type of approach is that it could generate more accurate benchmarks in cases where an ACO adds many participant TINs that were not active during the ACO's initial agreement period. However, this approach could be more complicated to implement and could reintroduce a limited ability for ACOs to influence future benchmarks through current decisions.
A potential disadvantage of approaches that determine benchmarks by holding an ACO's costs constant relative to its region is that future benchmarks are influenced to a large degree by holding the cost experience for the ACO participants that continue in the ACO static. This static cost experience would become dated and would not necessarily reflect the evolving complex factors that influence the cost profile of the beneficiary populations assigned to the ACO in future agreement periods. By holding costs static for existing ACO participants, there would be incentives for successful ACOs to continue to participate in the program (with the same ACO participant composition) against more favorable benchmarks. Moreover, some ACOs may “shop” for a particularly advantageous benchmark, for instance by delaying program entry, and only improving their expenditure and utilization trends in later years. As a result, these approaches might continue to yield shared savings for some ACOs despite marginal effort to improve efficiency, and push out ACOs for whom cumulative variation creates a Start Printed Page 72841predictable and unrealistically low expenditure target.
To the extent that this approach for resetting ACO benchmarks also incorporates elements of the other approaches described in this section, we would be faced with related concerns. For instance, when trending the benchmark according to regional FFS costs based on the PGP demonstration approach described above, we would need to determine what criteria to use in establishing the comparison group. Further, as discussed under the alternative benchmarking methodology later in this section, we may need to consider whether the risk adjustment methodology would need to be modified, in this case to account for changes in each ACO's risk profile relative to the risk profile of its regional comparison population. The types of approaches described in this section would require use of our authority under section 1899(i)(3) of the Act because we would be deviating from the requirement at section 1899(d)(1)(B)(ii) of the Act that the benchmark be reset at the start of each agreement period. Specifically, the benchmark would not be reset using the most recent available 3 years of per beneficiary expenditures for parts A and B services for those Medicare FFS beneficiaries that were assigned to the ACO during the preceding agreement period.
(5) Alternative Benchmark Methodology: Transitioning ACOs to Benchmarks Based Only on Regional FFS Costs Over the Course of Multiple Agreement Periods
We also considered using our authority under section 1899(i)(3) of the Act to transition ACOs from benchmarks based on their historical costs toward benchmarks based only on regional FFS costs, an approach suggested by stakeholders, including MedPAC. We recognize that under the existing benchmarking methodology, ACOs in the same market would have unique benchmarks, which may vary widely depending on the historical expenditures for the beneficiaries that receive care from the ACO participants in each ACO. As a result, ACOs within the same market may have substantially different benchmarks, such as the case of a historically low-cost ACO within a traditionally high cost market. Under the existing benchmarking methodology, the program may be more attractive (initially) to historically high-cost ACOs able to enter the program and achieve substantial shared savings by bringing costs down compared to their historical cost performance. ACOs with historically low costs may be less likely to enter and continue in the program because of their perceived difficulty in further reducing their assigned beneficiaries' costs relative to a benchmark based on their assigned beneficiaries populations' past experiences. However, as noted previously, the current benchmarking methodology may provide additional opportunity for increased shared savings for ACOs with low costs relative to the national average through the use of a flat dollar update for growth in national FFS expenditures, assuming program expenditure trends return to historically-familiar positive rates as compared to the unusually low growth experienced in the first several years of the program.
Under this alternative approach, over the course of several agreement periods, we would transition to using regional FFS cost data to make ACO benchmarks gradually more independent of the ACO's past performance and gradually more dependent on the ACO's success in being more cost efficient relative to its local market. For example, for the ACO's first agreement period, we may use the existing benchmarking methodology or one of the options described previously, which accounts for regional FFS expenditures. Starting in an ACO's second agreement period, we would calculate each ACO's benchmark as a weighted average of the ACO benchmark using the existing approach or one of the alternative approaches described above and risk adjusted regional FFS costs. The weight placed on risk adjusted regional FFS costs would increase over time. ACOs' assigned beneficiaries would be counted in the calculation of regional FFS costs and the definition of an ACO's region would require careful consideration so that the ACO's assigned beneficiary population would not be allowed to make up an unreasonable proportion of the region itself. This benchmarking methodology would help ensure the program remains attractive to ACOs, particularly those who have achieved shared savings in previous agreement periods, and strengthen the connection between the determination of the amount of shared savings earned by the ACO and an ACO's actual success in achieving savings relative to its region and local market.
An approach where we transition from ACO-specific benchmarks based on each ACO's historical costs to benchmarks based on regional FFS spending may be attractive to low-cost ACOs in high-cost regions because they would likely transition to a relatively higher (regional) benchmark over time against which they could likely show more savings because they have lower relative costs. However, high-cost ACOs in low-cost regions may find a regional benchmark unattractive because they would be required to create new efficiencies to fully offset their higher costs relative to their region in order to show savings under the benchmark. To mitigate the cost of any resulting selective participation by favored low-cost ACOs in high cost regions we considered whether a benchmark transition process could be employed over a number of agreement periods involving a gradual shift from the current methodology to one where benchmarks are set based on regional FFS spending (for example, using a weighted average of the two approaches whereby the weight for the regional FFS benchmark is gradually increased over several agreement periods). Using regional FFS spending to establish benchmarks could reward low-cost, high-quality ACOs, and further encourage them to attract more ACO participants and Medicare FFS beneficiaries over the course of time. We would also expect that a gradual transition may at least initially maintain an incentive for existing ACOs with high costs relative to their region to remain in the program because the initial ACO-specific benchmark would allow the ACOs to achieve shared savings for lowering their costs compared to their own historical performance. As they transition to a benchmark based on regional FFS spending, these ACOs' benchmarks would likely decline (given the overall experience of the market), encouraging these ACOs to continue to reduce their costs, while maintaining high quality care under the program. However, we also note that some ACOs may not perceive an ability to reduce their beneficiary expenditures below the regional average and therefore there remains a risk that the eventual transition to a regional benchmark would result in selective participation regardless of how the transition is performed. For instance, an ACO that perceives its patient population as having high relative costs may perceive itself as disadvantaged under this approach.
Therefore, to further mitigate selective participation and improve the accuracy of the benchmarks, we considered whether the regional FFS benchmark should be adjusted to reflect a regional or local reference population, similar to the method used in the PGP demonstration. However, as described previously, additional adjustment may be necessary to ensure the comparison Start Printed Page 72842population is sufficiently large and representative of the ACO's assigned patient population, particularly in the cases where ACOs make up a significant portion of their regional market.
We also considered whether the risk adjustment methodology would need to be modified to account for changes in the risk profile of the regional population rather than the national population. For instance, it may be necessary to account for coding intensity differences relative to the ACO's region rather than just the change in coding intensity by the ACO. As we explained in the November 2011 final rule (see 76 FR 67916), it may be necessary to guard against changes that result from more specific or comprehensive coding as opposed to improvements in the coordination and quality of health care. Thus, we considered the need for normalization of risk scores for ACO assigned beneficiaries and the comparison group beneficiaries relative to the regionally based comparison group. For instance, the benchmark could be normalized to the mix of beneficiaries assigned across the four Medicare enrollment types (ESRD, disabled, aged/dual, aged/non-dual) to the same strata within the regional comparison population. We also considered risk adjusting the growth rates, for example based upon risk scores for the comparison group, in combination with using a regional coding intensity adjustment or independently.
We also considered how to account for ACO participant TIN changes, over time, under a methodology where we transition ACOs from ACO-specific to regionally based benchmarks. For instance, we considered whether to continue to adjust the benchmark at the start of each performance year to reflect changes in the set of ACO participant TINs that constitutes the ACO, perhaps similar to our current approach to managing changes to ACO participants during the agreement period.
We also considered the pace for transitioning ACOs from ACO-specific to regional benchmarks, including the following factors:
- The period of time for transitioning to regional FFS benchmarks: For instance, should the transition occur over two agreement periods, or five agreement periods, or longer.
- Whether to consider the ACO's performance during a prior agreement period in determining the pace of its transition to regional FFS benchmarks. For example, should we delay downward adjustments to an ACO's benchmark if the ACO fails to achieve shared savings.
- Whether to consider the ACO's historical costs, relative to regional Medicare FFS average per capita costs, in determining the pace of its transition to regional FFS benchmarks. For example, should low-cost ACOs (those below the risk adjusted regional Medicare FFS average per capita costs) transition more quickly to regional FFS benchmarks than high-cost ACOs.
Another consideration was whether this kind of benchmarking methodology would allow the Shared Savings Program to maintain a fiscal balance. For instance, would the shared savings paid to low-cost ACOs (treating beneficiaries at below average costs) be more than offset with savings from lower than expected spending in high-cost ACOs and further control of spending growth in low-cost ACOs. We also recognize that more customized benchmarking approaches make it more difficult to provide ACOs with information they can use to predict their performance.
(6) Seeking Comment on the Benchmarking Alternatives Considered and the Applicability of These Approaches
In general we seek comment on the approaches to adjusting the methodology for establishing, updating and resetting ACO benchmarks discussed in detail above. In particular, we seek comment on the following:
- Using combinations of these approaches, as opposed to any one approach. Specifically, we considered revising the methodology for resetting ACO benchmarks by equally weighting the three benchmark years, and/or accounting for shared savings payments received by an ACO in its prior agreement period, and/or using regional FFS expenditures instead of national FFS expenditures in establishing and updating the benchmark. We also considered and seek comment on revising the benchmarking methodology more broadly, shifting either to a methodology that resets ACOs' benchmarks between agreement periods by holding an ACO's historical costs constant relative to costs in its region or to a methodology that transitions ACOs from benchmarks based on their historical costs toward benchmarks based only on regional FFS costs, potentially in combination with some or all of the other revisions we are considering to the benchmarking methodology.
- How broadly or narrowly to apply these alternative benchmarking approaches to the program's Tracks. Specifically, we envisioned that the revisions in the benchmarking methodology under section 1899(d)(1)(B)(ii) of the Act. (for example, equally weighing the three benchmark years, and accounting for shared savings payments received by an ACO in its prior agreement period) would be applied when resetting the benchmarks for all ACOs, regardless of the model they participate under (Tracks 1, 2, and 3). We envisioned applying the approaches requiring use of our authority under section 1899(i)(3) of the Act to ACOs participating under performance-based risk models (Tracks 2 and Track 3) because stakeholders' concerns about resetting the benchmarks were closely related to ensuring the program remains sustainable over time, and we envision ACOs would be transitioning to the performance-based risk models over time, specifically given our proposal to limit the number of agreement periods an ACO can remain under Track 1. We also considered and seek comment on applying these alternative benchmarking methodologies more broadly, specifically to all ACOs participating in a risk-based model (Tracks 2 and 3), or to all ACO financial models (Tracks 1, 2, and 3).
- Whether to use regional FFS expenditures instead of national FFS expenditures in establishing and updating the benchmark and/or a methodology for transitioning ACOs from benchmarks based on their historical costs toward benchmarks based only on regional FFS costs only when resetting ACO benchmarks under their second or subsequent agreement period, or when establishing the benchmark for all participating ACOs (regardless of agreement start date) the next full performance year after the effective date of the final rule. In other words, if a final rule adopting a revised benchmarking methodology is issued in early 2015, should the revised methodology be used to determine the benchmark that will apply during the 2016 performance year for all ACOs.
- The criteria for defining the comparison group for using regional FFS expenditure data to establish, update or reset the historical benchmark. In particular we welcome comments on the criteria we described previously and welcome commenters' suggestions for different criteria.
- We believe the concerns about risk adjustment raised in this section in the context of the alternative benchmarking methodology for establishing, updating and/or transitioning from ACO-specific benchmarks to regionally based benchmarks are also relevant to the approach where we would use regional FFS expenditures (as opposed to Start Printed Page 72843national FFS expenditures) in establishing or in updating the benchmark. We welcome comments on these concerns and commenters' suggestions about the use of regional normalization or coding intensity adjustments to guard against regional or other coding differences that may affect the characteristics of the ACOs' assigned beneficiary population in relation to the comparison group.
- We welcome commenters' detailed suggestions on our considerations of factors to use in resetting ACO benchmarks and for the alternative benchmark methodology; as well as considerations or concerns not described; and suggestions for alternative approaches for a benchmarking methodology that transition to use of regional benchmarks over the course of time. In particular, we seek commenters' input on whether an approach that transitions ACOs to regional benchmarks would encourage continued participation by existing low-cost and high-cost ACOs.
We also request commenters' input on alternatives not described here for resetting benchmarks to encourage ongoing participation by ACOs who perform well in the program and are successful in reducing expenditures for their assigned beneficiaries. We seek comment on whether these alterative benchmarking approaches would have unintended consequences for ACO participation in the program, for the Medicare Trust Funds, or for Medicare FFS beneficiaries. We intend to carefully review any comments that are received on these issues during the development of the final rule and will make an assessment at that time as to whether any change to our current methodology for establishing benchmarks is necessary and appropriate.
7. Seeking Comment on Technical Adjustments to the Benchmark and Performance Year Expenditures
When computing average per capita Medicare expenditures for an ACO during both the benchmark period and performance years under § 425.602, § 425.604, and § 425.606, we take into account all Parts A and B expenditures, including payments made under a demonstration, pilot or time limited program, with the exception of IME and DSH adjustments, which are excluded from these calculations. In the November 2011 final rule (76 FR 67919 through 67923), we considered whether to make adjustments to benchmark and performance year expenditures to exclude certain adjustments to Part A and B expenditures, including IME and DSH payments, geographic payment adjustments and some bonus payments and penalties. In the final rule, we acknowledged that taking into consideration payment changes could affect ACOs' financial performance and their ability to realize savings. However, with the exception of the adjustment to account for IME and DSH payments, we ultimately declined to make any adjustments to account for various differences in payment rates among providers and suppliers. We explained that while section 1899(d)(1)(B)(ii) of the Act provides a way of adjusting an ACO's benchmark for such payments, the statute does not include similar authority to adjust performance year expenditures. Therefore, we noted that while we could make adjustments to the ACO's benchmark to exclude certain payments under our authority in section 1899(d)(1)(B)(ii) of the Act, we did not have a similar authority to make adjustments in our calculation of an ACO's performance year expenditures, which would create a mismatch in expenditure calculations.
However, we were persuaded by commenters that not excluding IME and DSH payments in determining ACO financial performance could adversely affect the care of beneficiaries by creating an incentive for ACOs to avoid making appropriate referrals to teaching hospitals in an effort to demonstrate savings. Therefore, we considered using our authority under section 1899(i)(3) of the Act, which authorizes us to use other payment models for making payments under the Shared Savings Program that the agency “determines will improve the quality and efficiency of items and services” furnished under Medicare. Specifically we considered whether it would be appropriate to use this authority to include an adjustment to performance year expenditures to exclude IME and DSH payments. To exercise our authority under section 1899(i)(3) of the Act, we must also determine that the alternative payment model “. . . does not result in spending more for such ACO for such beneficiaries than would otherwise be expended . . . if the model were not implemented . . .”
In the November 2011 final rule (76 FR 67921 through 67922), we stated that we believed excluding IME and DSH payments would be consistent with the requirements under section 1899(i)(3) of the Act. That is, excluding these payments would both improve the care for beneficiaries while also not resulting in greater payments to ACOs than would otherwise have been made if these payments were included. Specifically, we stated that removing IME and DSH payments from benchmark and performance year expenditures would allow us to more accurately reward actual decreases in unnecessary utilization of healthcare services, rather than decreases arising from changes in referral patterns. In addition, we believed that excluding these payments from our financial calculations would help to ensure participation in ACOs by hospitals that receive these payments. Taken in combination, we believed these factors could result in Medicare beneficiaries receiving higher quality, better coordinated, and more cost-efficient care. As a result, we did not expect that excluding IME and DSH payments from the determination of ACOs' financial performance would result in greater payments to ACOs than would otherwise have been made. We also found that excluding these amounts was operationally feasible since they are included in separate fields on claims allowing them to be more easily excluded from financial calculations than certain other payments that are included on Part A and B claims. Therefore, we finalized a policy of excluding IME and DSH payments from both the benchmark and performance year expenditure calculations. We stated that we intended to monitor this issue and would revisit it if we determine that excluding these payments has resulted in additional program expenditures (76 FR 67922).
In addition to IME and DSH payments, we also considered whether standardizing payments to account for other types of payment adjustments would alleviate concerns resulting from changes in the Medicare payment systems. However, in light of the numerous payment adjustments included throughout the Medicare payment systems, we were concerned about the complexity resulting from standardizing payments and whether standardized payment information would provide meaningful and consistent feedback regarding ACO performance. We stated that we intended to evaluate this issue and would potentially address it in future rulemaking.
We also considered requests from commenters that we make adjustments to ACO benchmark and performance year expenditures to account for a number of other payments (76 FR 67922). We specifically considered how geographic payment adjustments, applied under Medicare payment systems (for example, the IPPS wage index adjustments and the physician fee schedule geographic practice cost index (GPCI) adjustments) could affect an Start Printed Page 72844ACO's ability to realize savings. These adjustments increase and decrease payments under the applicable payment systems to account for the different costs of providing care in different areas of the country. We further noted that there have been a number of temporary legislative adjustments to the wage indexes for various parts of the country during recent years. In some cases these have been extended on virtually an annual basis while others have been updated more intermittently. We recognized that the timing of these adjustments could result in changes being made during an ACO's agreement period and between the benchmark and the performance years, thus influencing an ACO's ability to realize savings under the program. Additionally, there have been cases where hospitals have moved in and out of reclassification status which can either increase or decrease the wage index in the state.
Of the comments received, most favored excluding geographic payments from benchmark and performance year expenditures (76 FR 67923). Commenters suggested specific adjustments, such as exclusion of payments based on the area wage index, low cost county payment adjustments, GPCI, and the frontier States policy adjustment. Some commenters, however, expressed concerns that variations in cost growth across geographic areas as well as the current CMS methods for accounting for differences in local input and practice costs may create incentives that reward ACO formation in some markets but not in others. Others suggested that inclusion of these geographic payment adjustments could have unintended consequences for referral patterns by ACOs, such as driving referrals based on geographic wage adjustments rather than performance. Yet others were generally concerned that making geographic payment adjustments would disproportionately disadvantage some ACOs.
Ultimately, we disagreed with commenters' suggestions that we adjust expenditures to account for various differences in cost and payment. We stated that we believed that making such extensive adjustments, or allowing for benchmark adjustments on a case-by-case basis, would create an inaccurate and inconsistent picture of ACO spending and may limit innovations in ACOs' redesign of care processes or cost reduction strategies (76 FR 67920). Unlike the IME/DSH adjustments, we stated we did not believe these other payment adjustments that are made to Part A and B payments (such as geographic payment adjustments) would result in a significant incentive to steer patients away from particular hospitals or providers since an ACO's financial performance would be compared to its own historical expenditure benchmark, as updated.
Since the publication of the November 2011 final rule, some questions have persisted regarding the most appropriate way to handle payment differences and changes under Medicare FFS; including whether to take into consideration certain payment changes that could affect ACO financial performance. We are not proposing to make any further adjustments at this time. However, now that both CMS and external stakeholders have some experience with our policies, we are interested in seeking further comment from stakeholders on this issue that we could potentially consider in future rulemaking. We are particularly interested in comments regarding standardization of payments, including which elements to adjust for, the impact of value-based payment adjustments on payments to physicians and hospitals, and the value of providing feedback on nonstandardized results while using standardized results to perform financial reconciliation.
Table 7 summarizes certain provisions of the current regulations and our proposals to change them as discussed in this section.
Table 7—Shared Savings Financial Model Overview
Track 1: One-sided risk model Tracks 2 and 3: Two-sided risk models Issue Current Proposed Current Track 2 Proposed Track 2 Proposed Track 3 Transition to Two-Sided Model First agreement period under one-sided model. Subsequent agreement periods under two-sided model Remove requirement to transition to two-sided model for a second agreement period ACOs may elect Track 2 without completing a prior agreement period under a one-sided model. Once elected, ACOs cannot go into Track 1 for subsequent agreement periods No change Same as Track 2. Assignment Preliminary prospective assignment for reports; retrospective assignment for financial reconciliation No change Preliminary prospective assignment for reports; retrospective assignment for financial reconciliation No change Prospective assignment for reports and financial reconciliation. Benchmark Reset at the start of each agreement period Seeking comment on alternative methodology Same as Track 1 Seeking comment on alternative methodology Same as Tracks 1 and 2 and seeking comment on alternative methodology. Start Printed Page 72845 Adjustments for health status and demographic changes Historical benchmark expenditures adjusted based on CMS-HCC model. Updated historical benchmark adjusted relative to the risk profile of the performance year. Performance year: Newly assigned beneficiaries adjusted using CMS-HCC model; continuously assigned beneficiaries adjusted using demographic factors alone unless CMS-HCC risk scores result in a lower risk score No change Same as Track 1 No change Same as Tracks 1 and 2. Adjustments for IME and DSH IME and DSH excluded from benchmark and performance year expenditures. No change Same as Track 1 No change Same as Tracks 1 and 2. Other payment adjustments Include other payment adjustments included in Part A and B claims such as, geographic payment adjustments and HVBP payments, in benchmark and performance year expenditures Seeking comment on other technical adjustments Same as Track 1 Seeking comment on other technical adjustments Same as Tracks 1 and 2. Quality Sharing Rate Up to 50 percent based on quality performance Up to 50 percent based on quality performance for first agreement period, reduced by 10 percentage points for each subsequent agreement period under the one-sided model Up to 60 percent based on quality performance No change Up to 75 percent based on quality performance. Minimum Savings Rate 2.0 percent to 3.9 percent depending on number of assigned beneficiaries No change Fixed 2.0 percent 2.0 percent to 3.9 percent depending on number of assigned beneficiaries Fixed 2.0 percent. Minimum Loss Rate Not applicable No change Fixed 2.0 percent 2.0 percent to 3.9 percent depending on number of assigned beneficiaries Fixed 2.0 percent. Performance Payment Limit 10 percent No change 15 percent No change 20 percent. Shared Savings First dollar sharing once MSR is met or exceeded No change Same as Track 1 No change Same as Tracks 1 and 2. Shared Loss Rate Not applicable No change One minus final sharing rate applied to first dollar losses once minimum loss rate is met or exceeded; shared loss rate not to exceed 60 percent No change One minus final sharing rate applied to first dollar losses once minimum loss rate is met or exceeded; shared loss rate may not be less than 40 percent or exceed 75 percent. Loss Sharing Limit Not applicable No change Limit on the amount of losses to be shared in phases in over 3-years starting at 5 percent in year 1; 7.5 percent in year 2; and 10 percent in year 3 and any subsequent year. Losses in excess of the annual limit would not be shared No change 15 percent. Losses in excess of the annual limit would not be shared. G. Additional Program Requirements and Beneficiary Protections
1. Background
Section 1899(a)(1)(A) of the Act authorizes the Secretary to specify criteria that ACOs must satisfy in order to be eligible to participate in the Shared Savings Program. In the November 2011 final rule, we finalized policies regarding how ACOs will be monitored with respect to program requirements and what actions will be taken against ACOs that are not in compliance with the requirements of the Shared Savings Program. Based on our initial experience with the Shared Savings Program, we propose several refinements and clarifications to our policies on—
- Public reporting (§ 425.308);
- Termination of the participation agreement (§§ 425.218 and 425.220);
- Enforcement of ACO compliance with quality performance standards (§ 425.316(c)); andStart Printed Page 72846
- Reconsideration review procedures (§§ 425.802 and 425.804)).
2. Public Reporting and Transparency
a. Overview
Section 1899 of the Act sets forth a number of requirements for ACOs. Section 1899(b)(2)(H) of the Act requires ACOs to demonstrate that they meet patient-centeredness criteria specified by the Secretary. We believe that one important aspect of patient-centeredness is patient engagement and transparency. Increasingly, transparency of information in the health care sector is seen as a means to help patients become more active in their health care choices and to generate feedback that may improve the quality of care and lower the cost of care. In addition, transparency may improve oversight and program integrity. Public reporting also supports the mandate for ACOs to be willing to “become accountable for the quality, cost, and overall care” of the Medicare beneficiaries assigned to them. Reports on ACO quality and cost-performance hold ACOs accountable and contribute to the dialogue on how to drive improvement and innovation in health care. Public reporting of ACO cost and quality data may improve a beneficiary's ability to make informed health care choices and facilitate an ACO's ability to improve the quality and efficiency of its care.
Therefore, for these reasons, which are described in more detail in the November 2011 final rule, we finalized requirements specified at § 425.308 that ACOs must make certain information publicly available. Since publication of the Shared Savings Program final rule, minor updates were made to § 425.308(e) in the 2013 PFS final rule with comment period (77 FR 69164 through 69170) and in the 2015 PFS final rule with comment period (79 FR 67769). For purposes of the Shared Savings Program, each ACO is currently required at § 425.308 to publicly report certain organizational information (such as the identification of ACO participants and governing body members), the amount of any shared savings or shared losses incurred, the proportion of shared savings invested in resources that support the three-part aim and certain quality performance information. (Specifically, ACOs are required to report the results of the claims-based quality measures while CMS will report the CAHPS and GPRO measure results on Physician Compare.) We recommend that ACOs publicly report the specified information in a standardized format that we have made available to ACOs through guidance at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Statutes_Regulations_Guidance.html. Our guidance recommended that ACOs report the required information on a Web site that complies with the marketing requirements set forth at § 425.310. Because Web pages used to publicly report the information specified in § 425.308 constitute “marketing materials and activities,” as defined at § 425.20, any changes to such Web pages must be submitted for CMS review in accordance with § 425.310. Thus, if an ACO changes any of the information on its public reporting Web page, such as adding an ACO participant or replacing a member of the governing body, the ACO must submit its Web page to us for marketing review. We believe this policy creates undue burden on the ACO as well as on CMS.
b. Proposed Revisions
We continue to believe that publicly reporting the information identified in § 425.308 supports our goals of program transparency and patient centeredness. We also continue to believe that it is important for the ACO to be responsible for making this information available to the public. We believe that the best way to do this is via an ACO-maintained Web site, the mechanism through which most ACOs have chosen to publicly report. However, based on our initial experience with the Shared Savings Program and requests from some ACOs, we propose some refinements to the requirements related to public reporting and transparency.
We propose to modify § 425.308 to reflect these new requirements. In § 425.308(a), we propose to require that each ACO maintain a dedicated Web page on which the ACO must publicly report the information listed in paragraph (b). In addition, we propose that an ACO must report to us the address of the Web page on which it discloses the information set forth in § 425.308 and apprise us of changes to that Web site address in the form and manner specified by CMS. We solicit comment on when an ACO should be required to inform us of such changes (for example, within 30 days after the change has occurred).
In § 425.308(b), we require ACOs to report certain information in a standardized format to be specified by CMS. Although we currently set forth a recommended standardized format in guidance, we intend to make a specific template available that ACOs must use so that ACOs report information uniformly. This would minimize the compliance burden on ACOs, enhance transparency for the public, and improve our oversight of ACO compliance with the public reporting requirement. We envision that the template would have fields in which the ACO must insert the applicable public reporting information. Additionally, because the ACOs would report information using a standard template, we do not believe the information would require marketing review each time the information is updated. Therefore, we propose in § 425.308(c) that information reported on an ACO's public reporting Web page which is in compliance with the requirements of the standardized format specified by CMS, (that is, through use of the template) is not subject to marketing review and approval under § 425.310. ACOs should keep in mind that although information reported using the template would not be subject to marketing review, we intend to monitor both the use of the template and the information inserted by ACOs into the template as part of our ongoing program monitoring and compliance oversight efforts.
Using a standardized format, such as a template, for this purpose has several advantages over the way ACOs currently make this information publicly available. First, using a template would improve the usefulness of this information for the public by standardizing the way the information is made available across ACOs. Second, using a template would minimize the compliance burden on ACOs by ensuring the information is reported in the way we intend. Finally, the use of a standardized format also affords CMS a more streamlined approach for our monitoring and compliance oversight activities. We seek comment on the proposal to use a standardized format for public reporting purposes.
We also propose to make a few changes to the information that must be publicly reported. In § 425.308(b), we propose to add two categories of organizational information that must be publicly reported. First, we propose to add a requirement at § 425.308(b)(3)(iv) that ACOs publicly identify key clinical and administrative leaders within their organization as part of the public reporting requirements. ACOs are already required to identify the members of their governing body, associated committees and committee leadership. However, key members of the ACO's clinical and administrative leadership might not be members of the governing body or committee leadership. For example, the ACO's medical director may be a stand-alone leadership position but not hold a committee leadership position or be a Start Printed Page 72847member on the ACO's governing body. Because clinical and administrative leadership is an eligibility requirement for program participation, we believe that requiring the ACO to publicly report its clinical and administrative leadership would lend additional transparency and insight into the ACO's organization.
Second, we believe it would be helpful for the public to have a better understanding of the types of ACO participants or combinations of ACO participants that have joined to form the ACO. At § 425.102(a), we articulate the following types of ACO participants or combinations of ACO participants that are eligible to form an ACO:
- ACO professionals in group practice arrangement.
- Networks of individual practices of ACO professionals.
- Partnerships or joint venture arrangements between hospitals and ACO professionals.
- Hospitals employing ACO professionals.
- CAHs that bill under Method II.
- RHCs and FQHCs.
We note that if revised by our proposals in section II.E. of this proposed rule, this list would also include teaching hospitals. On the application to the Shared Savings Program, each ACO must indicate the types of entities that formed the ACO. We propose to add a provision at § 425.308(b)(3)(vi) requiring ACOs to publicly report the types of ACO participants or combinations of ACO participants, as listed in § 425.102(a), that form the ACO. Stakeholders have requested information about the composition of ACOs. Providing the types and combinations of ACO participants would assist stakeholders in understanding the composition of ACOs.
In addition, we propose at § 425.308(b)(5) to require each ACO to publicly report its performance on all quality measures used to assess the quality of care furnished by the ACO. We currently require ACOs to post only the results of their performance on claims-based measures. The results of quality measures are reported by CMS on Physician Compare. We agree with the comments made by stakeholders that requiring an ACO to publicly report its performance on all quality measures (as defined at § 425.20) would assist stakeholders in getting a more accurate picture of the ACO's performance. Therefore, we propose to broaden the public reporting requirement to require ACOs to publicly report performance on all quality measures.
We also note a technical modification to our rules. Currently, we require ACOs to report the amount of any “shared savings performance payment” (§ 425.308(d)(1)). However, to conform this provision to the definition of “shared savings” at § 425.20, we propose to remove the term “performance payment” from the phrase. The new language is found at revised § 425.308(b)(4)(i).
Finally, for purposes of program transparency, we find it useful to post on Physician Compare and our Web site (www.cms.gov/sharedsavingsprogram/) certain information about ACOs, such as ACO public contact information, ACO public reporting Web page addresses, the amount of any shared savings or losses incurred, and quality performance results. Therefore, in addition to information we already post on our Web site and Physician Compare, we propose at § 425.308(d) to post ACO-specific information, including information the ACO is required to publicly report under § 425.308, as is necessary to support program goals and transparency. We solicit comment on what other information should be published on our Web site. Because proposed § 425.308(d) encompasses our ability to publicly report ACO performance on all quality measures, we propose to remove § 425.308(e) or reserve it for future use. We intend to continue reporting ACO quality measure performance on Physician Compare in the same way as for group practices that report under PQRS.
3. Terminating Program Participation
a. Overview
Section 425.218 of our regulations sets forth the grounds for terminating an ACO for failure to comply with the requirements of the Shared Savings Program (§ 425.218(a)). For example, an ACO's or ACO participant's failure to notify beneficiaries of their provider's participation in the program as required under § 425.312 would constitute grounds for terminating the ACO. In addition, we may terminate an ACO for a number of other violations, such as those related to certain fraud and abuse laws, the antitrust laws, or other applicable Medicare laws and regulations relevant to ACO operations, or if certain sanctions have been imposed on the ACO by an accrediting organization or a federal, state or local government agency (§ 425.218(b)).
Prior to termination, we may take interim steps such as issuing the ACO a warning notice or placing the ACO on a corrective action plan (CAP) (§ 425.216). However, we reserve the right to immediately terminate a participation agreement if necessary (§ 425.218(c)). We notify the ACO in writing if the decision is made to terminate the participation agreement.
Under § 425.220, an ACO may voluntarily terminate its participation agreement. Such an ACO is required to provide CMS and all of its ACO participants with a 60-day advance written notice of its decision to terminate its participation in the Shared Savings Program. An ACO is not required to notify beneficiaries of the ACO's decision to terminate from the Shared Savings Program. Under current regulations, an ACO that terminates its participation agreement before completion of the participation agreement does not share in any savings for the performance year during which it notifies CMS of its decision to terminate the participation agreement (§ 425.220(b)). This is because an ACO that terminates its participation agreement during a performance year will have failed to complete the entire performance year and will therefore have failed to meet the requirements for shared savings.
b. Proposed Revisions
We propose several modifications to the regulations related to termination of a participation agreement. First, we propose to permit termination for failure to timely comply with requests for documents and other information and for submitting false or fraudulent data. In addition, we propose to add a new regulation at § 425.221 requiring ACOs to implement certain close-out procedures upon termination and nonrenewal. Finally, we propose to address in new § 425.221 the payment consequences upon termination of a participation agreement.
(1) Grounds for Termination
First, at § 425.218(b) we propose to modify the grounds for termination to specifically include the failure to comply with CMS requests for submission of documents and other information by the CMS specified deadline. At times, we may request certain information from the ACO in accordance with program rules. The submission of those documents by the specified due date is important for program operations. For example, we require each ACO to submit to us, on an annual basis, its list of ACO participants and their TINs (existing § 425.304 and proposed § 425.118). When ACOs do not submit these lists by the due date specified, it prevents us from applying the assignment methodology (which is dependent on having accurate lists of Start Printed Page 72848ACO participants for all ACOs) and impacts the timelines for the program, such as the calculation of the benchmarks for all ACOs. Missing such deadlines is very disruptive to the program and other ACOs. Therefore, we propose to modify § 425.218(b) to permit termination of an ACO agreement for failure to comply with requests for information and documentation by the due date specified by CMS.
Additionally, under § 425.302, an individual with the authority to legally bind the individual or entity submitting data or information to CMS must certify the accuracy, completeness, and truthfulness of the data and information to the best of his or her knowledge and belief. However, circumstances could arise in which the data and information submitted was falsified or erroneous. Submission of false or fraudulent data, (for example, data submitted through the CMS web interface used to determine an ACO's quality performance) could impact the amount of shared savings calculated for the ACO and cause CMS to overpay the ACO. Because of the severity of the consequences of submitting false or fraudulent data, we propose to modify § 425.218(b) to permit termination of an ACO agreement for submission of false or fraudulent data. We note that ACOs are obligated to repay shared savings payments to which they are not entitled, including, by way of example only, any overpayment to the ACO based on the submission of false or fraudulent data.
(2) Close-Out Procedures and Payment Consequences of Early Termination
We propose to add new § 425.221 to address close-out procedures and payment consequences of early termination. First, we believe it is important to establish an orderly close-out process when an ACO's participation agreement is terminated. Therefore, we are proposing in § 425.221(a) that an ACO whose participation agreement is terminated prior to its expiration either voluntarily or by CMS must implement close-out procedures in a form, manner, and deadline specified by CMS. These close-out procedures shall address data sharing issues such as data destruction, beneficiary notification issues (for example removal of marketing materials and ensuring beneficiary care is not interrupted), compliance with quality reporting, record retention issues, and other issues established through guidance. We note that the close-out procedures would also apply to those ACOs that have elected not to renew their agreements upon expiration of the participation agreement. We further propose in § 425.221(a)(2) that any ACO that fails to complete the close-out procedures in the form and manner and by the deadline specified by CMS would not be eligible for shared savings. We solicit comments on other strategies that would ensure compliance with close-out procedures.
Second, we propose in § 425.221(b) to address certain payment consequences of early termination. Currently under § 425.220(b), an ACO that voluntarily terminates its agreement at any time during a performance year will not share in any savings for the performance year during which it notifies CMS of its decision to terminate the participation agreement. However, stakeholders have suggested that completion of the performance year, as part of an orderly close-out process, could be mutually beneficial to the ACO, its ACO participants and ACO providers/suppliers, and to CMS. Specifically, stakeholders have suggested that an ACO should be entitled to receive shared savings if the ACO completes a performance year through December 31 and satisfies all requirements for sharing in savings for that performance year (for example, the quality reporting for the performance year). Additionally, by completing quality reporting as part of the close-out process, the ACO participants would not be penalized by the ACO's decision to terminate its participation agreement. For example, eligible professionals that bill through the TIN of an ACO participant could satisfy the reporting requirement to avoid the downward payment adjustment under the PQRS in a subsequent year.
Therefore, we propose in § 425.221(b) to permit an ACO whose participation agreement is voluntarily terminated by the ACO under § 425.220 to qualify for shared savings, if—
- The effective date of termination is December 31; and
- By a date specified by CMS, it completes its close-out process for the performance year in which the termination becomes effective.
In order to effectively manage this option in the case of voluntary termination, the ACO must specify in its termination notice, and CMS must approve, a termination effective date of December 31 for the current performance year. Because the proposed new provision at § 425.221 will address the consequences of termination, including the payment consequences, we also propose to make a conforming change to § 425.220 to remove paragraph (b) addressing the payment consequences of early termination.
We note that the opportunity to share in savings for a performance year would not extend to ACOs that terminate their participation agreement with effective dates prior to December 31 or to ACOs that CMS terminates under § 425.218. Those ACOs that terminate prior to December 31 will not have completed the performance year and thus would not qualify for shared savings. ACOs terminated by CMS under § 425.218 would not qualify for shared savings irrespective of the termination date because maintaining eligibility to participate in the Shared Saving Program is a pre-requisite for sharing in savings (see §§ 425.604(c) and 425.606(c)). In such cases, we strongly encourage ACOs to fulfill their obligations to their ACO participants and ACO providers/suppliers by reporting quality for the performance year in which it terminates so that their ACO participants and ACO providers/suppliers are not unduly penalized by the ACO's decision. However, even if the ACO completes quality reporting on behalf of its ACO participants and ACO provider/suppliers, if the ACO terminates its participation midyear or is terminated by CMS under § 425.218 (prior to December 31), it would not be eligible to share in savings for the performance year. The ACO would not be eligible to share in savings because the ACO would not have satisfied all requirements for sharing in savings for that performance year.
(3) Reconsideration Review Process
(A) Overview
Under § 425.802(a), an ACO may appeal an initial determination that is not subject to the statutory preclusion on administrative or judicial review (see section 1899(g) of the Act). Specifically, the following determinations are not subject to administrative or judicial review:
- The specification of quality and performance standards under §§ 425.500 and 425.502.
- The assessment of the quality of care furnished by an ACO under the performance standards.
- The assignment of beneficiaries.
- The determination of whether the ACO is eligible for shared savings and the amount of such shared savings (including the determination of the estimated average per capita Medicare expenditures under the ACO for beneficiaries assigned to the ACO and the average benchmark for the ACO).
- The percent of shared savings specified by the Secretary and the limit on the total amount of shared savings established under §§ 425.604 and 425.606.Start Printed Page 72849
- The termination of an ACO for failure to meet the quality performance standards.
Initial determinations that are not precluded from administrative or judicial review would include the denial of an ACO application or the involuntary termination of an ACO's participation agreement by CMS.
Under § 425.802(a), an ACO may appeal an initial determination that is not prohibited from administrative or judicial review by requesting reconsideration review by a CMS official. The request for review must be submitted for receipt by CMS within 15 days of the notice of the initial determination. Section 425.802(a)(2) provides that reconsiderations may be heard orally (that is, in person, by telephone or other electronic means) or on the record (review of submitted documentation) at the discretion of the reconsideration official.
(B) Proposed Changes
To date, CMS reconsideration official(s) have reviewed all reconsideration requests received as on-the-record reviews. We believe that on-the-record reviews are fair to both parties. Experience to date has demonstrated that a robust oral review is not necessary in light of the narrow scope of review. The issues eligible for review can be easily communicated in a detailed writing by both parties and do not require in-person witness testimony. Finally, we believe that on-the-record reviews do not require as many agency resources and can therefore ensure that decisions are made in a timely manner.
Accordingly, we propose to modify § 425.802 to permit only on-the-record reviews of reconsideration requests. Additionally, we propose to similarly modify § 425.804 and also clarify that the reconsideration process allows both ACOs and CMS to submit one brief each in support of its position by the deadline established by the CMS reconsideration official.
4. Monitoring ACO Compliance With Quality Performance Standards
We propose a technical revision to § 425.316(c) to clarify our administrative enforcement authority when ACOs fail to meet the quality reporting requirements. Specifically, we propose to remove § 425.316(c)(3), which sets forth various required actions the ACO must perform if it fails to report one or more quality measures or fails to report completely and accurately on all measures in a domain. We also propose to remove § 425.316(c)(4), which sets forth the administrative action we may take against an ACO if it exhibits a pattern of inaccurate or incomplete reporting of quality measures or fails to make timely corrections following notice to resubmit. The actions identified in § 425.316(c)(3) and (4) include request for missing or corrected information, request for a written explanation for the noncompliance, and termination. All of these actions are already authorized under § 425.216 and § 425.218. Therefore, to reduce redundancy, prevent confusion, and to streamline our regulations, we propose to modify § 425.316(c) to remove § 425.316(c)(3) and (c)(4).
In addition, we propose a technical change to § 425.316(c)(5), which currently provides that an ACO “will not qualify to share in savings in any year it fails to report fully and completely on the quality performance measures.” We propose to redesignate this paragraph as § 425.316(c)(3) and replace “fully and completely” with “accurately, completely, and timely” to align with § 425.500(f) and to emphasize the importance of timely submission of measures.
III. Collection of Information Requirements
As stated in section 3022 of the Affordable Care Act, Chapter 35 of title 44, United States Code, shall not apply to the Shared Savings Program. Consequently, the information collection requirements contained in this proposed rule need not be reviewed by the Office of Management and Budget.
IV. Response to Comments
Because of the large number of public comments we normally receive on Federal Register documents, we are not able to acknowledge or respond to them individually. We will consider all comments we receive by the date and time specified in the DATES section of this proposed rule, and, when we proceed with a subsequent document, we will respond to the comments in the preamble to that document.
V. Regulatory Impact Analysis
A. Statement of Need
This proposed rule is necessary to propose payment and policy changes to the Medicare Shared Savings Program established under section 1899 of the Act. The Shared Savings Program promotes accountability for a patient population, coordinates items and services under parts A and B, and encourages investment in infrastructure and redesigned care processes for high quality and efficient service delivery.
B. Overall Impact
We have examined the impacts of this rule as required by Executive Order 12866 on Regulatory Planning and Review (September 30, 1993), Executive Order 13563 on Improving Regulation and Regulatory Review (January 18, 2011), the Regulatory Flexibility Act (RFA) (September 19, 1980, Pub. L. 96-354), section 1102(b) of the Social Security Act, section 202 of the Unfunded Mandates Reform Act of 1995 (March 22, 1995; Pub. L. 104-4), Executive Order 13132 on Federalism (August 4, 1999) and the Congressional Review Act (5 U.S.C. 804(2)).
Executive Orders 12866 and 13563 direct agencies to assess all costs and benefits of available regulatory alternatives and, if regulation is necessary, to select regulatory approaches that maximize net benefits (including potential economic, environmental, public health and safety effects, distributive impacts, and equity). Section 3(f) of Executive Order 12866 defines a “significant regulatory action” as an action that is likely to result in a rule: (1) Having an annual effect on the economy of $100 million or more in any 1 year, or adversely and materially affecting a sector of the economy, productivity, competition, jobs, the environment, public health or safety, or state, local or tribal governments or communities (also referred to as “economically significant”); (2) creating a serious inconsistency or otherwise interfering with an action taken or planned by another agency; (3) materially altering the budgetary impacts of entitlement grants, user fees, or loan programs or the rights and obligations of recipients thereof; or (4) raising novel legal or policy issues arising out of legal mandates, the President's priorities, or the principles set forth in the Executive Order.
A regulatory impact analysis (RIA) must be prepared for major rules with economically significant effects ($100 million or more in any 1 year). We estimate that this rulemaking is “economically significant” as measured by the $100 million threshold, and hence also a major rule under the Congressional Review Act. Accordingly, we have prepared a Regulatory Impact Analysis, which to the best of our ability presents the costs and benefits of the rulemaking.
C. Anticipated Effects
1. Effects on the Medicare Program
The Shared Savings Program is a voluntary program involving an innovative mix of financial incentives Start Printed Page 72850for quality of care and efficiency gains within FFS Medicare. As a result, the changes being proposed to the Shared Savings Program could result in a range of possible outcomes. In previous rulemaking (76 FR 67904), we indicated that participation in Track 1 might enable ACOs to gain the experience necessary to take on risk in a subsequent agreement period under a two-sided arrangement, possibly enhancing the opportunity for greater program savings in years beyond the first agreement period. Conversely, if in that first agreement period, ACOs come to reliably predict a bias that ensures an outcome—whether favorable or unfavorable—the program would be at risk for increasingly selective participation from favored ACOs and any real program savings could be overwhelmed by outsized shared-savings payments (76 FR 67964). Further, even ACOs that opt for a two-sided arrangement could eventually terminate their agreements if they anticipate that efforts to improve efficiency are overshadowed by their particular market circumstances. This scenario could also contribute to selective program participation by ACOs favored by the national flat-dollar growth target, or favored by other unforeseen biases affecting performance.
However, as we indicated in the previous rulemaking, even with the optional liability for a portion of excess expenditures, which offers less incentive to reduce costs than a model involving full capitation, the opportunity to share in FFS Medicare savings still represents an incentive for efficiency. The actual effects of shared savings (and potential liabilities in the form of shared losses) will have varying degrees of influence on hospitals, primary care physicians, specialty physicians, and other providers and suppliers. Moreover, while certain care improvements might be achieved relatively quickly (for example, prevention of hospital readmissions and emergency-room visits for certain populations with chronic conditions), some ACOs might need more than 3 years to achieve comprehensive efficiency gains.
As of the spring of 2014, over 330 organizations have chosen to participate in the Shared Savings Program. These organizations care for nearly 5 million assigned FFS beneficiaries living in 47 states, plus Puerto Rico and the District of Columbia. Half of all ACOs characterize themselves as networks of individual practices and the other half include hospitals. In the fall of 2014, CMS announced the final financial reconciliation and quality performance results for performance year 1 for ACOs with 2012 and 2013 agreement start dates. Of the 220 ACOs with 2012 and 2013 start dates, 58 ACOs generated shared savings during their first performance year. They held spending $705 million below their targets and earned shared savings payments of more than $315 million as their share of program savings. One ACO in Track 2 overspent its target by $10 million and owed shared losses of $4 million. Total net savings to Medicare is close to $383 million, including repayment of shared losses by one Track 2 ACO. An additional 60 ACOs reduced health costs compared to their benchmark, but did not qualify for shared savings, as they did not meet the minimum savings threshold. While evaluation of the program's overall impact is ongoing, the performance year 1 final financial reconciliation and quality results are within the range originally projected for the program's first year. Also, at this point, we have seen no evidence of systematic bias in ACO participation or performance that would raise questions about the savings that have been achieved.
Earlier in this proposed rule, we proposed additions to or changes in policy that are intended to better encourage ACO participation in risk-based models by—
- Easing the transition from Track 1 to Track 2;
- Reducing risk under Track 2; and
- Adopting an alternative risk-based model—Track 3.
First, as is currently the case, an ACO would be able to apply to participate in Track 1 for its initial agreement period during which the ACO could be eligible for shared savings payments in all 3 performance years of the agreement period without the risk of being responsible for repayment of any losses if actual expenditures exceed the benchmark. However, rather than requiring all Track 1 ACOs to transition to a risk-based model in their second agreement period, as is currently required, we are proposing to improve the transition from the shared-savings only model to a risk-based model for Track 1 ACOs that might require additional experience with the program before taking on performance-based risk. Specifically, in this proposed rule, we are proposing that Track 1 ACOs may elect to continue participation under Track 1 for a subsequent agreement period, albeit with a lower sharing rate, provided that they meet the eligibility requirements to continue in the program under Track 1.
Second, we are proposing to reduce the current level of risk for ACOs that participate in Track 2, which provides an opportunity for an ACO to receive a higher percentage of shared savings for all years of the agreement period, but with potential liability for shared losses in each of the agreement years if annual expenditures exceed the benchmark. Specifically, in this proposed rule, we are proposing to replace the current flat 2 percent MSR and MLR under Track 2 with a variable MSR and MLR using the same methodology as is currently used to establish the MSRs for ACOs under Track 1. Under this methodology an ACO's MSR varies based on the number of assigned beneficiaries using a sliding scale. Similarly, we are proposing to vary a Track 2 ACO's MSR and MLR based on the number of assigned beneficiaries. This proposal would reduce risk for many Track 2 ACOs by increasing the threshold before they would have to share in additional costs that they had incurred for the program.
Third, in this proposed rule, we are proposing to establish an additional risk-based option (Track 3) that offers a higher maximum shared savings percentage (75 percent) and performance payment limit (20 percent) than is available under Track 2 (60 percent and 15 percent respectively), a fixed MSR and MLR of 2 percent, and a cap on the amount of losses for which an ACO is liable that is fixed at 15 percent of its updated benchmark in each year. Also, under this model, beneficiaries would be assigned prospectively so an ACO would know in advance those beneficiaries for which it would be responsible.
As detailed in Table 8, we estimate at baseline (that is, without the proposed changes detailed in this proposed rule) a total aggregate median impact of $730 million in net federal savings for calendar years (CY) 2016 through 2018 from the continued operation of the Shared Savings Program for ACOs electing a second agreement period starting in January 2016. The 10th and 90th percentiles of the estimate distribution, for this same time period, yield a net savings of $380 million and $1,160 million, respectively. These estimated impacts represent the effect on federal transfers of payments to Medicare providers and suppliers. The median estimated federal savings are higher than the estimate for the program effects over the preceding calendar years (CY) 2012 through 2015 published in the previous final rule (estimated median net savings of $470 million for such 4 year period). This increase in savings is due to multiple factors related to maturation of the program, including continued phase-in of assumed savings potentials, lowered effective sharing Start Printed Page 72851rates due in part to rebased benchmarks, and increased collection of shared losses due to mandatory enrollment in Track 2 in a second agreement period. However, absent changes to improve the viability of participation for ACOs considering a second agreement period, we estimate fewer than one in four ACOs will opt for continued participation under downside risk in Track 2 as required under the current regulations. Further, we estimate approximately one in three of such re-enrolling ACOs would ultimately drop out of the program by 2018 to avoid future shared loss liability.
Alternatively, as detailed in Table 9, by including the proposed changes detailed in this rule, the total aggregate median impact would increase to $1,010 million in net federal savings for calendar years (CY) 2016 through 2018. The 10th and 90th percentiles of the estimate distribution, for the same time period, would also be higher, yielding net savings of $430 million and $1,650 million, respectively. Such median estimated federal savings are $280 million greater than the $730 million median net savings estimated at baseline absent proposed changes. A key driver of an anticipated increase in net savings is through improved ACO participation levels in a second agreement period. We estimate that at least 90 percent of eligible ACOs will renew their participation in the Shared Savings Program if presented with the new options, primarily under Track 1 and, to a lesser extent, under Track 3. This expansion in the number of ACOs willing to continue their participation in the program is estimated to result in additional improvements in care efficiency of a magnitude significantly greater than the reduced shared loss receipts estimated from baseline (median shared loss dollars reduced by $140 million relative to baseline) and the added shared savings payments flowing from a higher sharing rate in Track 3 and continued one-sided sharing available in Track 1 (median shared savings payments increased by $320 million relative to baseline).
With respect to costs incurred by ACOs, as discussed later in this section, for purposes of this analysis, we are retaining our assumption included in our November 2011 final rule (76 FR 67969) of an average of $0.58 million for start-up investment costs but are revising our assumption for average ongoing annual operating costs for an ACO participating in the Shared Savings Program to $0.86 million, down from the $1.27 million assumed in our November 2011 final rule (76 FR 67969). This revision is related to the lower average number of beneficiaries currently observed to be assigned to existing Shared Savings Program ACOs compared to the larger organizations participating in the Physician Group Practice Demonstration upon which the original assumption was based. We also believe that our proposals to streamline the administrative requirements for the program could further assist in lowering administrative costs.
For our analysis, we are comparing the effects of the proposed changes in this proposed rule for a cohort of ACOs that either continued their participation, beginning in 2016 or newly began participation in that same year. For purposes of our analysis, we assume that roughly one quarter of ACOs will incur aggregate start-up investment costs in 2016, ranging from $7 million under the baseline scenario to $30 million under the alternative (all proposed changes) scenario in aggregate. Aggregate-ongoing operating costs are estimated to range from $43 million under the baseline scenario to $181 million under the alternative scenario. Both start-up investment and ongoing operating cost ranges assume an anticipated average participation level of 50 (baseline scenario) to 210 (alternative scenario) new or currently participating ACOs that establish or renew participation agreements in 2016. For purposes of this analysis, we assume that some portion of ACOs currently participating in the program will not renew their participation agreement for a subsequent agreement period. As a result, under our baseline scenario, we assume 50 ACOs will either renew or begin an agreement period in 2016—far fewer than the 100 new ACOs that have entered the program in each of the last 2 years. The 3-year aggregate ongoing operating cost estimate also reflects our assumption that, under the baseline scenario, there would be a greater propensity for ACOs that have completed the full term of their initial agreement period, and that would be required to participate under Track 2 in their second agreement period, to drop out of the program after receiving poor results from their final settlement for the first performance year under Track 2 in the new agreement period. Therefore, as illustrated in Table 8 for the baseline scenario, for CYs 2016 through 2018, total median ACO shared savings payments of $310 million offset by $170 million in shared losses coupled with the aggregate average start-up investment and ongoing operating cost of $121 million result in an estimated net private benefit of $19 million. Alternatively, as illustrated in Table 9 for the all changes scenario, for CYs 2016 through 2018 the total median ACO shared savings payments of $630 million, offset by $30 million in shared losses, coupled with the aggregate average start-up investment and ongoing operating costs of $562 million, result in an estimated net private benefit of $38 million. By proposing to no longer require ACOs to accept risk in their second agreement period, our proposed changes also provide the benefit of reducing the per-ACO average shared loss liability by over 95 percent compared to the baseline. Therefore, the proposed changes would likely prevent a significant number of ACOs that would renew their participation agreements in 2016 from leaving the program prior to 2018.
By encouraging greater Shared Savings Program participation, the changes proposed in this rule will also benefit beneficiaries through broader improvements in accountability and care coordination than would occur under current regulations. Accordingly, we have prepared a regulatory impact analysis (RIA) that to the best of our ability presents the costs and benefits of this proposed rule.
Table 8—Baseline (Absent All Proposed Changes) Estimated Net Federal Savings, Costs and Benefits, CYs 2016 Through 2018
CY 2016 CY 2017 CY 2018 CYs (2016-2018) Net Federal Savings: 10th Percentile $200 million $150 million $20 million $380 million. Median $340 million $270 million $110 million $730 million. 90th Percentile $510 million $430 million $240 million $1160 million. ACO Shared Savings: 10th Percentile $40 million $60 million $70 million $180 million. Median $80 million $110 million $120 million $310 million. Start Printed Page 72852 90th Percentile $130 million $170 million $190 million $480 million. ACO Shared Losses: 10th Percentile $20 million $40 million $10 million $80 million. Median $60 million $80 million $30 million $170 million. 90th Percentile $100 million $150 million $60 million $290 million. Costs The estimated aggregate average start-up investment and 3-year operating costs is $121 million. The total estimated start-up investment costs average $7 million, with ongoing costs averaging $43 million, for the anticipated mean baseline participation of 50 ACOs. Benefits Improved healthcare delivery and quality of care and better communication to beneficiaries through patient-centered care. * Note that the percentiles for each individual year do not necessarily sum to equal the corresponding percentiles estimated for the total 3-year impact, in the column labeled CYs 2016 through 2018, due to the annual and overall distributions being constructed independently. Table 9—Alternative Scenario Assuming All Proposed Changes Estimated Net Federal Savings, Costs and Benefits, CYs 2016 Through 2018
CY 2016 CY 2017 CY 2018 CYs (2016-2018) Net Federal Savings: 10th Percentile $190 million $150 million $80 million $430 million. Median $380 million $350 million $280 million $1,010 million. 90th Percentile $590 million $570 million $510 million $1650 million. ACO Shared Savings: 10th Percentile $90 million $150 million $220 million $470 million. Median $140 million $210 million $280 million $630 million. 90th Percentile $200 million $280 million $350 million $820 million. ACO Shared Losses: 10th Percentile $0 million $0 million $0 million $10 million. Median $10 million $20 million $0 million $30 million. 90th Percentile $30 million $40 million $20 million $70 million. Costs The estimated aggregate average start-up investment and 3-year operating costs is $562 million. The total estimated start-up investment costs average $30 million, with ongoing costs averaging $181 million, for the anticipated mean baseline participation of 210 ACOs. Benefits Improved healthcare delivery and quality of care and better communication to beneficiaries through patient-centered care. Note that the percentiles for each individual year do not necessarily sum to equal the corresponding percentiles estimated for the total 3-year impact in the column labeled CYs 2016 through 2018, due to the annual and overall distributions being constructed independently. Also, the cost estimates for this table reflect our assumptions for increased ACO participation as well as changes in the mix of new and continuing ACOs. There remains uncertainty as to the number of ACOs that will continue to participate in the program, provider and supplier response to the financial incentives offered by the program in the medium and long run, and the ultimate effectiveness of the changes in care delivery that may result as ACOs work to improve the quality and efficiency of patient care. These uncertainties continue to complicate efforts to assess the financial impacts of the Shared Savings Program and result in a wide range of potential outcomes regarding the net impact of the proposed changes in this proposed rule on Medicare expenditures.
To best reflect these uncertainties, we continue to utilize a stochastic model that incorporates assumed probability distributions for each of the key variables that will affect the overall financial impact of the Shared Savings Program. Using a Monte Carlo simulation approach, the model randomly draws a set of specific values for each variable, reflecting the expected covariance among variables, and calculates the program's financial impact based on the specific set of assumptions. We repeated the process for a total of 2,500 random trials, tabulating the resulting individual cost or savings estimates to produce a distribution of potential outcomes that reflects the assumed probability distributions of the incorporated variables, as shown in Table 9. In this way, we can evaluate the full range of potential outcomes based on all combinations of the many factors that will affect the financial impact, and with an indication of the likelihood of these outcomes. It is important to note that these indications do not represent formal statistical probabilities in the usual sense, since the underlying assumptions for each of the factors in the model are based on reasonable judgments, using independent expert opinion when available.
The median result from the distribution of simulated outcomes represents the “best estimate” of the financial effect of the proposed changes to the Shared Savings Program. The full distribution illustrates the uncertainty surrounding the mean or median financial impact from the simulation.
The median estimate involves a combination of—
- Reduced actual Medicare expenditures due to more efficient care;
- Shared savings payments to ACOs; and
- Payments to CMS for shared losses when actual expenditures exceed the Start Printed Page 72853benchmark, resulting in a projected total of $1,010 million in net savings over CYs 2016 through 2018, or $280 million greater than the median projected total at baseline without the changes proposed in this rule.
This net Federal savings estimate, detailed at the top of Table 9, can be summed with the projected ACO shared savings less projected ACO shared losses—both also detailed in Table 9—to show the median expected effect on Medicare claim expenditures before accounting for shared savings payments (that is, the reduction in actual Medicare expenditures due to more efficient care).
A net savings (cost) occurs when payments of earned and unearned shared savings (less shared losses collected) resulting from: (1) Reductions in spending; (2) care redesign; and (3) random group claim fluctuation, in total are less than (greater than) assumed savings from reductions in expenditures.
As continued emerging data become available on the differences between actual expenditures and the target expenditures reflected in ACO benchmarks, it may be possible to evaluate the financial effects with greater certainty. The estimate distribution shown in Table 10 provides an objective and reasonable indication of the likely range of financial outcomes, given the chosen variables and their assumed distributions at this time in the program's operation.
a. Assumptions and Uncertainties
We continue to rely on input gathered as part of the analysis for the existing regulation from a wide range of external experts, including credentialed actuaries, consultants, and academic researchers, to identify the pertinent variables that could determine the efficacy of the program, and to identify the reasonable ranges for each variable. We also continue to monitor emerging evidence from current participation in this program, the Pioneer ACO Model, and related published evidence where available. The factors that we are continuing to consider for modeling include all of the following:
- Number of participating ACOs, including the sensitivity to burdens of participation and the generosity of the sharing arrangement.
- Size mix of participating ACOs.
- Type of ACO that would consider accepting risk.
- Participating ACOs' current level of integration and preparedness for improving the quality and efficiency of care delivery.
- Baseline per-capita costs for ACOs, relative to the national average.
- Number and profile of providers and suppliers available to participate in the Shared Savings Program as a result of Innovation Center model initiatives.
- Range of gross savings achieved by ACOs, and the time required for full phase-in.
- Local variation in expected claims cost growth relative to the national average.
- Quality reporting scores and resulting attained sharing (or loss) percentages.
- Potential 'spillover' effects between the Shared Savings Program and other value-based incentive programs implemented by CMS and/or other payers.
We assumed that overall between 0.8 million Medicare beneficiaries (under baseline) and 3.3 million Medicare beneficiaries (with all proposed changes) would annually be assigned to between 50 and 210 ACOs beginning a new agreement period in 2016. Given data on current participation, we anticipate the program will continue to garner comparable levels of participation from markets exhibiting baseline per-capita FFS expenditures above, at, or below the national average. In addition, we assumed the level of savings generated by an ACO to positively correlate to the achieved quality performance score and resulting sharing percentage.
For estimating the impact of the proposed changes, we assume that most ACOs (approximately 9 out of 10, on average) will choose Track 1 despite a proposed decrease in the savings sharing percentage. This is because the ACOs will seek to simultaneously: (1) Avoid the potential for financial loss if expenditures experience a significant upward fluctuation or efficiency improvements are less effective than planned; and (2) continue to build organizational experience to achieve a per-capita cost target as determined under the program's benchmark methodology.
In contrast, we assume that a minority of ACOs—disproportionately represented from a more capable subset of the total program participation—will opt for Track 3 in the second agreement period. These ACOs will be enabled by experience accepting risk and/or achieving success in their first agreement period in this program, and motivated by the provision for prospective assignment of beneficiaries and the greater sharing percentage as proposed for this new option. A particularly important cause for uncertainty in our estimate is the high degree of variability observed for local per-capita cost growth rates relative to the national average “flat dollar” growth (used to update ACO benchmarks). The benchmark or expenditure target effectively serves as the chief measure of efficiency for participating ACOs. Factors such as lower-than-average baseline per-capita expenditure and variation in local growth rates relative to the national average can trigger shared savings payments even in the absence of any efficiency gains. Similarly, some ACOs could find that factors, such as prevailing per-capita expenditure growth in their service area that is higher than the national average, limit efficiency gains and reduce or prevent shared savings.
b. Detailed Stochastic Modeling Results
Table 10 shows the distribution of the estimated net financial impact for the 2,500 stochastically generated trials under the scenario where all proposed changes are implemented. (The amounts shown are in millions, with negative net impacts representing Medicare savings). The net impact is defined as the total cost of shared savings less—(1) any amount of savings generated by reductions in actual expenditures; and (2) any shared losses collected from ACOs that accepted risk and have actual expenditures exceeding their benchmark.
The median estimate of the Shared Savings Program financial impact for ACOs potentially entering a second agreement period as proposed in this rule and covering calendar years 2016 through 2018 is a net federal savings of $1,010 million, which is $280 million higher than our estimate for the same period assuming a baseline scenario, which excludes the changes proposed in this rule. This amount represents the “best estimate” of the financial impact of the Shared Savings Program during the applicable period. However, it is important to note the relatively wide range of possible outcomes. While over 99 percent of the stochastic trials resulted in net program savings, the 10th and 90th percentiles of the estimated distribution show net savings of $430 million to net savings of $1,650 million, respectively. In the extreme scenarios, the results were as large as $2.9 billion in savings or $200 million in costs.
The stochastic model and resulting financial estimates were prepared by the CMS Office of the Actuary (OACT). The median result of $1,010 million in savings is a reasonable “point estimate” of the impact of the Shared Savings Program during the period between 2016 and 2018 if the changes proposed Start Printed Page 72854in this proposed rule are finalized and implemented. However, we emphasize the possibility of outcomes differing substantially from the median estimate, as illustrated by the estimate distribution. As we analyze additional data on ACO performance in the first agreement period, we may likely improve the precision of future financial impact estimates.
To the extent that the Shared Savings Program will result in net savings or costs to Part B of Medicare, revenues from Part B beneficiary premiums would also be correspondingly lower or higher. In addition, because MA payment rates depend on the level of spending within traditional FFS Medicare, savings or costs arising from the Shared Savings Program would result in corresponding adjustments to MA payment rates. Neither of these secondary impacts has been included in the analysis shown.
Table 11 shows the median estimated financial effects for the Shared Savings Program of ACOs entering in a new agreement period starting in 2016 and the associated 10th and 90th percentile ranges, assuming all changes in this proposed rule are implemented. Net savings (characterized by a negative net impact on federal outlays) are expected to moderately contract over the 3-year period, from a median of $380 million in 2016 to $270 million in 2018. This progression is related to the maturation of efficiencies achieved by renewing ACOs contrasted by progressive increases in shared savings payments due to increasing variability in expenditures in later performance years relative to a static benchmark expenditure baseline. To similar effect, the potential that Track 3 ACOs experiencing losses may elect to voluntarily terminate their participation in the program could work to decrease net savings in the last year of the period relative to prior years. We note that the percentiles are tabulated for each year separately. Therefore, the overall net impact distribution (Table 9) will not necessarily exactly match the sum of distributions for each distinct year.
Start Printed Page 72855c. Further Consideration
The impact analysis shown is only for the 3 years 2016 through 2018 corresponding to the second agreement period potentially available for the up to nearly 220 ACOs that will complete their first agreement period in 2015. As of January 1, 2014, 123 additional ACOs have joined the program and would potentially be eligible for a second agreement period beginning in 2017. For both groups of ACOs, uncertainties exist regarding providers' continued engagement with program goals and incentives, especially for providers who fail to generate shared savings revenue comparable to the cost of effective participation in the program. It is possible that, notwithstanding the enhancements proposed in this rule, a significant drop-off in participation could materialize from ACOs failing to achieve significant revenue from shared savings in the short run. On the other hand, value-based payment models are showing significant growth in arrangements from state Medicaid programs, private insurers, and employer-sponsored plans. Moreover, we would also note that the number of providers and suppliers participating in these models and in the existing ACOs continues to grow. Therefore, providers may view continued participation in this program as part of a wider strategy for care redesign rather than be driven only by the potential for receiving incentives in the form of shared savings payments from the Medicare Shared Savings Program. Therefore, there remains a potential for broad gains in efficiency and quality of care delivery across all populations served by ACOs participating in the Shared Savings Program with possible additional “spillover” effects on federal savings potentially traceable to momentum originally created by this program. The stochastic model for estimating future program impacts starting in 2016 does not incorporate either of these divergent longer-run scenarios, but both remain possibilities. An impact estimate expanded to include performance beyond the 2016 through 2018 agreement period would likely entail a significantly wider range of possible outcomes. However, emerging results of the first performance cycle will help inform estimates of the ongoing financial effects of the Shared Savings Program.
2. Effects on Beneficiaries
This program is still in the early stages of implementation. However, we continue to believe that the Shared Savings Program will benefit beneficiaries because the intent of the program is to—
- Encourage providers and suppliers to join together to form ACOs that will be accountable for the care provided to an assigned population of Medicare beneficiaries;
- Improve the coordination of FFS items and services; andStart Printed Page 72856
- Encourage investment in infrastructure and redesigned care processes for high quality and efficient service delivery that demonstrates a dedication to, and focus on, patient-centered care that results in higher quality care.
The benefits of a payment model that encourages providers and suppliers to become accountable for the overall care furnished to Medicare beneficiaries were evidenced by the PGP demonstration, upon which many features of the Shared Savings Program are based. Under the PGP demonstration, all of the PGP participants achieved improvements in their scores for most of the quality measures over time. While only 2 PGP participants met all 10 quality measure targets active in their first performance year, by the fifth performance year, seven sites met all 32, or 100 percent of their targets, and the remaining 3 PGP participants met over 90 percent of the targets. More specifically, as we previously discussed in our November 2011 final rule (76 FR 67968), over the first 4 years of the PGP Demonstration, physician groups increased their quality scores an average of 10 percentage points on the ten diabetes measures, 13 percentage points on the ten congestive heart failure measures, 6 percentage points on the seven coronary artery disease measures, 9 percentage points on the 2 cancer screening measures, and 3 percentage points on the 3 hypertension measures. Further analysis is provided in the Physician Group Practice Demonstration Evaluation Report (Report to Congress, 2009; http://www.cms.gov/DemoProjectsEvalRpts/downloads/PGP_RTC_Sept.pdf).
As we have also previously discussed (76 FR 67968), in addition to the overall increases in quality scores, we can examine the impact of the PGP Demonstration on quality by comparing the values of the seven claims-based quality measures for each PGP site and its comparison group. Our analysis found that, on the claims-based measures, PGP performance exceeded that of the comparison groups (CGs) on all measures between the base year (BY) and performance year 2 (PY2). It also found that the PGP sites exhibited more improvement than their CGs on all but one measure between the BY and PY2. Even after adjusting for pre-demonstration trends in the claims-based quality indicators, the PGP sites improved their claims-based quality process indicators more than their comparison groups.
Further, for the first year of the Pioneer ACO Model, all 32 Pioneer ACOs successfully reported quality measures and achieved the maximum quality score for complete and accurate reporting, earning incentive payments for their reporting accomplishments. Overall, Pioneer ACOs performed better than published rates in FFS Medicare for all 15 clinical quality measures for which comparable data are available. For example,
- Twenty-five of 32 Pioneer ACOs generated lower risk-adjusted readmission rates for their aligned beneficiaries than the benchmark rate for all Medicare FFS beneficiaries.
- Pioneer ACOs performed better on clinical quality measures that assess hypertension control for patients. The median rate among Pioneer ACOs on blood pressure control among beneficiaries with diabetes was 68 percent compared to 55 percent as measured in adult diabetic population in 10 managed care plans across 7 states from 2000 to 2001.
- Pioneer ACOs performed better on clinical quality measures that assess low density lipoprotein (LDL) control for patients with diabetes. The median rate among Pioneer ACOs for LDL control among beneficiaries with diabetes was 57 percent compared to 48 percent in an adult diabetic population in 10 managed care plans across 7 states from 2000 to 2001.
Additionally, under the Shared Savings Program, all but 6 organizations fully and completely reported quality measures for the 2013 reporting period, providing important information on current performance that can be used to improve patient engagement and make meaningful positive impacts on patient care.
Above and beyond the early quality data generated by participating organizations, we have anecdotal evidence that illustrates the importance of encouraging participation in the Shared Savings Program. For example, ACO providers/suppliers report very meaningful changes in patient engagement through beneficiary participation on the governing body of the ACO and on patient advisory committees. In response to beneficiary input, clinical practices are offering extended office hours, including weekend hours, and ensuring timely appointments and access to clinical staff. Using the data shared by CMS, ACOs are able to identify high risk beneficiaries that require additional clinical attention, assign case managers, and actively work to improve care for these beneficiaries. One ACO reported that it has implemented a process for performing in-home medication reconciliation and review of care plans as a follow up to hospital discharge and for one third of those patients, discovered an intervention that avoided an unnecessary hospital readmission. Active identification and management of these patients has uncovered previously unaddressed issues that factored into patient inability to adhere to treatment plans. For example, one ACO reported that it has uncovered several psycho-social issues that were resulting in avoidable readmissions such as—
- The inability to self-medicate (the ACO arranged for home health services);
- Lack of transportation to clinical practices (the ACO's affiliated hospitals had a taxi service voucher program that the ACO was able to expand to the beneficiary population assigned to the ACO):
- Inadequate access to healthy food resources (the ACO worked with community stakeholders to have meals delivered to the patient's home).
Additionally, ACOs are using claims data to identify diagnoses prevalent in the assigned population and develop best practice guidelines for those conditions, and educating and alerting ACO participants and ACO providers/suppliers to standardize care.
We expect that the changes proposed in this proposed rule, specifically those easing administrative requirements, smoothing the transition to a risk-based model, and expanding opportunities to share in a higher level of savings will encourage greater program participation by ACOs, which will in turn increase the number of beneficiaries that can potentially benefit from high quality and more coordinated care. Nonetheless, this program does not affect beneficiaries' freedom of choice regarding which providers and suppliers they see for care since beneficiaries assigned to an ACO continue to be in the traditional Medicare program. Thus, beneficiaries may continue to choose providers and suppliers that do not participate in ACOs under the Shared Savings Program.
3. Effect on Providers and Suppliers
Based on discussions with ACOs that generated interim shared savings and demonstrated high quality care during their first performance year in the Shared Savings Program, we know that ACOs are busy implementing a variety of strategies designed to improve care coordination for beneficiaries and lower the rate of growth in expenditures. Most of these ACOs consider themselves to be “physician-based” organizations, rather than “hospital-based”, although many state that a strong collaboration between Start Printed Page 72857inpatient and outpatient facilities is critical to better care coordination across sites of care. ACOs mentioned several strategies they believed were important such as careful pre-participation planning, transparency between the ACO leadership and its ACO participants and ACO providers/suppliers, education of ACO providers/suppliers regarding the ACO's care processes, strong physician leadership, and working to streamline and transform practices for highly efficient coordinated care across sites of care. Several clinicians in ACOs have reported to us that the ACO is providing them with the support and structure needed to practice “how [they] always hoped [they] could”. All of the ACOs recognize that they are early in the process of implementing their strategies to improve care coordination and reduce the rate of growth in expenditures and have plans to refine and improve based upon their early lessons learned.
We realize that ACOs bear costs in building the organizational, financial and legal infrastructure that is necessary to participate in the Shared Savings Program and implementing the strategies previously articulated, as well as performing the tasks required of an ACO, such as: Quality reporting, conducting patient surveys, and investing in infrastructure for effective care coordination. While provider and supplier participation in the Shared Savings Program is voluntary, we have examined the potential costs of continued program participation.
In this proposed rule, we are proposing to revise several program policies in order to reduce the burden associated with the infrastructure, start-up and ongoing annual operating costs for participating ACOs in the Shared Savings Program. These proposals include simplifying the application process for certain ACOs with experience under either Pioneer ACO Model or the Shared Savings Program streamlining sharing of beneficiary data. These significant proposed policy modifications are discussed in detail in sections II.B., C., and D. of this proposed rule.
The Shared Savings Program is still relatively new, and the initial group of organizations that applied to participate has only recently completed the first performance year. Because of this limited experience with the program and flexibility regarding the composition of providers and suppliers within an ACO and the strategies that the provider community will pursue in order to improve quality and reduce cost of care, precise estimates of expected provider costs or changes to their costs due to this proposed rule are difficult to create.
In our November 2011 final rule (76 FR 67968), we discussed a Government Accountability Office analysis of the PGP demonstration. The GAO study showed that both start-up and annual operating costs varied greatly across the participating practices. Thus, as we indicated in the November 2011 final rule (76 FR 67968), we use GAO's analysis not to predict cost investment and operating expenditures, but to demonstrate that we expect the range of investment to vary greatly across ACOs and to provide the potential scope for aspiring participants.
For purposes of our current impact analysis, we are retaining the assumption included in our November 2011 final rule (76 FR 67969) of $0.58 million in average start-up investment cost but are revising our assumption for average ongoing annual operating costs for an ACO from $1.27 million to $0.86 million to reflect the lower average number of beneficiaries assigned to existing Shared Savings Program ACOs (approximately 14,700 beneficiaries) compared to the ten PGP sites examined by GAO (average size approximately 22,400 beneficiaries). Therefore, our cost estimates for purposes of this proposed rule reflect an average estimate of $0.58 million for the start-up investment costs and $0.86 million in ongoing annual operating costs for an ACO participating in the Shared Savings Program. Assuming an expected range of ACOs participating in the Shared Savings Program of 50 to 210 ACOs (baseline scenario and all changes scenario, respectively) yields an estimated aggregate start-up investment cost ranging from $7 million to $30 million (assuming 1 in 4 ACOs will incur start-up costs), with aggregate ongoing operating costs ranging from $43 million to $181 million for the agreement period coinciding with CYs 2016 through 2018. We are also assuming that ACOs participating in a track that includes two-sided performance-based risk will in certain cases drop out of the program after receiving poor results for the first performance period beginning in 2016. Such drop out activity is assumed to affect a greater proportion of ACOs at baseline than under the all changes scenario because of the requirement that all renewing ACOs participate in Track 2 under the baseline scenario. When utilizing the anticipated mean participation rate of ACOs in the Shared Savings Program for such agreement period coupled with the average start-up investment and ongoing annual operating costs for the up to 3 years that ACOs may participate for such agreement period, this yields estimated aggregate average start-up investment and ongoing operating costs of $121 million for 50 ACOs (assuming no regulatory changes) to $562 million for 210 ACOs (assuming the proposed regulatory changes) for the agreement period covering CYs 2016 through 2018.
While there will be a financial cost placed on ACOs that participate, there will be benefits to the respective organizations in the form of increased operational and healthcare delivery efficiency. Furthermore, as discussed previously, and explained in more detail in the preamble of this proposed rule, there will be an opportunity for financial reward for success in the program in the form of shared savings. As shown in Table 12, the estimate of the shared savings that will be paid to participating ACOs is a median of $630 million during CYs 2016 through 2018, with $470 million and $820 million reflecting the 10th and 90th percentiles, respectively. (Similar to the previously presented stochastic distributions, the distribution represents uncertainty given the range of expert opinion, rather than a true statistical probability distribution.)
Compared to shared savings payments, under our proposed changes to the program, we anticipate collection from participating ACOs of a relatively moderate $30 million in shared losses during the same period, with our 10th and 90th percentiles projecting $10 million and $70 million in shared losses collected, respectively. Shared losses decrease relative to the baseline (median of $170 million over the same 3 years) because, in contrast to the baseline requirement, not all renewing ACOs would be required to enter Track 2 and take on downside risk. Modeling indicates that not all ACOs choosing downside risk in a second agreement period, whether required, as under the current regulation or as an alternative option under the proposed changes, will achieve shared savings and some may incur a financial loss, due to the requirement to repay a share of actual expenditures in excess of their benchmark as shared losses. The significantly reduced level of shared losses anticipated under the all proposed changes scenario is largely attributable to the proposed option for eligible ACOs to be able to renew under a modified Track 1, and illustrates a key reason why the program would be anticipated to see significantly stronger continued participation under the proposed changes than at baseline.Start Printed Page 72858
Assuming the proposed changes in this proposed rule, total median ACO shared savings payments ($630 million) net of median shared losses ($30 million) to ACOs with agreement periods covering CYs 2016 through 2018 are $600 million in net payments. Such median total net payment amount, coupled with the aggregate average start-up investment and ongoing operating cost of $562 million, incurred by the mean participation rate of ACOs in the Shared Savings Program during the same time period, yields a net private benefit of $38 million. At baseline, absent the proposed changes, the median net payments to ACOs over the same time period would be only $140 million ($310 million in shared savings payments less $170 million in shared losses). Such lower net sharing at baseline, combined with baseline average start-up investment and ongoing operating costs of $121 million, yields a net private benefit of $19 million. We expect that a significant portion of Track 1 ACOs that are assumed to be unwilling to renew under the program without the protection from downside risk will welcome the opportunity to continue under Track 1 for a second agreement period, albeit with a lower maximum sharing rate of 40 percent. Moreover, the proposed changes reduce the estimated per-ACO average shared loss liability by over 95 percent compared to the baseline, and increase the chance an ACO renewing in 2016 will continue to participate for all 3 years of the new agreement period.
We would note that our estimates of net private benefits under the baseline and all proposed changes scenarios are influenced by assumptions that could vary in practice and thus result in a very different actual result than what was estimated. First, we assume that savings realized by existing ACOs during their first agreement period are built into their benchmarks and our baseline for their successive agreement period. This means that these ACOs may have to achieve greater efficiencies and quality improvements during their successive agreement period compared to their prior one in order to share in savings. Moreover, the extent to which these ACOs actually exceed or fall short of our assumed baseline savings will result in higher or lower actual net private benefits relative to our estimate. Second, our estimates assume a large proportion of existing Track 1 ACOs will continue participating under Track 1 for 2016 to 2018, albeit at the lower 40 percent sharing rate. This assumption has the effect of diminishing estimated benefits under our model. Thus, all else being equal, the extent to which a smaller or larger percentage of these ACOs remain under Track 1 for their second agreement period will also respectively increase or decrease the actual net private benefits relative to what we estimated. Finally, to the extent that actual ACO quality performance exceeds or falls short of our estimates, the net private benefits could be respectively higher or lower than what we estimated.
We also note that the net private benefits actually experienced by a given ACO may increase as a result of other benefits associated with participation in the Shared Savings Program. For example, an ACO that is participating in the Shared Savings Program and simultaneously receives value-based contracts from other payers may receive additional benefits. Such potential benefits are not considered in our analysis because they are not readily quantifiable. Therefore, we limit our benefit-cost estimate to shared savings and shared loss dollars received under the Shared Savings Program relative to estimated operational costs associated with participating in the program as previously described.
Start Printed Page 728594. Effect on Small Entities
The RFA requires agencies to analyze options for regulatory relief of small entities, if a rule has a significant impact on a substantial number of small entities. For purposes of the RFA, small entities include small businesses, nonprofit organizations, and small governmental jurisdictions. Most physician practices, hospitals and other providers are small entities, either by virtue of their nonprofit status or by qualifying as small businesses under the Small Business Administration's size standards (revenues of less than $7.5 to $38.5 million in any 1 year; NAIC Sector-62 series). States and individuals are not included in the definition of a small entity. For details, see the Small Business Administration's Web site at http://www.sba.gov/content/small-business-size-standards. For purposes of the RFA, approximately 95 percent of physicians are considered to be small entities. There are over 1 million physicians, other practitioners, and medical suppliers that receive Medicare payment under the Physician Fee Schedule (PFS).
Although the Shared Savings Program is a voluntary program and payments for individual items and services will continue to be made on a FFS basis, we acknowledge that the program can affect many small entities and have drafted the proposed changes to our rules and regulations accordingly in order to minimize costs and administrative burden on such entities as well as to maximize their opportunity to participate. Small entities are both allowed and encouraged to participate in the Shared Savings Program, provided they have a minimum of 5,000 assigned beneficiaries, thereby potentially realizing the economic benefits of receiving shared savings resulting from the utilization of enhanced and efficient systems of care and care coordination. Therefore, a solo, small physician practice or other small entity may realize economic benefits as a function of participating in this program and the utilization of enhanced clinical systems integration, which otherwise may not have been possible.
We have determined that this proposed rule will have a significant impact on a substantial number of small entities and we present more detailed analysis of these impacts, including costs and benefits to small entities and alternative policy considerations throughout this RIA. However, as detailed in this RIA, total median shared Start Printed Page 72860savings payments net of shared losses will offset about 107 percent of the average costs borne by entities participating in the Shared Savings Program, with an offset significantly greater than the cost of participation for the subset of ACOs that achieve shared savings in a given year, and no downside risk of significant shared losses for ACOs choosing to remain under Track 1 for a second agreement period. As a result, this regulatory impact section, together with the remainder of the preamble, constitutes our preliminary Regulatory Flexibility Analysis.
5. Effect on Small Rural Hospitals
Section 1102(b) of the Act requires us to prepare a regulatory impact analysis if a rule may have a significant impact on the operations of a substantial number of small rural hospitals. This analysis must conform to the provisions of section 603 of the RFA. For purposes of section 1102(b) of the Act, we define a small rural hospital as a hospital that is located outside of a metropolitan statistical area and has fewer than 100 beds. Although the Shared Savings Program is a voluntary program, this proposed rule will have a significant impact on the operations of a substantial number of small rural hospitals. We have proposed changes to our regulations such that rural hospitals will have stronger incentives to participate in the program through offering a smoother transition to risk-based models, additional opportunities to potentially share in savings under proposed new Track 3, and streamlined administrative requirements. As detailed in this RIA, the estimated aggregate median impact of shared savings payments to participating ACOs is approximately 107 percent of the average costs borne by entities that voluntarily participate in the Shared Savings Program, with an offset significantly greater than the cost of participation for the subset of ACOs that achieve shared savings in a given year, and no downside risk of significant shared loss penalties for ACOs choosing to remain under Track 1 for a second agreement period.
6. Unfunded Mandates
Section 202 of the Unfunded Mandates Reform Act of 1995 (UMRA) also requires that agencies assess anticipated costs and benefits before issuing any rule whose mandates require spending in any 1 year of $100 million in 1995 dollars, updated annually for inflation. In 2014, that is approximately $141 million. This proposed rule does not include any mandate that would result in spending by state, local or tribal governments, in the aggregate, or by the private sector in the amount of $141 million in any 1 year. Further, participation in this program is voluntary and is not mandated.
D. Alternatives Considered
In the November 2011 final rule (76 FR 67971), we noted in the regulatory impact analysis that many tenets of the program are statutorily mandated and thus allow for little, if any, flexibility in the rulemaking process. Where there was flexibility, we made our policy decisions regarding alternatives based on a balance between creating the least possible negative impact on the stakeholders affected by the program and satisfactorily fitting the vision of the program within given operational constraints. This proposed rule contains a range of modifications to program policies that take this balance into consideration. The preceding preamble provides descriptions of the various statutory provisions that are addressed in this proposed rule, identifies those policies where discretion has been allowed and exercised, presents the rationales for our proposals and, where relevant, alternatives that were considered.
In addition to estimating the difference between impacts at baseline and assuming all proposed changes are adopted, the stochastic model was also adapted to isolate marginal impacts for several alternative scenarios related to individual proposals within the overall set of proposed changes to the program. In one scenario, all proposed changes were assumed except the addition of Track 3. Relative to the all-changes scenario, this modification was not anticipated to materially reduce overall participation. However, we estimated that excluding Track 3 as a proposal would reduce median gross savings by $70 million over 3 years as fewer ACOs would be willing to accept the stronger incentive of downside risk without the opportunity to earn enhanced shared savings up to the 75 percent maximum sharing percentage under Track 3. Lastly, median shared losses under this scenario would decline by $10 million. Thus, the overall impact on net federal savings of offering Track 3 in the context of all other proposed changes to the program is minimal. However for individual ACOs, the higher sharing rate available under Track 3 may boost efforts to build capacity for accepting downside risk while potentially accelerating activities related to improving the efficiency of care. Also, the opportunity under Track 3 to share in a greater percentage of the savings that are achieved could assist in addressing the concerns of ACOs that were successful in achieving savings in their first agreement period but are concerned that their new expenditure baseline for the agreement period starting in 2016 will be lower as a result of their prior success in reducing the cost of care for their assigned beneficiaries, thus making it more difficult to achieve savings.
Another alternative scenario we considered included all proposed changes except for lowering the Track 1 sharing rate from 50 percent to 40 percent for Track 1 ACOs that elect to renew for a second agreement period under this model starting in 2016. Similar to the previous scenario, this change would not be expected to materially change overall assumed participation. However, relative to the all changes model, the net effect of this alternative would be to increase median shared savings payments by $110 million over 3 years. Furthermore, because a portion of ACOs that would have otherwise chosen Track 3 under the all changes scenario would now be expected to choose Track 1 given the higher sharing rate, overall median gross savings would decline by $30 million under this alternative, resulting in an overall reduction of $140 million in median net federal savings compared to the all changes scenario.
Lastly, an alternative scenario was considered where no changes were proposed other than to allow current Track 1 ACOs a 2-year extension to their current agreement period, after which they would then be limited to participating under Track 2 as required under the current regulations. This alternative was assumed to boost ACO participation in 2016 and 2017 comparable to the participation level expected for such years in the all-changes scenario. However, we would anticipate a significant contraction in participation in 2018 similar to the rate of participation assumed at baseline for that year. The net impact of this alternative would be $220 million in reduced net federal savings compared to all changes as proposed in this rule, driven mainly by reduced program participation in the third year and by increased shared savings payments in 2016 and 2017 because ACO benchmarks would not be rebased until 2018.
E. Accounting Statement and Table
As required by OMB Circular A-4 under Executive Order 12866, in Table 13, we have prepared an accounting statement showing the change in (A) net Start Printed Page 72861federal monetary transfers, (B) shared savings payments to ACOs net of shared loss payments from ACOs and (C) the aggregate cost of ACO operations for ACO participants and ACO providers/suppliers from 2016 to 2018 that are associated with the provisions of this proposed rule as compared to baseline.
Table 13—Accounting Statement Estimated Impacts
[CYs 2016-2018]
Category Primary estimate (in millions) Minimum estimate (in millions) Maximum estimate (in millions) Source citation (RIA, preamble, etc.) BENEFITS: Annualized monetized transfers Discount rate: 7% −$76.3 −$12.0 −$129.7 Change from baseline (Table 8) to proposed changes (Table 9) Annualized monetized transfers Discount rate: 3% −$83.8 −$13.7 −$142.0 From whom to whom? Negative values reflect reduction in federal net cost resulting from care management by ACOs BENEFITS: Annualized monetized transfers Discount rate: 7% $124.1 $96.5 $152.0 Change from baseline (Table 8) to proposed changes (Table 9) Annualized monetized transfers Discount rate: 3% $134.8 $105.1 $164.7 From whom to whom? Positive values reflect increase in aggregate shared savings net of shared losses OPERATIONAL COST: Annualized monetized transfers Discount rate: 7% $121.3 Change from baseline (Table 8) to proposed changes (Table 9) Annualized monetized transfers Discount rate: 3% $130.7 From whom to whom? Positive values reflect increase in aggregate ACO operating costs largely attributable to assumed increased participation as a result of the proposals included in this proposed rule compared to baseline F. Conclusion
The analysis in this section, together with the remainder of this preamble, provides a Regulatory Impact Analysis. As a result of this proposed rule, the median estimate of the financial impact of the Shared Savings Program for CYs 2016 through 2018 would be net federal savings (after shared savings payments) of $1,010 million. Under this proposed rule, median savings would be about $280 million higher than we estimate assuming none of the proposed changes for this period. Although this is the “best estimate” of the financial impact of the Shared Savings Program during CYs 2016 through 2018, a relatively wide range of possible outcomes exists. While over 99 percent of the stochastic trials resulted in net program savings, the 10th and 90th percentiles of the estimated distribution show net savings of $430 million to net savings of $1,650 million, respectively. In the extreme scenarios, the results were as large as $2.9 billion in savings or $200 million in costs.
In addition, at the anticipated mean participation rate of ACOs in the Shared Savings Program, participating ACOs may experience an estimated aggregate average start-up investment and ongoing operating cost of $815 million for CYs 2016 through 2018. Lastly, we estimate an aggregate median impact of $630 million in shared savings payments to participating ACOs in the Shared Savings Program for CYs 2016 through 2018. The 10th and 90th percentiles of the estimate distribution, for the same time period, yield shared savings payments to ACOs of $470 million and $820 million, respectively. Therefore, the total median ACO shared savings payments of $630 million during CYs 2016 through 2018, net of a median $30 million shared losses, coupled with the aggregate average start-up investment and ongoing operating cost of $562 million yields a net private benefit of $38 million.
Overall, we assumed greater participation by ACOs under the policies contained in this proposed rule due to our proposals to ease the transition from Track 1 to Track 2, reduce risk under Track 2, and adopt an alternative risk-based model—Track 3. This resulted in total shared savings increasing significantly, while shared losses decreased due to these changes. Moreover, as participation in the Shared Savings Program continues to expand, we anticipate there will be a broader focus on care coordination and quality improvement among providers and suppliers within the Medicare program that will lead to both increased efficiency in the provision of care and improved quality of the care that is provided to beneficiaries.
In accordance with the provisions of Executive Order 12866, this rule was Start Printed Page 72862reviewed by the Office of Management and Budget.
Start List of SubjectsList of Subjects in 42 CFR Part 425
- Administrative practice and procedure
- Health facilities
- Health professions
- Medicare
- Reporting and recordkeeping requirements
For the reasons set forth in the preamble, the Centers for Medicare & Medicaid Services proposes to amend 42 CFR part 425 as follows:
Start PartPART 425—MEDICARE SHARED SAVINGS PROGRAM
End Part Start Amendment Part1. The authority citation for part 425 continues to read as follows:
End Amendment PartStart Amendment Part[Amended]2. Amend § 425.10 (b)(6) by removing the phrase “two-sided model” and adding in its place the phrase “two-sided models”.
End Amendment Part Start Amendment Part3. Amend § 425.20 as follows:
End Amendment Part Start Amendment PartA. By revising the definition of “ACO participant”.
End Amendment Part Start Amendment PartB. By adding the definition of “ACO participant agreement” in alphabetical order.
End Amendment Part Start Amendment PartC. By revising the definitions of “ACO professional”, “ACO provider/supplier”, “Agreement period”, and “Assignment”.
End Amendment Part Start Amendment PartD. By adding the definition of “Assignment window” in alphabetical order.
End Amendment Part Start Amendment PartE. By revising the definitions of “Continuously assigned beneficiary”, “Hospital”, and “Newly assigned beneficiary”.
End Amendment Part Start Amendment PartF. By adding the definition of “Participation agreement” in alphabetical order.
End Amendment Part Start Amendment PartG. In the definition of “Performance year” by removing the phrase “in the ACO's agreement” and adding in its place the phrase “in the participation agreement”.
End Amendment Part Start Amendment PartH. In paragraph (2) of the definition of “Primary care services”, by removing the “;” and adding in its place “.”.
End Amendment Part Start Amendment PartI. By adding paragraphs (4) and (5) to the definition of “Primary care services”.
End Amendment PartThe revisions and additions read as follows:
Definitions.* * * * *ACO participant means an entity identified by a Medicare-enrolled billing TIN through which one or more ACO providers/suppliers bill Medicare, that alone or together with one or more other ACO participants compose an ACO, and that is included on the list of ACO participants that is required under § 425.118.
ACO participant agreement means the written agreement (as required at § 425.116) between the ACO and ACO participant in which the ACO participant agrees to participate in, and comply with, the requirements of the Shared Savings Program.
ACO professional means an individual who is Medicare-enrolled and bills for items and services furnished to Medicare fee-for-service beneficiaries under a Medicare billing number assigned to the TIN of an ACO participant in accordance with applicable Medicare regulations and who is either of the following:
(1) A physician legally authorized to practice medicine and surgery by the State in which he or she performs such function or action.
(2) A practitioner who is one of the following:
(i) A physician assistant (as defined at § 410.74(a)(2) of this chapter).
(ii) A nurse practitioner (as defined at § 410.75(b) of this chapter).
(iii) A clinical nurse specialist (as defined at § 410.76(b) of this chapter)
ACO provider/supplier means an individual or entity that meets all of the following:
(1) Is a—
(i) Provider (as defined at § 400.202 of this chapter); or
(ii) Supplier (as defined at § 400.202 of this chapter).
(2) Is enrolled in Medicare.
(3) Bills for items and services furnished to Medicare fee-for-service beneficiaries during the agreement period under a Medicare billing number assigned to the TIN of an ACO participant in accordance with applicable Medicare regulations.
(4) Is included on the list of ACO providers/suppliers that is required under § 425.118.
Agreement period means the term of the participation agreement, which is 3 performance years unless otherwise specified in the participation agreement.
* * * * *Assignment means the operational process by which CMS determines whether a beneficiary has chosen to receive a sufficient level of the requisite primary care services from ACO professionals so that the ACO may be appropriately designated as exercising basic responsibility for that beneficiary's care during a given benchmark or performance year.
Assignment window means the 12-month period used to assign beneficiaries to an ACO.
* * * * *Continuously assigned beneficiary means a beneficiary assigned to the ACO in the current performance year who was either assigned to or received a primary care service from any of the ACO participants during the assignment window for the most recent prior benchmark or performance year.
* * * * *Hospital means a hospital as defined in section 1886(d)(1)(B) of the Act.
* * * * *Newly assigned beneficiary means a beneficiary that is assigned to the ACO in the current performance year who was neither assigned to nor received a primary care service from any of the ACO participants during the assignment window for the most recent prior benchmark or performance year.
* * * * *Participation agreement means the written agreement required under § 425.208(a) between the ACO and CMS that, along with the regulations in this part, govern the ACO's participation in the Shared Savings Program.
* * * * *Primary care services * * *
(4) CPT codes 99495 and 99496 and HCPCS code GXXX1.
(5) Additional codes designated by CMS as primary care services for purposes of the Shared Savings Program, including new HCPCS/CPT and revenue center codes and any subsequently modified or replacement codes for the HCPCS/CPT and revenue center codes identified in paragraphs (1) through (4) of this definition.
* * * * *Start Amendment Part[Amended]4. Amend § 425.100 as follows:
End Amendment Part Start Amendment PartA. In paragraph (b) by removing the reference “under § 425.604 or § 425.606” and adding in its place the reference “under § 425.604, § 425.606 or § 425.610”.
End Amendment Part Start Amendment PartB. In paragraph (c) by removing the phrase “under the two-sided model” and adding in its place the phrase “under a two-sided model”.
End Amendment Part Start Amendment PartC. In paragraph (c) by removing the reference “under § 425.606” and adding in its place the reference “under § 425.604, § 425.606 or § 425.610”.
End Amendment Part Start Amendment Part5. Amend § 425.102 as follows:
End Amendment Part Start Amendment PartA. By adding paragraph (a)(8).
End Amendment Part Start Amendment PartB. In paragraph (b) by removing the phrase “eligible participate” and adding in its place the phrase “eligible to participate”.
End Amendment PartThe addition reads as follows:
Eligible providers and suppliers.(a) * * *
(8) Teaching hospitals that have elected under § 415.160 of this chapter Start Printed Page 72863to receive payment on a reasonable cost basis for the direct medical and surgical services of their physicians.
* * * * *Start Amendment Part[Amended]6. Amend § 425.104(b), by removing the phrase “otherwise independent ACO participants must” and adding in its place the phrase “ACO participants, each of which is identified by a unique TIN, must”.
End Amendment Part Start Amendment Part7. Amend § 425.106 by revising paragraphs (a), (b)(3), (c)(1), (c)(2), and (c)(5) to read as follows:
End Amendment PartStart Amendment PartShared governance.(a) General rule. (1) An ACO must maintain of an identifiable governing body with ultimate authority to execute the functions of an ACO as defined under this part, including but not limited to the processes defined under § 425.112 to promote evidence-based medicine and patient engagement, to report on quality and cost measures, and to coordinate care.
(2) The governing body of the ACO must satisfy all of the following criteria:
(i) Be the same as the governing body of the legal entity that is the ACO.
(ii) Be separate and unique to the ACO and must not be the same as the governing body of any ACO participant, in the case of an ACO that comprises two or more ACO participants.
(iii) Satisfy all other requirements of this section.
(b) * * *
(3) The governing body members must have a fiduciary duty to the ACO, including the duty of loyalty, and must act consistent with that fiduciary duty.
* * * * *(c) * * *
(1) The ACO must—(i) Establish a mechanism for shared governance among the ACO participants or combinations of ACO participants (as identified in § 425.102(a)) that formed the ACO; and
(ii) Provide for meaningful participation in the composition and control of the ACO's governing body for ACO participants or their designated representatives.
(2) The ACO governing body must include a Medicare beneficiary who—
(i) Is served by the ACO;
(ii) Is not an ACO provider/supplier;
(iii) Does not have a conflict of interest with the ACO; and
(iv) Does not have an immediate family member who has a conflict of interest with the ACO.
* * * * *(5) In cases in which the composition of the ACO's governing body does not meet the requirements of paragraphs (c)(2) of this section, the ACO must describe—
(i) Why it seeks to differ from this requirement; and
(ii) How it will provide meaningful representation of Medicare beneficiaries in ACO governance.
* * * * *8. Amend § 425.108 by removing paragraph (e) and revising paragraph (c) to read as follows:
End Amendment PartStart Amendment PartLeadership and management.* * * * *(c) Clinical management and oversight must be managed by a senior-level medical director. The medical director must be—
(1) A board-certified physician;
(2) Licensed in a State in which the ACO operates; and
(3) Physically present on a regular basis at any clinic, office or other location of the ACO, ACO participant or ACO provider/supplier.
* * * * *9. Amend § 425.110 by revising paragraphs (a)(2) and (b) to read as follows:
End Amendment PartStart Amendment PartNumber of ACO professionals and beneficiaries.(a) * * *
(2) CMS deems an ACO to have initially satisfied the requirement to have at least 5,000 assigned beneficiaries as specified in paragraph (a)(1) of this section if 5,000 or more beneficiaries are historically assigned to the ACO participants in each of the 3 benchmark years, as calculated using the assignment methodology set forth in subpart E of this part. In the case of the third benchmark year, CMS uses the most recent data available to estimate the number of assigned beneficiaries.
(b) If at any time during the performance year, an ACO's assigned population falls below 5,000, the ACO may be subject to the actions described in §§ 425.216 and 425.218.
(1) While under a CAP, the ACO remains eligible for shared savings and losses and the MSR is set at a level consistent with the number of assigned beneficiaries.
(2) If the ACO's assigned population is not at least 5,000 by the end of the performance year specified by CMS in its request for a CAP, CMS terminates the participation agreement and the ACO is not eligible to share in savings for that performance year.
10. Amend § 425.112 by adding paragraphs (b)(4)(ii)(C), (D), and (E) to read as follows:
End Amendment PartStart Amendment PartRequired processes and patient-centeredness criteria.* * * * *(b) * * *
(4) * * *
(ii) * * *
(C) Describe how the ACO will encourage and promote use of enabling technologies for improving care coordination for beneficiaries. Enabling technologies may include one or more of the following:
(1) Electronic health records and other health IT tools.
(2) Telehealth services, including remote patient monitoring.
(3) Electronic exchange of health information.
(4) Other electronic tools to engage beneficiaries in their care.
(D) Describe how the ACO intends to partner with long-term and post-acute care providers, both inside and outside the ACO, to improve care coordination for their assigned beneficiaries.
(E) Define and submit a set of major milestones or performance metrics the ACO will use in each performance year to assess the progress of its ACO participants in implementing the processes described in paragraph (b)(4) of this section.
11. Add § 425.116 to subpart B to read as follows:
End Amendment PartStart Amendment PartAgreements with ACO participants and ACO providers/suppliers.(a) ACO participant agreements. The ACO must have an ACO participant agreement with each ACO participant that complies with the following criteria:
(1) The only parties to the agreement are the ACO and the ACO participant.
(2) The agreement must be signed on behalf of the ACO and the ACO participant by individuals who are authorized to bind the ACO and the ACO participant, respectively.
(3) The agreement must expressly require the ACO participant to agree, and to ensure that each ACO provider/supplier billing through the TIN of the ACO participant agrees, to participate in the Shared Savings Program and to comply with the requirements of the Shared Savings Program and all other applicable laws and regulations (including, but not limited to, those specified at § 425.208(b)).
(4) The agreement must set forth the ACO participant's rights and obligations in, and representation by, the ACO, including without limitation, the quality reporting requirements set forth in subpart F of this part, the beneficiary notification requirements set forth at § 425.312, and how participation in the Shared Savings Program affects the Start Printed Page 72864ability of the ACO participant and its ACO providers/suppliers to participate in other Medicare demonstration projects or programs that involve shared savings.
(5) The agreement must describe how the opportunity to receive shared savings or other financial arrangements will encourage the ACO participant to adhere to the quality assurance and improvement program and evidence-based medicine guidelines established by the ACO.
(6) The agreement must require the ACO participant to update its enrollment information, including the addition and deletion of ACO professionals and ACO providers/suppliers billing through the TIN of the ACO participant, on a timely basis in accordance with Medicare program requirements and to notify the ACO of any such changes within 30 days after the change.
(7) The agreement must permit the ACO to take remedial action against the ACO participant, and must require the ACO participant to take remedial action against its ACO providers/suppliers, including imposition of a corrective action plan, denial of incentive payments, and termination of the ACO participant agreement, to address noncompliance with the requirements of the Shared Savings Program and other program integrity issues, including those identified by CMS.
(8) The agreement must be for a term of at least one performance year and must articulate potential consequences for early termination from the ACO.
(9) The agreement must require completion of a close-out process upon termination or expiration of the agreement that requires the ACO participant to furnish all data necessary to complete the annual assessment of the ACO's quality of care and addresses other relevant matters.
(b) Agreements with ACO providers/suppliers. ACOs have the option of contracting directly with its ACO providers/suppliers regarding items and services furnished to beneficiaries aligned to the ACO. An ACO's agreement with an ACO provider/supplier regarding such items and services must satisfy the following criteria:
(1) The only parties to the agreement are the ACO and the ACO provider/supplier.
(2) The agreement must be signed by the ACO provider/supplier and by an individual who is authorized to bind the ACO.
(3) The agreement must expressly require the ACO provider/supplier to agree to participate in the Shared Savings Program and to comply with the requirements of the Shared Savings Program and all other applicable laws and regulations (including, but not limited to, those specified at § 425.208(b)).
(4) The agreement must set forth the ACO provider's/supplier's rights and obligations in, and representation by, the ACO, including without limitation, the quality reporting requirements set forth in subpart F of this part, the beneficiary notification requirements set forth at § 425.312, and how participation in the Shared Savings Program affects the ability of the ACO provider/supplier to participate in other Medicare demonstration projects or programs that involve shared savings.
(5) The agreement must describe how the opportunity to receive shared savings or other financial arrangements will encourage the ACO provider/supplier to adhere to the quality assurance and improvement program and evidence-based medicine guidelines established by the ACO.
(6) The agreement must require the ACO provider/supplier to—
(i) Update its enrollment information on a timely basis in accordance with Medicare program requirements; and
(ii) Notify the ACO of any such changes within 30 days after the change.
(7) The agreement must permit the ACO to take remedial action including the following against the ACO provider/supplier to address noncompliance with the requirements of the Shared Savings Program and other program integrity issues, including those identified by CMS:
(i) Imposition of a corrective action plan.
(ii) Denial of incentive payments.
(iii) Termination of the ACO participant agreement.
(c) Submission of agreements. The ACO must submit an executed ACO participant agreement in accordance with CMS guidance for each ACO participant at the time of its initial application, participation agreement renewal process, and when adding to its list of ACO participants in accordance with § 425.118. The agreements may be submitted in the form and manner set forth in § 425.204(c)(6).
12. Add new § 425.118 to subpart B to read as follows:
End Amendment PartStart Amendment PartRequired reporting of ACO participants and ACO providers/suppliers.(a) List requirements. (1) The ACO must maintain, update, and submit to CMS an accurate and complete list identifying each ACO participant (including its Medicare-enrolled TIN) and each ACO provider/supplier (including its NPI or other identifier) in accordance with this section.
(2) Before the start of an agreement period, before each performance year thereafter, and at such other times as specified by CMS, the ACO must submit to CMS an ACO participant list and an ACO provider/supplier list.
(3) The ACO must certify the submitted lists in accordance with § 425.302(a)(2).
(4) All Medicare enrolled individuals and entities that have reassigned their right to receive Medicare payment to the TIN of the ACO participant must be included on the ACO provider/supplier list and must agree to participate in the ACO and comply with the requirements of the Shared Savings Program before the ACO submits the ACO participant list and the ACO provider/supplier list.
(b) Changes to the ACO participant list. (1) Additions. (i) An ACO must submit to CMS a request to add an entity and its Medicare enrolled TIN to its ACO participant list. This request must be submitted at such time and in the form and manner specified by CMS.
(ii) If CMS approves the request, the entity and its Medicare enrolled TIN is added to the ACO participant list effective January 1 of the following performance year.
(iii) CMS may deny the request on the basis that the entity is not eligible to be an ACO participant or on the basis of the results of the screening performed under § 425.304(b).
(2) Deletions. (i) An ACO must notify CMS no later than 30 days after the termination of an ACO participant agreement. Such notice must be submitted in the form and manner specified by CMS and must include the termination date of the ACO participant agreement.
(ii) The entity is deleted from the ACO participant list as of the termination date of the ACO participant agreement.
(3) Adjustments. (i) CMS annually adjusts an ACO's assignment, historical benchmark, the quality reporting sample, and the obligation of the ACO to report on behalf of ACO providers/suppliers for certain CMS quality initiatives to reflect the addition or deletion of entities from the list of ACO participants that is submitted to CMS before the start of a performance year in accordance with paragraph (a) of this section.
(ii) Absent unusual circumstances, CMS does not make adjustments during the performance year to the ACO's assignment, historical benchmark, performance year financial calculations, the quality reporting sample, or the obligation of the ACO to report on Start Printed Page 72865behalf of ACO providers/suppliers for certain CMS quality initiatives to reflect the addition or deletion of entities from the ACO participant list that become effective during the performance year. CMS has sole discretion to determine whether unusual circumstances exist that would warrant such adjustments.
(c) Changes to the ACO provider/supplier list. (1) Additions. (i) An ACO must notify CMS within 30 days after an individual or entity becomes a Medicare-enrolled provider or supplier that bills for items and services it furnishes to Medicare fee-for-service beneficiaries under a billing number assigned to the TIN of an ACO participant. The notice must be submitted in the form and manner specified by CMS.
(ii) If the ACO timely submits notice to CMS, the addition of an individual or entity to the ACO provider/supplier list is effective on the date specified in the notice furnished to CMS, but no earlier than 30 days before the date of the notice. If the ACO fails to submit timely notice to CMS, the addition of an individual or entity to the ACO provider/supplier list is effective on the date of the notice.
(2) Deletions. (i) An ACO must notify CMS no later than 30 days after an individual or entity ceases to be a Medicare-enrolled provider or supplier that bills for items and services it furnishes to Medicare fee-for-service beneficiaries under a billing number assigned to the TIN of an ACO participant. The notice must be submitted in the form and manner specified by CMS.
(ii) The deletion of an ACO provider/supplier from the ACO provider/supplier list is effective on the date the individual or entity ceased to be a Medicare-enrolled provider or supplier that bills for items and services it furnishes to Medicare fee-for-service beneficiaries under a billing number assigned to the TIN of an ACO participant.
(d) Update of Medicare enrollment information. The ACO must ensure that all changes to enrollment information for ACO participants and ACO providers/suppliers, including changes to reassignment of the right to receive Medicare payment, are reported to CMS consistent with § 424.516.
13. Amend § 425.200 as follows:
End Amendment Part Start Amendment PartA. By revising the section heading.
End Amendment Part Start Amendment PartB. In paragraph (a), by removing the term “three” and adding in its place the figure “3”.
End Amendment Part Start Amendment PartC. In the heading of paragraph (b), and paragraphs (b)(1) introductory text, (b)(1)(i), (b)(1)(ii), (b)(2)(ii), and (c)(1) by removing the term “agreement” each time it appears and adding in its place the terms “participation agreement”.
End Amendment PartThe revision reads as follows:
Start Amendment Part14. Amend § 425.202 by revising paragraphs (b) and (c) to read as follows:
End Amendment PartStart Amendment PartApplication procedures.* * * * *(b) Condensed application form. (1) PGP demonstration sites applying to participate in the Shared Savings Program will have an opportunity to complete a condensed application form.
(2) A Pioneer ACO may use a condensed application form to apply for participation in the Shared Savings Program if it satisfies all of the following criteria:
(i) The applicant is the same legal entity as the Pioneer ACO.
(ii) ACO participant list does not contain any ACO participant TINs that did not appear on the “Confirmed Annual TIN/NPI List” (as defined in the Pioneer ACO Model Innovation Agreement with CMS) for the applicant ACO's last full performance year in the Pioneer ACO Model.
(iii) The applicant is not applying to participate in the one-sided model.
(c) Application review. CMS reviews applications in accordance with § 425.206.
15. Amend § 425.204 as follows:
End Amendment Part Start Amendment PartA. In paragraph (b)(2) by removing the terms “ACO agreement” and adding in its place the terms “participation agreement”.
End Amendment Part Start Amendment PartB. In paragraph (b)(3) by removing the term “agreement” and adding in its place the terms “participation agreement”.
End Amendment Part Start Amendment PartC. By revising paragraphs (c)(1) introductory text and (c)(1)(i), (iii), and (iv).
End Amendment Part Start Amendment PartD. In paragraph (c)(1)(vi) by removing the terms “ACO's agreement” and adding in its place the terms “participation agreement”.
End Amendment Part Start Amendment PartE. By revising paragraph (c)(3).
End Amendment Part Start Amendment PartF. In paragraph (c)(4)(ii), by removing the phrase ” among multiple, independent ACO participants” and adding in its place the phrase “among two or more ACO participants”.
End Amendment Part Start Amendment PartG. By revising paragraph (c)(5)(i).
End Amendment Part Start Amendment PartH. By adding paragraph (c)(6).
End Amendment Part Start Amendment PartI. In paragraph (e)(1), removing the phrase “an ACO must specify whether it is applying to participate in Track 1 or Track 2” and adding in its place the phrase “an ACO must specify the Track for which it is applying”
End Amendment Part Start Amendment PartJ. By revising paragraph (f).
End Amendment Part Start Amendment PartK. By adding paragraph (g).
End Amendment PartThe revisions and additions read as follows:
Start Amendment PartContent of the application.* * * * *(c) * * *
(1) As part of its application, and upon request thereafter, an ACO must submit to CMS the following supporting materials to demonstrate that the ACO satisfies the requirements set forth in this part:
(i) Documents (for example, ACO participant agreements, agreements with ACO providers/suppliers, employment contracts, and operating policies) sufficient to describe the ACO participants' and ACO providers'/suppliers' rights and obligations in and representation by the ACO, and how the opportunity to receive shared savings or other financial arrangements will encourage ACO participants and ACO providers/suppliers to adhere to the quality assurance and improvement program and evidence-based clinical guidelines.
* * * * *(iii) Materials documenting the ACO's organization and management structure, including an organizational chart, a list of committees (including names of committee members) and their structures, and job descriptions for senior administrative and clinical leaders specifically noted in § 425.108 and § 425.112(a)(2).
(iv) Evidence that the governing body—
(A) Is an identifiable body;
(B) Represents a mechanism for shared governance for ACO participants;
(C) Is composed of representatives of its ACO participants; and
(D) Is at least 75 percent controlled by its ACO participants.
* * * * *(3) If an ACO requests an exception to the governing body requirement in § 425.106(c)(2), the ACO must describe—
(i) Why it seeks to differ from this requirement; and
(ii) How the ACO will provide meaningful representation in ACO governance by Medicare beneficiaries.
* * * * *(5) * * *
(i) The ACO must submit a list of all ACO participants and ACO providers/suppliers in accordance with § 425.118.
* * * * *(6) As part of the application process and upon request by CMS, the ACO must submit documents demonstrating that its ACO participants, ACO providers/suppliers, and other individuals or entities performing Start Printed Page 72866functions or services related to ACO activities are required to comply with the requirements of the Shared Savings Program. The evidence to be submitted must include, without limitation, sample or form agreements and, in the case of ACO participant agreements, the first and signature page(s) of each executed ACO participant agreement. CMS may request all pages of an executed ACO participant agreement to confirm that it conforms to the sample form agreement submitted by the ACO. The ACO must certify that all of its ACO participant agreements comply with the requirements of this part.
* * * * *(f) Assurance of ability to repay. (1) An ACO must have the ability to repay all shared losses for which it may be liable under a two-sided model.
(i) As part of the application or participation agreement renewal process, an ACO that is seeking to participate under a two-sided model of the Shared Savings Program must submit for CMS approval documentation that it is capable of repaying shared losses that it may incur during the agreement period.
(ii) The documentation specified in paragraph (f)(1)(i) of this section must include details supporting the adequacy of the mechanism for repaying shared losses equal to at least 1 percent of the ACO's total per capita Medicare parts A and B fee-for-service expenditures for its assigned beneficiaries based on expenditures used to calculate the benchmark for the applicable agreement period, as estimated by CMS at the time of application or participation agreement renewal.
(2) An ACO may demonstrate its ability to repay shared losses by placing funds in escrow, obtaining a surety bond, establishing a line of credit (as evidenced by a letter of credit that the Medicare program can draw upon), or establishing a combination of such repayment mechanisms, that will ensure its ability to repay the Medicare program.
(3) An ACO participating under a two-sided model must demonstrate the adequacy of this repayment mechanism prior to the start of each agreement period in which it takes risk, and upon request thereafter. After the repayment mechanism has been used to repay any portion of shared losses owed to CMS, the ACO must replenish the amount of funds available through the repayment mechanism within 60 days.
(4) The repayment mechanism must be in effect for a sufficient period of time after the conclusion of the agreement period to permit CMS to calculate the amount of shared losses owed and to collect this amount from the ACO.
(g) Consideration of claims billed under merged and acquired Medicare-enrolled TINs. An ACO may request that CMS consider, for purposes of beneficiary assignment and establishing the ACO's benchmark under § 425.602, claims billed by Medicare-enrolled entities' TINs that have been acquired through sale or merger by an ACO participant.
(1) The ACO may include an acquired Medicare-enrolled entity's TIN on its ACO participant list under the following circumstances:
(i) The ACO participant has subsumed the acquired entity's TIN in its entirety, including all of the providers and suppliers that reassigned their right to receive Medicare payment to the acquired entity's Medicare-enrolled TIN.
(ii) Each provider or supplier that previously reassigned his or her right to receive Medicare payment to the acquired entity's TIN has reassigned his or her right to receive Medicare payment to the TIN of the acquiring ACO participant and has been added to the ACO provider/supplier list under paragraph (c)(5) of the section.
(iii) The acquired entity's TIN is no longer used to bill Medicare.
(2) The ACO must submit the following supporting documentation in the form and manner specified by CMS.
(i) An attestation that—
(A) Identifies by Medicare-enrolled TIN both the acquired entity and the ACO participant that acquired it;
(B) Specifies that all the providers and suppliers that previously reassigned their right to receive Medicare payment to the acquired entity's TIN have reassigned such right to the TIN of the identified ACO participant and have been added to the ACO provider/supplier list under paragraph (c)(5) of this section; and
(C) Specifies that the acquired entity's TIN is no longer used to bill Medicare.
(ii) Documentation sufficient to demonstrate that the acquired entity's TIN was merged with or purchased by the ACO participant.
16. Amend § 425.206 by revising paragraph (a) to read as follows:
End Amendment PartStart Amendment PartEvaluation procedures for applications.(a) Basis for evaluation and determination. (1) CMS evaluates an ACO's application to determine whether an applicant satisfies the requirements of this part and is qualified to participate in the Shared Savings Program. Applications are approved or denied on the basis of the following:
(i) Information contained in and submitted with the application by a deadline specified by CMS.
(ii) Supplemental information that was submitted by a deadline specified by CMS in response to CMS' request for information.
(iii) Other information available to CMS.
(2) CMS notifies an ACO applicant when supplemental information is required for CMS to make such determination and provides an opportunity for the ACO to submit the information.
(3) CMS may deny an application if an ACO applicant fails to submit information by the deadlines established by CMS.
* * * * *17. Amend § 425.212 by revising the section heading and paragraph (a) to read as follows:
End Amendment PartStart Amendment PartChanges to program requirements during the agreement period.(a) An ACO is subject to all regulatory changes that become effective during the agreement period, with the exception of the following program areas, unless otherwise required by statute:
(1) Eligibility requirements concerning the structure and governance of ACOs.
(2) Calculation of sharing rate.
* * * * *18. Amend § 425.214 as follows:
End Amendment Part Start Amendment PartA. By revising the section heading.
End Amendment Part Start Amendment PartB. By removing paragraph (a).
End Amendment Part Start Amendment PartC. By redesignating paragraphs (b) and (c) as paragraphs (a) and (b), respectively.
End Amendment Part Start Amendment PartD. By revising newly redesignated paragraph (a).
End Amendment Part Start Amendment PartE. In newly redesignated paragraph (b) introductory text, removing the phrase “Upon receiving” and adding in its place the phrase “Upon becoming aware of a significant change or receiving”.
End Amendment Part Start Amendment PartF. In newly redesignated paragraphs (b)(2) and (4) by removing the term “agreement” and adding in its place the terms “participation agreement”.
End Amendment PartThe revisions read as follows:
Managing changes to the ACO during the agreement period.(a)(1) An ACO must notify CMS within 30 days of any significant change.
(2) An ACO's failure to notify CMS of a significant change shall not preclude CMS from determining that the ACO has experienced a significant change.
(3) A “significant change” occurs when —
(i) An ACO is no longer able to meet the eligibility or program requirements of this part; orStart Printed Page 72867
(ii) The number or identity of the ACO participants on the ACO's list of ACO participants has changed by 50 percent or more.
* * * * *Start Amendment Part[Amended]19. Amend § 425.216 in paragraph (b) by removing the term “ACO's agreement” and adding in its place the terms “participation agreement”.
End Amendment Part Start Amendment Part20. Amend § 425.218 by revising the section heading and adding paragraphs (b)(4) and (5) to read as follows:
End Amendment PartTermination of the participation agreement by CMS.* * * * *(b) * * *
(4) Failure to comply with CMS requests for documentation or other information by the deadline specified by CMS.
(5) Submitting false or fraudulent data or information.
* * * * *Start Amendment Part[Amended]21. Amend § 425.220 by removing and reserving paragraph (b).
End Amendment Part Start Amendment Part22. Add § 425.221 to read as follows:
End Amendment PartStart Amendment PartClose-out procedures and payment consequences of early termination.(a) Close-out procedures. (1) An ACO whose participation agreement has expired or is terminated by CMS under § 425.218 or by the ACO under § 425.220 must implement close-out procedures regarding the following in a form and manner and by a deadline specified by CMS:
(i) Notice to ACO participants of termination.
(ii) Record retention.
(iii) Data sharing.
(iv) Quality reporting.
(v) Beneficiary continuity of care
(vi) Other relevant operational matters established through guidance.
(2) ACOs that fail to complete close-out procedures in the form and manner and by the deadline specified by CMS will not be eligible to share in savings.
(b) Payment consequences of early termination. (1) An ACO whose participation agreement is terminated by the ACO under § 425.220 is eligible to receive shared savings for the performance year during which the termination becomes effective only if—
(i) CMS designates or approves an effective date of termination of December 31st of such performance year;
(ii) The ACO has completed all close-out procedures by the deadline specified by CMS; and
(iii) The ACO has satisfied the criteria for sharing in savings for the performance year.
(2) An ACO that terminates its participation agreement under § 425.220 before December 31 of a performance year or whose participation agreement is terminated by CMS under § 425.218 at any time is not eligible to receive shared savings for the performance year during which the termination becomes effective.
23. Amend § 425.222 by revising paragraph (c) to read as follows:
End Amendment PartStart Amendment PartReapplication after termination.* * * * *(c) An ACO whose participation agreement was previously terminated may reenter the program under a subsequent agreement period.
(1) If the termination occurred less than half way through the agreement period, an ACO that was previously under a one-sided model may reenter the program under the one-sided model or a two-sided model. If the ACO reenters the program under the one-sided model, the ACO will be considered to be in its first agreement period under the one-sided model.
(2) If the termination occurred more than half way through the agreement period, an ACO that was previously under a one-sided model may reenter the program under the one-sided model or a two-sided model. If the ACO reenters the program under the one-sided model, the ACO will be considered to be in its second agreement period under the one-sided model.
(3) Regardless of the date of termination, an ACO that was previously under a two-sided model may only reapply for participation in a two-sided model.
24. Add § 425.224 to subpart C to read as follows:
End Amendment PartRenewal of participation agreements.(a) General rules. An ACO may request renewal of its participation agreement for a second or subsequent agreement period.
(1) In order to obtain a determination regarding whether it meets the requirements for renewal of its participation agreement, the ACO must submit a complete renewal request in the form and manner and by the deadline specified by CMS.
(2) An ACO executive who has the authority to legally bind the ACO must certify to the best of his or her knowledge, information, and belief that the information contained in the renewal request is accurate, complete, and truthful.
(3) An ACO that seeks renewal of its participation agreement and was newly formed after March 23, 2010, as defined in the Antitrust Policy Statement, must agree that CMS can share a copy of its renewal request with the Antitrust Agencies.
(b) Review of renewal request. (1) CMS determines whether to renew a participation agreement based on an evaluation of all of the following factors:
(i) Whether the ACO satisfies the criteria for operating under the selected risk track.
(ii) The ACO's history of compliance with the requirements of the Shared Savings Program.
(iii) Whether the ACO has established that it is in compliance with the eligibility and other requirements of the Shared Savings Program, including the ability to repay losses, if applicable.
(iv) Whether the ACO met the quality performance standard during at least one of the first 2 years of the previous agreement period.
(v) For ACOs under a two-sided model, whether the ACO has repaid losses owed to the program that it generated during the first 2 years of the previous agreement period.
(vi) The results of a program integrity screening of the ACO, its ACO participants, and its ACO providers/suppliers (conducted in accordance with § 425.304(b)).
(2) Renewal requests are approved or denied on the basis of the following information:
(i) Information contained in and submitted with the renewal request by a deadline specified by CMS.
(ii) Supplemental information that was submitted by a deadline specified by CMS in response to CMS' request for information.
(iii) Other information available to CMS.
(3) CMS notifies the ACO when supplemental information is required for CMS to make such a determination and provides an opportunity for the ACO to submit the information.
(c) Notice of determination. (1) CMS notifies in writing each ACO of its determination to approve or deny the ACO's renewal request.
(2) If CMS denies the renewal request, the notice of determination—
(i) Specifies the reasons for the denial; and
(ii) Informs the ACO of its right to request reconsideration review in accordance with the procedures specified in subpart I of this part.
Start Amendment Part[Amended]25. Amend § 425.304 by removing paragraph (d). Start Printed Page 72868
End Amendment Part Start Amendment Part26. Revise § 425.306 to read as follows:
End Amendment PartStart Amendment PartParticipant agreement and exclusivity of ACO participants.(a) Each ACO participant must commit to the term of the participation agreement and sign an ACO participant agreement that complies with the requirements of this part.
(b)(1) Except as specified in paragraph (b)(2) of this section, ACO participants are not required to be exclusive to one Shared Savings Program ACO.
(2) Each ACO participant that submits claims for primary care services used to determine the ACO's assigned population under subpart E of this part must be exclusive to one Shared Savings Program ACO.
27. Revise § 425.308 to read as follows:
End Amendment PartStart Amendment PartPublic reporting and transparency.(a) ACO public reporting Web page. Each ACO must create and maintain a dedicated Web page on which it publicly reports the information set forth in paragraph (b) of this section. The ACO must report the address of such Web page to CMS in a form and manner specified by CMS and must notify CMS of changes to the Web address in the form and manner specified by CMS.
(b) Information to be reported. The ACO must report the following information in a standardized format specified by CMS:
(1) Name and location.
(2) Primary contact.
(3) Organizational information, including all of the following:
(i) Identification of ACO participants.
(ii) Identification of participants in joint ventures between ACO professionals and hospitals.
(iii) Identification of the members of its governing body.
(iv) Identification of key clinical and administrative leadership.
(v) Identification of associated committees and committee leadership.
(vi) Identification of the types of ACO participants or combinations of ACO participants (as listed in § 425.102(a)) that formed the ACO.
(4) Shared savings and losses information, including the following:
(i) Amount of any payment of shared savings received by the ACO or shared losses owed to CMS.
(ii) Total proportion of shared savings invested in infrastructure, redesigned care processes and other resources required to support the three-part aim goals of better health for populations, better care for individuals and lower growth in expenditures, including the proportion distributed among ACO participants.
(5) The ACO's performance on all quality measures.
(c) Approval of public reporting information. Information reported on an ACO's public reporting Web page in compliance with the requirements of the standardized format specified by CMS is not subject to marketing review and approval under § 425.310.
(d) Public reporting by CMS. CMS may publicly report ACO-specific information, including but not limited to the ACO public reporting Web page address and the information required to be publicly reported under paragraph (b) of this section.
28. Amend § 425.312 by removing and reserving paragraph (b) and revising paragraph (a) to read as follows:
End Amendment PartNotification to beneficiaries of participation in the shared savings program.(a) ACO participants must notify beneficiaries at the point of care that their ACO providers/suppliers are participating in the Shared Savings Program and of the opportunity to decline claims data sharing under § 425.708.
(1) Notification is carried out when an ACO participant posts signs in its facilities and, in settings in which beneficiaries receive primary care services, by making standardized written notices available upon request.
(2) The ACO must use template language developed by CMS for notifications described in paragraph (a)(1) of this section.
* * * * *Start Amendment Part[Amended]29. Amend § 425.314 in paragraph (c) by removing the word “agreement” and adding in its place the words “participation agreement”.
End Amendment PartStart Amendment Part[Amended]30. Amend § 425.316 as follows:
End Amendment Part Start Amendment PartA. By removing paragraphs (c)(3) and (4).
End Amendment Part Start Amendment PartB. By redesignating paragraph (c)(5) as (c)(3).
End Amendment Part Start Amendment PartC. In newly redesignated paragraph (c)(3) by removing the phrase “fully and completely” and adding in its place the phrase “accurately, completely, and timely”.
End Amendment Part Start Amendment Part31. Amend § 425.400 as follows:
End Amendment Part Start Amendment PartA. By adding paragraph (a)(1) introductory text.
End Amendment Part Start Amendment PartB. By revising paragraph (a)(1)(i).
End Amendment Part Start Amendment PartC. In paragraph (a)(1)(ii), by removing the phrase “by a physician who is an ACO provider/supplier during the performance year” and adding in its place the phrase “by a physician who is an ACO professional during each benchmarking year and during each performance year”.
End Amendment Part Start Amendment PartD. By adding a subject heading to paragraph (a)(2).
End Amendment Part Start Amendment PartE. By adding paragraph (a)(3).
End Amendment PartThe additions read as follows:
Start Amendment PartGeneral.(a)(1) General. (i) A Medicare fee-for-service beneficiary is assigned to an ACO for a performance year if the—
(A) Beneficiary meets the eligibility criteria under § 425.401(a); and
(B) Beneficiary's utilization of primary care services meets the criteria established under the assignment methodology described in § 425.402 and § 425.404.
* * * * *(2) Assignment under Tracks 1 and 2.
* * * * *(3) Prospective assignment under Track 3. (i) Medicare fee-for-service beneficiaries are prospectively assigned to an ACO under Track 3 at the beginning of each performance year based on the beneficiary's use of primary care services in the most recent 12 months for which data are available, using the assignment methodology described in § 425.402 and § 425.404.
(ii) Beneficiaries that are prospectively assigned to an ACO under paragraph (a)(3)(i) of this section will remain assigned to the ACO at the end of the performance year unless they meet any of the exclusion criteria under § 425.401(b).
* * * * *32. Add § 425.401 to read as follows:
End Amendment PartStart Amendment PartCriteria for a beneficiary to be assigned to an ACO.(a) A beneficiary may be assigned to an ACO under the assignment methodology in §§ 425.402 and 425.404, for a performance or benchmark year, if the beneficiary meets all of the following criteria during the assignment window:
(1)(i) Has at least 1 month of Part A and Part B enrollment; and
(ii) Does not have any months of Part A only or Part B only enrollment.
(2) Does not have any months of Medicare group (private) health plan enrollment.
(3) Is not assigned to any other Medicare shared savings initiative.
(4) Lives in the United States or U.S. territories and possessions, based on the most recent available data in our beneficiary records regarding the beneficiary's residence at the end of the assignment window.
(b) A beneficiary will be excluded from the prospective assignment list of Start Printed Page 72869an ACO participating under Track 3 at the end of a performance or benchmark year, if the beneficiary meets any of the following criteria during the performance or benchmark year:
(1)(i) Does not have at least 1 month of Part A and Part B enrollment; and
(ii) Has any months of Part A only or Part B only enrollment.
(2) Has any months of Medicare group (private) health plan enrollment.
(3) Did not live in the United States or U.S. territories and possessions, based on the most recent available data in our beneficiary records regarding the beneficiary's residency at the end of the year.
33. Revise § 425.402 to read as follows:
End Amendment PartStart Amendment PartBasic assignment methodology.(a) For purposes of benchmarking, preliminary prospective assignment (including quarterly updates) and retrospective reconciliation, and prospective assignment, CMS employs the following step-wise methodology to assign Medicare fee-for-service beneficiaries to an ACO:
(1) Identify all beneficiaries that had at least one primary care service with a physician who is an ACO professional in the ACO and who is a primary care physician as defined under § 425.20 or who has one of the primary specialty designations included in paragraph (b) of this section.
(2) Identify all primary care services furnished to beneficiaries identified in paragraph (a)(1) by ACO professionals of that ACO who are primary care physicians as defined under § 425.20, non-physician ACO professionals, and physicians with specialty designations included in paragraph (b) of this section during the applicable assignment window.
(3) Under the first step, a beneficiary identified in paragraph (a)(1) of this section is assigned to an ACO if the allowed charges for primary care services furnished to the beneficiary by primary care physicians who are ACO professionals and non-physician ACO professionals in the ACO are greater than the allowed charges for primary care services furnished by primary care physicians, nurse practitioners, physician assistants, and clinical nurse specialists who are—
(i) ACO professionals in any other ACO; or
(ii) Not affiliated with any ACO and identified by a Medicare-enrolled billing TIN.
(4) The second step considers the remainder of the beneficiaries identified in paragraph (a)(1) of this section who have not had a primary care service rendered by any primary care physician, nurse practitioner, physician assistant, or clinical nurse specialist, either inside the ACO or outside the ACO. The beneficiary will be assigned to an ACO if the allowed charges for primary care services furnished to the beneficiary by physicians who are ACO professionals with specialty designations as specified in paragraph (b) of this section are greater than the allowed charges for primary care services furnished by physicians with specialty designations as specified in paragraph (b) of this section—
(i) Who are ACO professionals in any other ACO; or
(ii) Who are unaffiliated with an ACO and are identified by a Medicare-enrolled billing TIN.
(b) ACO professionals considered in the second step of the assignment methodology in paragraph (a)(4) of this section include physicians who have one of the following primary specialty designations:
(1) Allergy/immunology.
(2) Cardiology.
(3) Gastroenterology.
(4) Neurology.
(5) Obstetrics/gynecology.
(6) Hospice and palliative care.
(7) Sports medicine.
(8) Physical medicine and rehabilitation.
(9) Pulmonary disease.
(10) Pediatric medicine.
(11) Nephrology.
(12) Infectious disease.
(13) Endocrinology.
(14) Rheumatology.
(15) Multispecialty clinic or group practice.
(16) Hematology.
(17) Hematology/oncology.
(18) Preventive medicine.
(19) Medical oncology.
(20) Gynecology/oncology.
(c) When considering services furnished by ACO professionals in teaching hospitals that have elected under § 415.160 to receive payment on a reasonable cost basis for the direct medical and surgical services of their physicians in the assignment methodology under paragraph (a) of this section, CMS uses the amount payable under the physician fee schedule for the specified HCPCS code as a proxy for the amount of the allowed charges for the service.
34. Amend § 425.404 by revising paragraph (b) to read as follows:
End Amendment PartStart Amendment PartSpecial assignment conditions for ACOs including FQHCs and RHCs.* * * * *(b) Under the assignment methodology in § 425.402, CMS treats a service reported on an FQHC/RHC claim as—
(1) A primary care service if the claim includes a HCPCS or revenue center code that meets the definition of primary care services under § 425.20;
(2) A primary care service performed by a primary care physician if the NPI of a physician identified in the attestation provided under paragraph (a) of this section is reported on the claim for a primary care service (as described in paragraph (b)(1) of this section) as the attending provider; and
(3) A primary care service performed by a non-physician ACO professional if the NPI reported on the claim for a primary care service (as described in paragraph (b)(1) of this section) as the attending provider is an ACO professional but is not identified in the attestation provided under paragraph (a) of this section.
36. Amend § 425.600 as follows:
End Amendment Part Start Amendment PartA. In paragraph (a)(2), by removing the phrase “under the two-sided model” and adding in its place the phrase “under a two-sided model”.
End Amendment Part Start Amendment PartB. By adding paragraph (a)(3).
End Amendment Part Start Amendment PartC. By revising paragraph (b).
End Amendment PartThe addition and revision read as follows:
Selection of risk model.(a) * * *
(3) Track 3. Under Track 3, the ACO operates under a two-sided model (as described under § 425.610), sharing both savings and losses with the Medicare program for the agreement period.
(b) An ACO may not operate under the one-sided model for a second agreement period unless the—
(1) Immediately preceding agreement period was under the one-sided model;
(2) The ACO did not generate losses in excess of its negative MSR in both of the first 2 performance years of the previous agreement period; and
(3) The ACO meets the criteria established for ACOs seeking to renew their agreements under § 425.224(b).
* * * * *Start Amendment Part[Amended]37. Amend § 425.602 (a)(8), by removing the phrase “The ACO's benchmark may be adjusted” and adding in its place the phrase “The ACO's benchmark will be adjusted in accordance with § 425.118(b)”.
End Amendment Part Start Amendment Part38. Amend § 425.604 as follows:
End Amendment Part Start Amendment PartA. By redesignating the text of paragraph (d) as paragraph (d)(1).
End Amendment Part Start Amendment PartB. In newly redesignated paragraph (d)(1), removing the phrase “under the one-sided model” and adding in its place the phrase “during a performance year in its first agreement period under the one-sided model”.Start Printed Page 72870
End Amendment Part Start Amendment PartD. By adding a paragraph (d)(2).
End Amendment PartThe addition reads as follows:
Start Amendment PartCalculation of savings under the one-sided model.* * * * *(d) * * *
(2) An ACO that meets all the requirements for receiving shared savings payments during a performance year in its second agreement period under the one-sided model will receive a shared savings payment of up to 40 percent of all savings under the updated benchmark, as determined on the basis of its quality performance under § 425.502 (up to the performance payment limit described in paragraph (e)(2) of this section).
* * * * *39. Amend § 425.606 as follows:
End Amendment Part Start Amendment PartA. By revising the section heading.
End Amendment Part Start Amendment PartB. In paragraph (a) introductory text, by removing the phrase “under the two-sided model,” and adding in its place the phrase “under Track 2,”.
End Amendment Part Start Amendment PartC. By revising paragraph (b).
End Amendment Part Start Amendment PartD. In paragraph (d), by removing the phrase “under the two-sided model” and adding in its place the phrase “under Track 2”.
End Amendment Part Start Amendment PartE. In paragraph (e)(2), by removing the phrase “under the two-sided model” and adding in its place the phrase “under Track 2”.
End Amendment Part Start Amendment PartF. In paragraph (g)(1), by removing the phrase “in a two-sided model” and adding in its place the phrase “in Track 2”.
End Amendment PartThe revisions read as follows:
Start Amendment PartCalculation of shared savings and losses under Track 2.* * * * *(b) Minimum savings or loss rate. CMS uses a sliding scale, based on the number of beneficiaries assigned to the ACO under subpart E of this part, to establish the MSR and MLR for an ACO participating under Track 2. The MSR under Track 2 is the same as the MSR that would apply in the one-sided model under § 425.604(b) and is based on the number of assigned beneficiaries. The MLR under Track 2 is equal to the negative MSR.
(1) To qualify for shared savings under Track 2, an ACO's average per capita Medicare expenditures for the performance year must be below its updated benchmark costs for the year by at least the MSR established for the ACO.
(2) To be responsible for sharing losses with the Medicare program, an ACO's average per capita Medicare expenditures for the performance year must be above its updated benchmark costs for the year by at least the MLR established for the ACO.
* * * * *40. Add § 425.610 to subpart G to read as follows:
End Amendment PartStart Amendment PartCalculation of shared savings and losses under Track 3.(a) General rule. For each performance year, CMS determines whether the estimated average per capita Medicare expenditures under the ACO for Medicare fee-for-service beneficiaries for Parts A and B services are above or below the updated benchmark determined under § 425.602. In order to qualify for a shared savings payment under Track 3, or to be responsible for sharing losses with CMS, an ACO's average per capita Medicare expenditures under the ACO for Medicare fee-for-service beneficiaries for Parts A and B services for the performance year must be below or above the updated benchmark, respectively, by at least the minimum savings or loss rate under paragraph (b) of this section.
(1) Newly assigned beneficiaries. CMS uses an ACO's HCC prospective risk score to adjust for changes in severity and case mix in this population.
(2) Continuously assigned beneficiaries. (i) CMS uses demographic factors to adjust for changes in the continuously assigned beneficiary population.
(ii) If the prospective HCC risk score is lower in the performance year for this population, CMS adjusts for changes in severity and case mix for this population using this lower prospective HCC risk score.
(3) Assigned beneficiary changes in demographics and health status are used to adjust benchmark expenditures as described in § 425.602(a). In adjusting for health status and demographic changes CMS makes separate adjustments for each of the following populations of beneficiaries:
(i) ESRD.
(ii) Disabled.
(iii) Aged/dual eligible Medicare and Medicaid beneficiaries.
(iv) Aged/non-dual eligible Medicare and Medicaid beneficiaries.
(4) To minimize variation from catastrophically large claims, CMS truncates an assigned beneficiary's total annual Parts A and B fee-for-service per capita expenditures at the 99th percentile of national Medicare fee-for-service expenditures as determined for each performance year.
(5) CMS uses a 3-month claims run out with a completion factor to calculate an ACO's per capita expenditures for each performance year.
(6) Calculations of the ACO's expenditures will include the payment amounts included in Part A and B fee-for-service claims.
(i) These calculations will exclude indirect medical education (IME) and disproportionate share hospital (DSH) payments.
(ii) These calculations will take into consideration individually beneficiary identifiable payments made under a demonstration, pilot or time limited program.
(7) In order to qualify for a shared savings payment, the ACO's average per capita Medicare expenditures for the performance year must be below the applicable updated benchmark by at least the minimum savings rate established for the ACO under paragraph (b) of this section.
(b) Minimum savings or loss rate. (1) To qualify for shared savings under Track 3 an ACO's average per capita Medicare expenditures for the performance year must be below its updated benchmark costs for the year by at least 2 percent.
(2) To be responsible for sharing losses with the Medicare program under Track 3, an ACO's average per capita Medicare expenditures for the performance year must be at least 2 percent above its updated benchmark costs for the year.
(c) Qualification for shared savings payment. To qualify for shared savings, an ACO must meet the minimum savings rate requirement established under paragraph (b) of this section, meet the minimum quality performance standards established under § 425.502, and otherwise maintain its eligibility to participate in the Shared Savings Program under this part.
(d) Final sharing rate. An ACO that meets all the requirements for receiving shared savings payments under Track 3 will receive a shared savings payment of up to 75 percent of all the savings under the updated benchmark, as determined on the basis of its quality performance under § 425.502 (up to the performance payment limit described in paragraph (e)(2) of this section).
(e) Performance payment. (1) If an ACO qualifies for savings by meeting or exceeding the MSR, the final sharing rate will apply to an ACO's savings on a first dollar basis.
(2) The amount of shared savings an eligible ACO receives under Track 3 may not exceed 20 percent of its updated benchmark.
(f) Shared loss rate. The shared loss rate—
(1) For an ACO that is required to share losses with the Medicare program for expenditures over the updated Start Printed Page 72871benchmark, the amount of shared losses is determined based on the inverse of its final sharing rate described in § 425.610(d) (that is, 1 minus the final shared savings rate determined under § 425.610(d));
(2) May not exceed 75 percent; and
(3) May not be less than 40 percent.
(g) Loss recoupment limit. The amount of shared losses for which an eligible ACO is liable may not exceed 15 percent of its updated benchmark as determined under § 425.602.
(h) Notification of savings and losses. (1) CMS notifies an ACO in writing regarding whether the ACO qualifies for a shared savings payment, and if so, the amount of the payment due.
(2) CMS provides written notification to an ACO of the amount of shared losses, if any, that it must repay to the program.
(3) If an ACO has shared losses, the ACO must make payment in full to CMS within 90 days of receipt of notification.
41. Amend § 425.702 by revising paragraph (c)(1) to read as follows:
End Amendment PartStart Amendment PartAggregate reports.* * * * *(c) * * *
(1) At the beginning of the agreement period, during each quarter (and in conjunction with the annual reconciliation), and at the beginning of each performance year, CMS, upon the ACO's request for the data for purposes of population-based activities relating to improving health or reducing growth in health care costs, process development, care management, and care coordination, will provide the ACO with information about its fee-for-service population.
(i) Under Tracks 1 and 2, the following information is made available regarding preliminarily prospectively assigned beneficiaries and beneficiaries that received a primary care service during the previous 12 months from one of the ACO participants that submits claims for primary care services used to determine the ACO's assigned population under subpart E of this part:
(A) Beneficiary name.
(B) Date of birth.
(C) Health Insurance Claim Number (HICN).
(D) Sex.
(ii) Under Tracks 1 and 2, information in the following categories, which represents the minimum data necessary for ACOs to conduct health care operations work is made available regarding preliminarily prospectively assigned beneficiaries:
(A) Demographic data such as enrollment status.
(B) Health status information such as risk profile and chronic condition subgroup.
(C) Utilization rates of Medicare services such as the use of evaluation and management, hospital, emergency, and post-acute services, including the dates and place of service.
(D) Expenditure information related to utilization of services.
(iii) The information under paragraphs (c)(1)(i) and (c)(1)(ii) of this section will be made available to ACOs in Track 3, but will be limited to the ACO's prospectively assigned beneficiaries.
* * * * *42. Amend § 425.704 as follows:
End Amendment Part Start Amendment PartA. By revising the section heading.
End Amendment Part Start Amendment PartB. In the introductory text, by removing the phrase “claims data for preliminary prospectively assigned beneficiaries” and adding in its place the phrase “claims data for preliminarily prospectively and prospectively assigned beneficiaries”.
End Amendment Part Start Amendment PartC. In the introductory text, by removing the phrase “upon whom assignment is based during the agreement period” and adding in its place the phrase “that submits claims for primary care services used to determine the ACO's assigned population under subpart E of this part during the performance year”.
End Amendment Part Start Amendment PartD. In paragraph (a) by removing the phrase “ACOs may request data as often” and adding in its place “ACOs may access requested data as often”.
End Amendment Part Start Amendment PartE. By revising paragraph (d)(1).
End Amendment Part Start Amendment PartF. In paragraph (d)(2) by removing the phrase “has been notified in writing how the ACO intends to use” and adding in its place the phrase “has been notified in compliance with § 425.708 that the ACO has requested access to”.
End Amendment PartThe revisions read as follows:
Start Amendment PartBeneficiary-identifiable claims data.* * * * *(d) * * *
(1) For an ACO participating—
(i) In Track 1 or 2, the beneficiary's name appears on the preliminary prospective assignment list provided to the ACO at the beginning of the performance year, during each quarter (and in conjunction with the annual reconciliation) or the beneficiary has received a primary care service from an ACO participant upon whom assignment is based (under subpart E of this part) during the most recent 12-month period.
(ii) In Track 3, the beneficiary's name appears on the prospective assignment list provided to the ACO at the beginning of the performance year.
* * * * *43. Amend § 425.708 as follows:
End Amendment Part Start Amendment PartA. Revising the section heading and paragraph (a).
End Amendment Part Start Amendment PartB. Removing paragraphs (b) and (c).
End Amendment Part Start Amendment PartC. Redesignating paragraphs (d) through (f) as paragraphs (b) through (d), respectively.
End Amendment Part Start Amendment PartD. Revising newly redesignated paragraphs (b) and (c).
End Amendment PartThe revisions read as follows:
Start Amendment PartBeneficiaries may decline claims data sharing.(a) Beneficiaries must receive notification about the Shared Savings Program and the opportunity to decline claims data sharing and instructions on how to inform CMS directly of their preference.
(1) FFS beneficiaries are notified about the opportunity to decline claims data sharing through CMS materials such as the Medicare & You Handbook and through the notifications required under § 425.312.
(2) The notifications provided under § 425.312 must state that the ACO may have requested beneficiary identifiable claims data about the beneficiary for purposes of its care coordination and quality improvement work, and inform the beneficiary how to decline having his or her claims information shared with the ACO in the form and manner specified by CMS.
(3) Beneficiary requests to decline claims data sharing will remain in effect unless and until a beneficiary subsequently contacts CMS to amend that request to permit claims data sharing with ACOs.
(b) The opportunity to decline having claims data shared with an ACO under paragraph (a) of this section does not apply to the information that CMS provides to ACOs under § 425.702(c).
(c) In accordance with 42 U.S.C. 290dd-2 and the implementing regulations at 42 CFR part 2, CMS does not share beneficiary identifiable claims data relating to the diagnosis and treatment of alcohol and substance abuse without the explicit written consent of the beneficiary.
* * * * *44. Amend § 425.802 by revising paragraph (a)(2) to read as follows:
End Amendment PartStart Amendment PartRequest for review.(a) * * *
(2) The reconsideration review must be held on the record (review of submitted documentation).
* * * * *45. Amend § 425.804 as follows:
End Amendment Part Start Amendment PartA. By revising paragraph (a)(3).Start Printed Page 72872
End Amendment Part Start Amendment PartB. By removing paragraph (d).
End Amendment Part Start Amendment PartC. Redesignating paragraphs (e) and (f) as paragraphs (d) and (e), respectively.
End Amendment PartThe revision reads as follows:
Start SignatureReconsideration review process.(a) * * *
(3) A briefing schedule that permits each party to submit only one written brief, including any evidence, for consideration by the reconsideration official in support of the party's position.
* * * * *End Signature End Supplemental InformationDated: November 20, 2014.
Marilyn Tavenner,
Administrator, Centers for Medicare & Medicaid Services.
Dated: November 21, 2014.
Sylvia M. Burwell,
Secretary, Department of Health and Human Services.
[FR Doc. 2014-28388 Filed 12-1-14; 4:15 pm]
BILLING CODE 4120-01-P
Document Information
- Published:
- 12/08/2014
- Department:
- Centers for Medicare & Medicaid Services
- Entry Type:
- Proposed Rule
- Action:
- Proposed rule.
- Document Number:
- 2014-28388
- Dates:
- To be assured consideration, comments must be received at one of
- Pages:
- 72759-72872 (114 pages)
- Docket Numbers:
- CMS-1461-P
- RINs:
- 0938-AS06: Medicare Shared Savings Program; Accountable Care Organizations (CMS-1461-P)
- RIN Links:
- https://www.federalregister.gov/regulations/0938-AS06/medicare-shared-savings-program-accountable-care-organizations-cms-1461-p-
- Topics:
- Administrative practice and procedure, Health facilities, Health professions, Medicare, Reporting and recordkeeping requirements
- PDF File:
- 2014-28388.pdf
- CFR: (43)
- 42 CFR 425.10
- 42 CFR 425.20
- 42 CFR 425.100
- 42 CFR 425.102
- 42 CFR 425.104
- More ...